Introduction to Nerve Complications After Bone Trauma
PTA 104 Orthopedic Dysfunctions
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Nerve injury can result following a fracture and may result in most disabling symptoms well after the bone tissue is healed. Injury to nerve tissue may be temporary or permanent. Specific interventions for management of upper and motor neuron conditions will be covered in PTA 204/204L. The purpose of this lecture is to introduce the etiology of nerve disorders as it related to fracture diagnoses and to reinforce how the phases of healing discussed for conditions of orthopedic conditions/trauma relates to management of peripheral nerve conditions
Nerve entrapment in the upper and lower extremities can be temporary or long-standing. Conditions such as obesity and pregnancy where there is increase fluid or body weight on nerves can interfere with nerve gliding. Surgical interventions and subsequent scar formation can also entrap nerves, resulting in chronic nerve symptoms, pain, and loss of function.
In some cases, patients consent to surgery to release the nerve or to transfer nerves to restore function in affected sensory and motor areas.
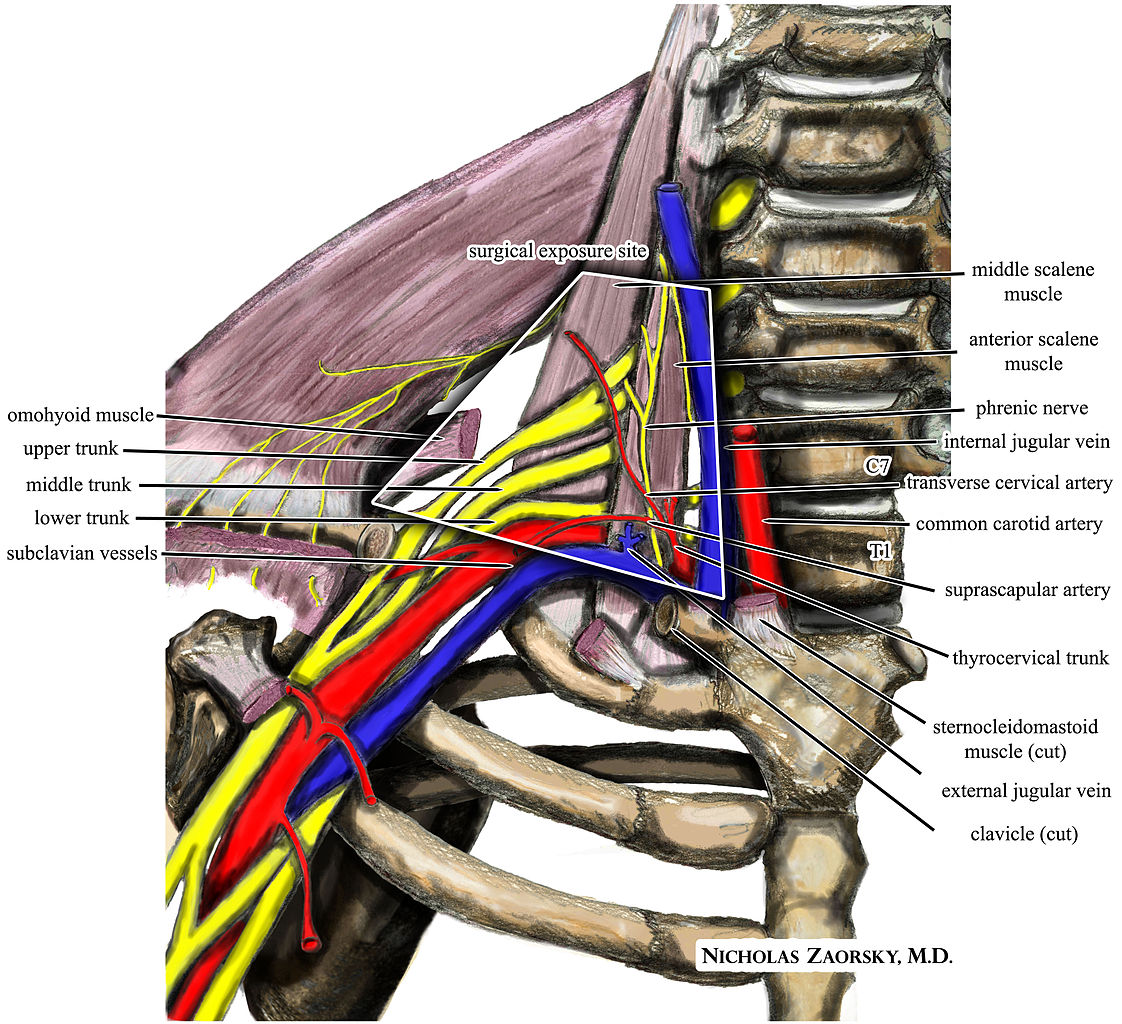
Upper extremity nerve injuries are more common than lower extremity. Compression and traction (stretching) forces to components of the brachial plexus can result in pain, loss of sensation, and loss of motor function. Note how the brachial plexus originates from C5-T1 and then forms a series of overlapping trunks, divisions, and