
PTA103Pulmonary Conditions2019
PTA 103 Intro to Clinical Practice 2
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.

Understanding function of the pulmonary system is essential for safe and effective exercise selection and planning.
Pulmonary dysfunction is encountered acidosis the life span and is significantly influenced by environmental and personal factors. Regardless of age, decreased breathing efficiency and effectiveness results in decreased activity tolerance and can limit full participation in work, home, and school activities.
Although industrial safety standards have improved and tobacco use is declining, there are several generations of clientele with decreased lung function as a result of one or often both of these exposure points.
Optimal care and safe discharge planning often involves close coordination with nursing, Respiratory Care, and family. Treatment progression and discharge planning may include the use of supportive equipment, such as breathing apparatus and supplemental O2 , instruction therapeutic positioning and postural control, breathing reeducation, and progressive reconditioning
Smoking decreases overall health, with primary effects on the cardiopulmonary system. In addition to implementing the PT plan of care, PTAs are also health advocates and communicate effectively with patients in health promotion and disease prevention.
This Quit Smoking Campaign video notes explicit vascular compromise in a deceased smoker. Effective education and outreach can change a life.

One challenge with this unit is in how text book material is organized. Cameron follows the Guide to Physical Therapy Practice, so its chapters are based on specific practice patterns. Cameron and Pagliarulo provide excellent, comprehensive information on physical therapy uses knowledge of anatomy, physiology and pathophysiology to restore optimal function with safe and effective clinical and home exercise instruction. Specific sections of each chapter are included in the respective "Reading Assignments". In order to keep the amount of reading relevant and less redundant, be sure you complete your readings in the suggested order as you go through the lecture.
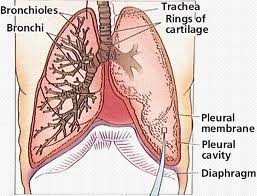
The anatomy of the respiratory system will be a review of content from your A&P coursework and Pagliarulo from fall term.
Breathing is an automatic action coordinated by the nervous system, the musculoskeletal system, and the anatomical structures that comprise the airways. Impairments that arise when their are dysfunctions within one or more of these systems can result in decreased endurance, decreased strength, postural abnormalities, and impaired airway clearance. When respiration or ventilation is impaired, a patient will work to generate compensatory strategies to maintain breathing function.
Why is an understanding of anatomy critical to optimizing ventilation and respiration? As we move forward in the lecture, we will be connecting anatomy and physiology to the basis for the interventions. For example, positioning for postural drainage requires that a PTA can integrate knowledge of lung lobes and respective airways and gravity to passively improve airway clearance, and therefore decrease muscular efforts and improve gas exchange. Although breathing is largely under autonomic control, PTs and PTAs take advantage of volitional breathing patterns and pathways to help patients and clients optimize respiration and ventilation.
As you refresh your knowledge of anatomy and breathing mechanics, start thinking about how each structure, such as the rib cage, intercostals, and respiratory zones play an essential role in breathing:
Respiration: "Respiration is the process of exchange of gases between the atmosphere and the tissues"
Ventilation: "Ventilation refers to the movement of a volume of air from the atmosphere in and out of the airways and is highly dependent on the ability of the respiratory muscles to generate force to bring air into the lungs"
Note the number of medical diagnoses (Cameron & Monroe, Box 26-1) that are associated with breathing impairments. In addition to COPD, neuromuscular disorders, infections, and musculoskeletal conditions, such as scoliosis, can present with breathing impairments as a primary contributor to disability. Can you see why a strong foundation of anatomy, physiology, and pathophysiology can improve patient outcomes in airway clearance, posture, and endurance?
The take home message for PTs/PTAs is that abnormal level of O2 and CO2 trigger a change in respiration rate, effort, efficiency, perfusion, and overall function.
Lung volumes during different phases of breathing are used to assess the effects of pathology on ventilation. Remember, ventilation is the volume of air that moves in and out of the airways. PTs and PTAs teach patients interventions that aim to increase air in and improve the force by which air flows out, therefore foundational knowledge in pulmonary function measures provides some insight into the major barriers to ventilation (e.g. restrictive versus obstructive) and how lung volume measures compare to normal values. Measuring pulmonary function is accomplished through spirometry and is typically performed by Respiratory Care.
Shortness of breath is a sign that ventilation is insufficient to meet the oxygen demands of the activity. This can present at rest with advanced lung disease, and after exertion during mild to high intensity exercise and activity. In patients with pulmonary impairments, breathing rate is closely monitored as an indicator of exercise intensity and tolerance. Shortness of breath is one of the indicators of Work of Breathing (WOB).
Airway tissue resistance, elasticity, and compliance are major factors in respiration. PTs and PTAs apply knowledge of respiratory muscle function, posture, and breathing mechanics to optimize pressures for inspiration and exhalation, which can result in improved gas exchange. The video below provides a brief, yet thorough explanation of pulmonary function measures. You should be able to identify the variables in calculating:
Active Learning Exercise
As you view the video below, try how you can volitionally assess your own inspiratory capacity and your expiratory reserve. What muscles are you engaging to maximally inhale and maximally exhale?
Critical thinking question: Why do interventions to increase inspiratory capacity positively affect ventilation and respiration? Try your answers in the CAN YOU HELP ME? forum.
![]()
![]()
![]()

