Elbow and Forearm Disorders
PTA 104 Orthopedic Dysfunctions

Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Elbow and Forearm Complex
Objectives
- Describe the mechanism of injury for common conditions for the elbow and forearm
- Select appropriate interventions and exercises based on the the tissue healing stage, precautions and contraindications for elbow and forearm conditions
Functional Anatomy
The elbow-forearm complex is comprised of the humeroulnar, humeroradial, and radioulnar joints. The majority of joint stability comes from the humeroulnar joint. Upper extremity mobilty for agility, reaching, and manipulating objects required functional range of motion within this complex.
Functional range of motion (ROM) is 30-130 degrees at the elbow and a combined 100 degree in the forearm, equally distributed
Anatomy and Kinesiology Review Videos(Approximately 8 minutes, and 4 minutes respectively)
Ligaments
The ligaments and joint capsule are primary sources of joint stability
- medial collateral ligament - also called ulnar collateral ligament, is a complex of three ligaments that form a fan: anterior, posterior, and transfer. It's role is to protect against valgus forces throughout the range of motion
- lateral collateral ligament - also called radial collateral ligament, intersects with the annular ligament, which provides stability against varus stresses
- annular ligament - stabilizes and controls the position of the radius with respect to the ulna and the humerus during elbow and forearm activities
The interossesus membrane provides stability between the radius and ulna during pronation and supination motions
Videos for Varus and Valgus Tests (Approximately 4 minutes)
Muscles, bones, and motions
Check your muscles that flex and extend the elbow, and pronate and supinate the forearm.
Components of an Elbow PT Exam
Christina narrates a Elbow PT Exam
Observation and Inspection
Posture (carrying angle, scapula position)
Functional use of arm during gait and ADLs
Soft tissue: atrophy, symmetry, swelling
Skin
Joint testing: hypomobility and hypermobility
AROM/PROM and overpressures
Accessory joint motion (distraction, medial-lateral and dorsal-ventral glides)
Mobilization with Movement
Manual Muscle Testing
Motor Function and Control
Muscle length
Palpation
Neuromuscular tests (light touch, DTRs, upper limb tension tests)
Special tests
median nerve (pinch grip, pronator syndrome, Tinel's)
valgus extension overload
thoracic outlet syndrome
pulses (brachial)
cervical screen (C5-T2 pathologies can refer to the elbow)
Review of images (if available)
Common Soft and Connective Tissue Conditions
Strains and Ruptures
Muscle strains of elbow flexors and elbow extensors can evolve over time with overuse, or can present suddenly with sudden forces to the joint. Tendons can rupture completely, which produces signficant bruising and a sudden loss of elbow strength and elbow and forearm function. Athough distal biceps and tricep tendon ruptures are rare, overuse and improper lifting techniques may result in rupture and loss of elbow function.
A PTA should be mindful of providing the appropriate exercise interventions, specifically when adding resistance or weight to the distal end.