cords, before branching into peripheral nerves. Proximal compression can result in significant neurovascular syndromes, which may requires surgical releases to preserve nerve function and circulation. Neal and Fields (2010) noted, "risk factors include a superficial position, a long course through an area at high risk for trauma, and a narrow path through a bony canal"
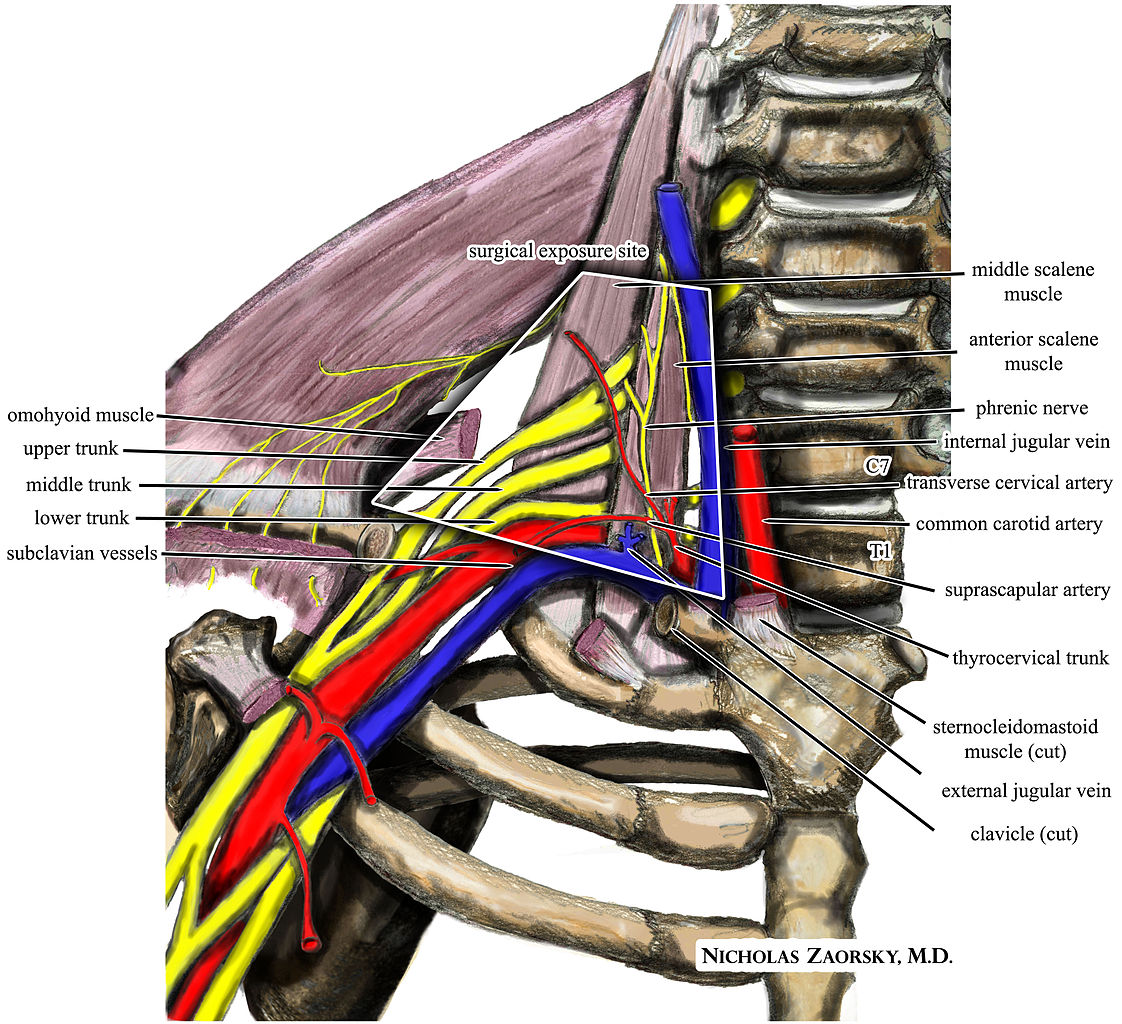
https://commons.wikimedia.org/wiki/File:Brachial_plexus_anterior_view_nerves.JPG;
https://commons.wikimedia.org/wiki/File:Wikipedia_medical_illustration_thoracic_outlet_syndrome_brachial_plexus_anatomy_with_labels.jpg
|
Nerve |
Injury Risk |
Presentation |
|
Axillary |
Stretch during abduction; glenohumeral dislocation; compression in axilla (e.g. misuse of crutches) |
Weakness in teres minor and deltoid |
|
Long Thoracic |
Sudden upper extremity traction; shoulder depression with contralateral lateral cervical flexion, sustained compression ("Backpacker's syndrome) |
scapular winging |
|
Suprascapular |
Throwing athletes, trauma, clavicle fracture |
supraspinatus weakness, atrophy and tenderness, pain with horizontal adduction, |
|
Median |
Elbow, forearm, and wrist overuse or injury |
weak and painful grip; sensory changes in hand |
|
Musculocutaneous |
Shoulder dislocation; biceps injury; hypertrophy of coracobrachialis |
shoulder and elbow flexion weakness |
|
Radial |
Proximal humerus fracture; elbow fracture or dislocation; "Saturday Night Palsy" when passing out from alcohol use results in prolonged compression on chair or bar |