Freitas, E. R., Soares, B. G., Cardoso, J. R., & Atallah, Á. N. (2012, September). Incentive spirometry for preventing pulmonary complications after coronary artery bypass graft. Cochrane Database of Systematic Reviews (9). doi 10.1002/14651858.CD004466.pub3.
Restrepo, R. D., Wettstein, R., Wittnebel, L., & Tracy, M. (2011). Incentive spirometry: 2011. Respiratory care, 56(10), 1600-1604.
Breathing pattern is documented in terms of rate, regularity, and location
|
Normal Rate (Adults) |
Inspiration:Expiration (Normal) |
Inhalation:Expiration (Obstructive) |
|
12-20/min > 20/min is tachypnea <12 is bradypnea |
1:2 |
1:4 |
Apnea - cessation of expiration; no airflow in or out of lungs. May be voluntary or involuntary. Prolonged apnea results in CO2 accumulation and triggers a healthy nervous system to increase arousal and breathing.
Tachypnea - shallow and rapid breathing, often present at rest with pulmonary and systemic infection
Bradypnea - shallow and slow breathing, present in coma, increased intracranial pressure
Dyspnea - labored breathing, shortness of breath
Orthopnea - difficulty breathing in supine; often experienced with obesity and lung disease
Hyperventilation - rapid and deep breathing, triggered by increased CO2 ; also associated with pain, anxiety, asthma/obstructive lung disease, heart failure; Associated symptoms include dizziness, distal muscle cramping, weakness, syncope
Cyanosis - bluish appearance in nail beds or lips; sign of inadequate ventilation and perfusion

Image of cyanosis
Retrieved from https://commons.wikimedia.org/wiki/File:Blue_finger_tips_3.jpg
Shallow, deep, rapid, irregular, asymmetric are all qualitative observational terms to describe breathing patterns.
Breathing motion is assessed by palpation of the thoracic at upper, mid, and regions; motion is also assessed holistically based on the overall automatic pattern. Accessory muscle palpation provides qualitative information about muscle tone and activation during breathing at rest.

By Jprealini (Own work) [GFDL (http://www.gnu.org/copyleft/fdl.html) or CC BY-SA 4.0-3.0-2.5-2.0-1.0 (http://creativecommons.org/licenses/by-sa/4.0-3.0-2.5-2.0-1.0)], via Wikimedia Commons

By Cchavoin (Own work) [CC BY-SA 4.0 (http://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
Observation include noting the use of supplemental oxygen and flow rate or other devices to support breathing function during activity
Pulse oximetry measures oxygen saturation and is used to guide activity intensity and inform responsiveness of interventions to improve gas exchange. Normal values are 95%-100% (Cameron & Monroe, 2011).
![]()
An excellent resource to explore breath sounds.
![]()
PTs and PTAs use standardized assessment to monitor response to exercise. Common standardized assessments used in this population include:
Wipf, J. E., Lipsky, B. A., Hirschmann, J. V., Boyko, E. J., Takasugi, J., Peugeot, R. L., & Davis, C. L. (1999). Diagnosing pneumonia by physical examination: relevant or relic?. Archives of Internal Medicine, 159(10), 1082-1087.