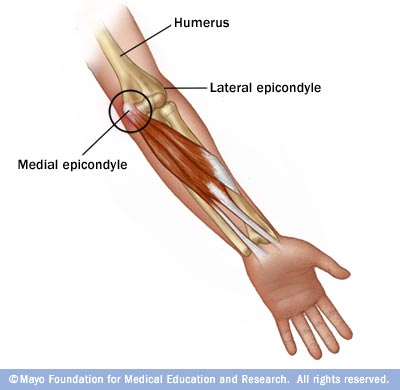
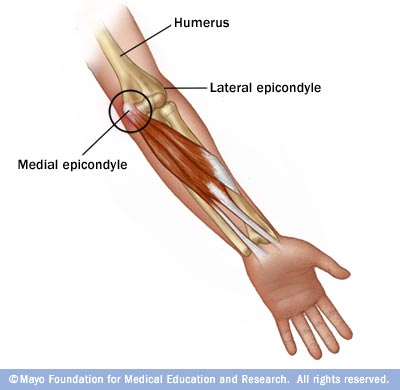
Medial Epicondylitis - Medical elbow tendinopathy
.jpg)
- onset is associated with faulty mechanics (e.g., with throwing, golfing, swimming) and with repetitive use (e.g. with hand tools)
- repeated microtrauma to medial flexors and pronator tendon leads to tendon overload and failure
- primary muscle involved: flexor carpi radialis, pronator teres; some involvement of palmaris, flexor carpi radialis, and flexor ulnaris
Video approximately 2 minutes
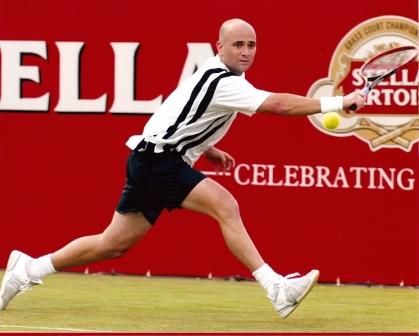
Lateral Epicondylitis - Lateral Elbow Tendinopathy
- 7% of all sports injuries (most common injury in elbow and forearm)
- presents most often in age 35-50
- tendon degeneration due to microtrauma from hyperpronation
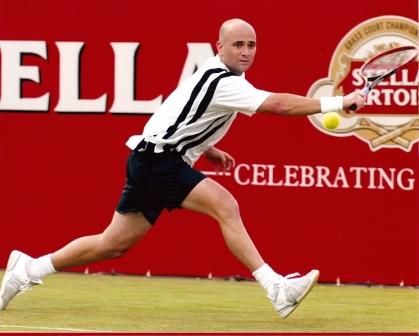
- high risk for chronic pain and dysfunction due to soft tissue changes from repetitive overuse/chronic inflammation
- can be a misdiagnosis: some evidence of referred cervical pain, peripheral nerve entrapment, bony changes or myofascial pain syndromes presenting with similar pain patterns
Videos approximately 4 minutes
Triceps Tendinitis
- rare
- sudden severe strain (javelin, tennis, volleyball)
- may evolve into a "snapping triceps" over posterior medial aspect of elbow due to subluxation or dislocation of portion of triceps and/or ulnar nerve
- incidence can be associated with decreased triceps flexibility
Medial Collateral Ligament Injuries
Valgus Overload Triad

- serious injury in the overhead athlete (baseball, javelin, racquet) involving the posterior medial joint capsule, the ulnar nerve, and the ulnar ligament (MCL)
- may also result from traumatic valgus strain during fall on outstretched hand
- ligament tears, tendon avulsions, tendinitis and bony changes may result
- in children, overload forces can result in asymmetric growth changes and disruption (e.g. stress fracture) to the growth plate (Little Leaguer's Elbow)
Summary of Common Soft and Connective Tissue Conditions
|
Diagnosis
|
Common Description
|
Involved Structures
|
Contributing Factors
|
Signs and Symptoms
|
|
Medial epicondylitis
|
Golfer's Elbow
|
Wrist flexors (common flexor tendon) and forearm pronators
|
Poor mechanics with sports and repetitive grip
|
Pain with resisted wrist flexion and forearm pronation; pain with passive wrist extension and supination; pain on medial epicondyle
|
|
Lateral epicondylitis
|
Tennis Elbow
|
Wrist extensors (ext. carpi radialis brevis origin)
forearm supinators
|
Overloading with sport and leisure activities involving grip and pronated grip
|
Pain with resisted wrist extension with elbow extension; pain with grip, pain in lateral epicondyle
|
|
Triceps tendinitis
|
Posterior Tennis Elbow
|
Triceps insertion; ulnar nerve
|
sudden strain to triceps in full arm extension
|
Pain with resisted elbow extension; snapping sensation with elbow flex/ext on posterior medial elbow
|
|
Valgus Overload Triad
|
|
MCL, post-med joint capsule, ulnar nerve
|
trauma; overuse in athletics
|
Pain and instability with valgus testing
|
|
(Epiphyseal Injury)
|
Little Leaguer's Elbow
|
Accelerated growth of medial epicondyle; ulnar hypertrophy
|
Overuse in throwing with strain to growth plate region in proximal forearm
|
Pain and tenderness with loss of full extension
|
|
Olecranon bursitis