Image of lung tissue riddled with cancer
Content for pathology should be a review from your anatomy and physiology courses. You are expected to be able to describe diseases of the respiratory system and how they may be classified (e.g. obstructive, restrictive, etc.). Respiratory refers to the gas exchange; pulmonary refers specifically to the lung organ.
There is a succinct listing of respiratory diseases included in Pagliarulo COPD and restrictive lung diseases pages 244-245. Focus on your ability to:
You should be able to provide an example of each disease listed below under the appropriate category. Notice some diseases fall in more than one category such as pneumonia:
In general, this limits the efficiency and effectiveness of exhalation. It is difficult to expel CO2
Chronic Obstructive Pulmonary Disease (COPD):
COPD describes a combination of two conditions
![]()
![]()
![]()
Common diagnosis and conditions that indicate restrictive disease are:
Here is a link on what is the cause of pneumonia
https://www.youtube.com/watch?v=yqwG-O3GR74
![]()
![]()
|
Classification |
Description |
Examples |
Signs and Symptoms |
Common Causes |
|
Obstructive |
Airway obstruction – difficulty moving air out of lungs |
COPD Emphysema Asthma Bronchitis Cystic fibrosis (CF) |
Productive cough Dyspnea |
Smoking Environmental particulates; allergies Genetic disorder (CF) |
|
Restrictive |
Increased lung stiffness/decreased compliance – infection or exposure resulting in scar tissue |
Asbestosis Respiratory Distress Syndromes |
Cough SOB |
Environmental exposure |
|
Infections |
Upper
Lower |
Cold Laryngitis Pneumonia Tuberculosis |
Sore throat, runny nose, sneezing |
Bacterial or Viral |
|
Pleural |
Collection of fluid in pleural cavity |
Pneumothorax Empyema |
Hypoxia Hypercapnia SOB Chest pain |
Trauma Acute or chronic infection Chronic lung disease |
You can check your understanding of the diseases, their descriptions and classifications by linking to the
Self Study Activities.
Note only one disease per category for this activity, due to limitations of the formatting design of the self-study
Subramanian, J., & Govindan, R. (2007). Lung cancer in never smokers: a review. Journal of clinical oncology, 25(5), 561-570.
Cameron & Monroe p. 372-384; Pagliarulo, Pg 254, Box 10-2, 259-263
![]()
Note: There is mention in the text of interventions specifically for those who are using mechanical ventilation equipment. We will be covering specific retraining and ventilator weaning considerations in PTA 205.
You should be able to recognize the signs and symptoms of over exertion in this population and make appropriate clinical decisions regarding exercise modification and termination.
![]()
![]()
Specific interventions, that can be a part of the PT plan of care, and delegated to the PTA may include:
airway clearance can be treated with hand-held devices, such as Flutter, Acapella, or Positive Expiratory Pressure. High frequency chest wall devices include a vest and a compressor and may be used in the home, especially by those affected by CF.
Exercise is an effective intervention for improving function in patients with obstructive and restrictive lung disease.
Physiological monitoring, medication use, such as bronchodilators (inhalers), and patient education in exercise monitoring are key components to an effective exercise, and the evidence is clear that exercise can reduce anxiety, body weight, and general cardiopulmonary efficiency (Spruit, et al., 2016). Patients with severe restrictive lung disease have shown improvements in quality of life with exercise and appropriate ventilator support (Ho, et al., 2013).
In general, cycling induces less oxygen desaturation than walking in patients with COPD. Desaturation during small muscle mass exercise (e.g. arm exercise) is not very common. (Pothirat, et al., 2015)
Sample exercise program
![]()
![]()
Fink, J. B. (2007). Forced expiratory technique, directed cough, and autogenic drainage. Respiratory care, 52(9), 1210-1223.
Ho, S.-C., Lin, H.-C., Kuo, H.-P., Chen, L.-F., Sheng, T.-F., Jao, W.-C., … Lee, K.-Y. (2013). Exercise training with negative pressure ventilation improves exercise capacity in patients with severe restrictive lung disease: a prospective controlled study. Respiratory Research, 14(1), 22. http://doi.org/10.1186/1465-9921-14-22
Morgan, K., Osterling, K., Gilbert, R., & Dechman, G. (2015). Effects of autogenic drainage on sputum recovery and pulmonary function in people with cystic fibrosis: a systematic review. Physiotherapy Canada, 67(4), 319-326.
Pothirat, C., Chaiwong, W., Phetsuk, N., Liwsrisakun, C., Bumroongkit, C., Deesomchok, A., … Limsukon, A. (2015). Long-term efficacy of intensive cycle ergometer exercise training program for advanced COPD patients. International Journal of Chronic Obstructive Pulmonary Disease, 10, 133–144. http://doi.org/10.2147/COPD.S73398
Spruit, M. A., Burtin, C., De Boever, P., Langer, D., Vogiatzis, I., Wouters, E. F., & Franssen, F. M. (2016). COPD and exercise: does it make a difference?. Breathe, 12(2), e38.
van der Schans, C. P. (2007). Conventional chest physical therapy for obstructive lung disease. Respiratory care, 52(9), 1198-1209.

Communication with the interdisciplinary team is very important. Equipment needs, environmental assessments for activity modification, and assist and supervision recommendations are a critical component to an effective and safe pulmonary rehabilitation program.
![]()
![]()

Image retrieved from http://www.veteranshealthlibrary.org/GotoGuides/COPD/6B2011502_VA_Large.png
Bill is a 62 year old man with severe COPD. He is a high school educated, retired truck driver who lives with his wife and son. He walks without an assistive device and has difficulty walking on the flat, showering and carrying heavy loads. These activities produce breathlessness and low back pain as he has had a previous fracture to the pelvis. As a result, his wife assists him with most ADLs. He stopped smoking three months ago following an 80 pack year history of smoking. The respiratory medications he uses are Seretide, Ventolin and Spiriva. He is keen to lose some weight and be able to return to gardening.
On assessment, his spirometry is FEV1 / FVC = 0.63/1.2 with an FEV1 (% pred) of 22%. His weight is 198 lbs, height 178 cm, BMI = 28.4. Resting HR = 85 beats/min; resting SpO2% = 93%. The supervising PT asks you to test his performance on a six-minute walk test. He is able to walk 300 yards with two rests in the best of two six minute walk tests but desaturated to 86% on room air and felt very severely breathless (dyspnea score = 7) at the end of the walk. (Adapted from Pulmonary Rehabilitation Tool Kit)
Active Learning Exercise
Classify elements in the case study according to ICF factors. Check your work by completing the associated labeling activity below

Now check your understanding of classifications
How did you do with your attempt to classify case elements? Can you think of how this mapping activity guides clinical planning and problem-solving within the physical therapy plan of care?
What exercises will you select to help Bill reach his goals? Given his desaturation response to walking, consider assistive devices and other physiological support that may help improve activity and conserve energy. What do you think is a likely intervention from the supervising MD based on the six-minute walk test result? What are you considering may be a best practice for patient and family education?
Want feedback on your reasoning? Post your ideas in the CAN YOU HELP ME? forum.
A tool to help guide thinking around ICF classification: http://apps.who.int/classifications/icfbrowser/
A presentation on how the ICF system is used in patient care planning: https://www.cms.gov/medicare/billing/therapyservices/downloads/mapping_therapy_goals_icf.pdf
American Lung Association. 2018. Measuring Your Peak Flow Rate. Available at: https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate.html
Lung Foundation Austrailia (2016). Pulmonary Rehabilitation Toolkit. Retrieved from http://pulmonaryrehab.com.au/importance-of-exercise/case-studies/case-study-one/