|
Student's Elbow
|
Olecranon bursa, may include ulnar nerve
|
Mild, repetitive pressure; weight bearing on elbows
|
Swelling on posterior aspect cyst-like appearance, may include point tenderness in affected area
|
Treatment:
- Protect: immobilization, rest, ice, modalities, submaximal isometrics, cross fiber massage. Splinting and/or use of a sling often follows acute injury to prevent loading through use of the hand
- Controlled motion: assisted and self-stretching, cross fiber massage, joint mobilization and MWM, resisted isometrics, progressive functional strengthening patterns
- Return to function: sport and activity specific, plyometrics
- Patient education to prevent recurrence with modifying lifting, hitting carrying and HEP for injury management and prevention
Common Bony and/or Articular Conditions
Osteoarthritis and rheumatoid arthritis, dislocation and history of fracture are factors which may lead to progressive loss of function and/or surgical intervention
Myositis Ossificans (MO) & Heterotopic Ossification (HO)
- Bone spontaneously lays down into muscle (MO) or in surrounding areas or joint space (HO) following blunt trauma or fracture
- Idiopathic onset associated with traumatic brain injury
- Presents as red, hot, swollen, marked painful motion
- Active and passive ROM is encouraged and may require spinting.
- MASSAGE, PASSIVE STRETCHING AND RESISTIVE EXERCISES ARE CONTRAINDICATED
Internal Derangement
- periodic locking of joint due to loose bodies in joint
- results in loss of end-range flexion and extension which gradually resolve; repeat occurrences and predispose OA changes
- in adolescents: associated with trauma (chip fracture) or osteochondrosis
- in adults: cartilage fractures due to trauma and becomes a loose body (treated with joint manipulation); may need arthroscopic removal
- in mid-age to elder: fragments are more numerous: may result in longer periods of limted motion
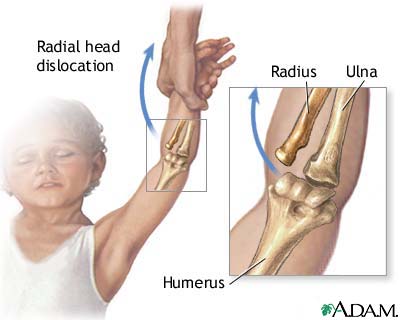
Subluxation of the Radial Head
- "Nursemaid's Elbow" or "Pulled Elbow": sudden traction injury
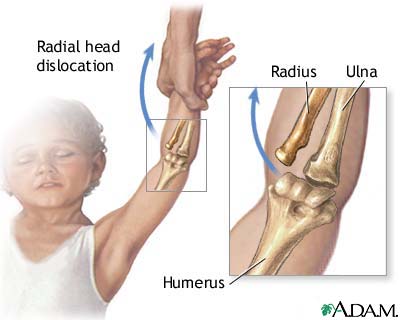
- Child is lifted up suddenly by the arm while it is held over their head in a pronated and extended position
- Presents with painful inability to use arm and avoidance of supination
- Generally resolves with short term immobilization
Trauma
- sprain/strain to joint capsule (likelihood increases with RA)
- traumatic ulnar dislocation
- fracture (radial fracture is most common elbow fracture)
- may result in post-immobilization capsular tightness and loss of motion, especially with closed reduction of a fracture
- may result in progressive osteoarthritis or joint replacement
- displaced fractures may require surgery with hardware and/or removal of bone
- should be taken with stretching if there is a bony block to ROM; overstretching can lead to hypermobility
Elbow Dislocation
Elbow subluxation and dislocation can have long-standing secondary effects associated with nerve trauma and heterotopic ossification. Uncontrolled swelling can result in disability that includes the wrist and hand.
Patients are typically placed in a posterior splint for up to 2 weeks and then begin gradual ROM and strengthening of surrounding structures to progressively add stability while ROM is progressively increased.
End of Lesson


.jpg)