weakness in elbow flexion and wrist extension |
|
Ulnar |
Elbow dislocation or prolonged posterior elbow compression; repetitive throwing |
weakness in the ulnar side of the hand and interossei |
|
Nerve |
Injury Risk |
Presentation |
|
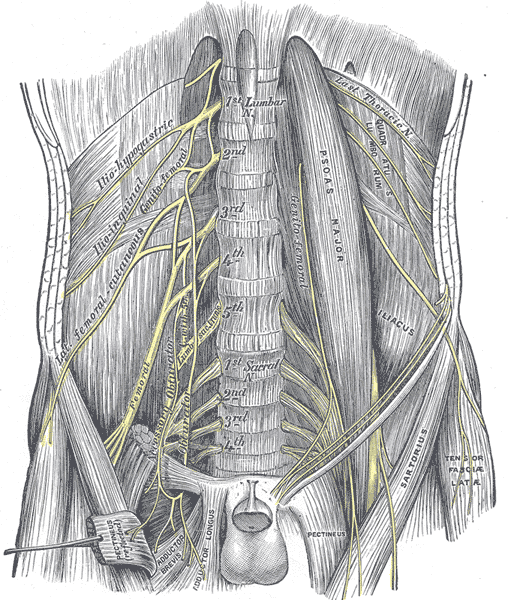
ilioinguinal (T12-L1)
|
Lower abdominal surgery; orthopedic surgery (iliac bone harvesting for bone graft), pregnancy
|
pain in groin and medial inner thigh, may radiate to genital areas |
|
lateral femoral cutaneous nerve (L1-L3) |
tight clothing (e.g. jeans), pregnancy, trauma to ASIS |
also known as "meralgia paresthetica" burning, coldness, or lightning like pain on lateral thigh
|
|
femoral nerve (L2-4) |
trauma (surgical or other), pelvic fracture, acute hyperextension of hip, diabetes (neuropathy), tumors |
numbness, tingling and burning in the thigh, quadriceps weakness; difficulty managing stairs, feeling like knee will buckle |
|
sciatic nerve (L4-S1)
|
hypertrophy of piriformis, direct trauma to SI or gluteals, hip flexion contracture, excessive hamstring exercise
|
also known as "piriformis syndrome" Numbness, tingling, and weakness in the posterior hip and extend down posteriorly to the toes |
|
tibial nerve
|
Rheumatoid arthritis, Baker's cyst (posterior knee), diabetes, tight-fitting shoes, pronation or pes planus
|
also known as "tarsal tunnel syndrome" when involves the posterior tibial nerve sensation changes and weakness to the bottom of the foot and toes; weakness in plantar flexion and eversion; pain with weight bearing
|
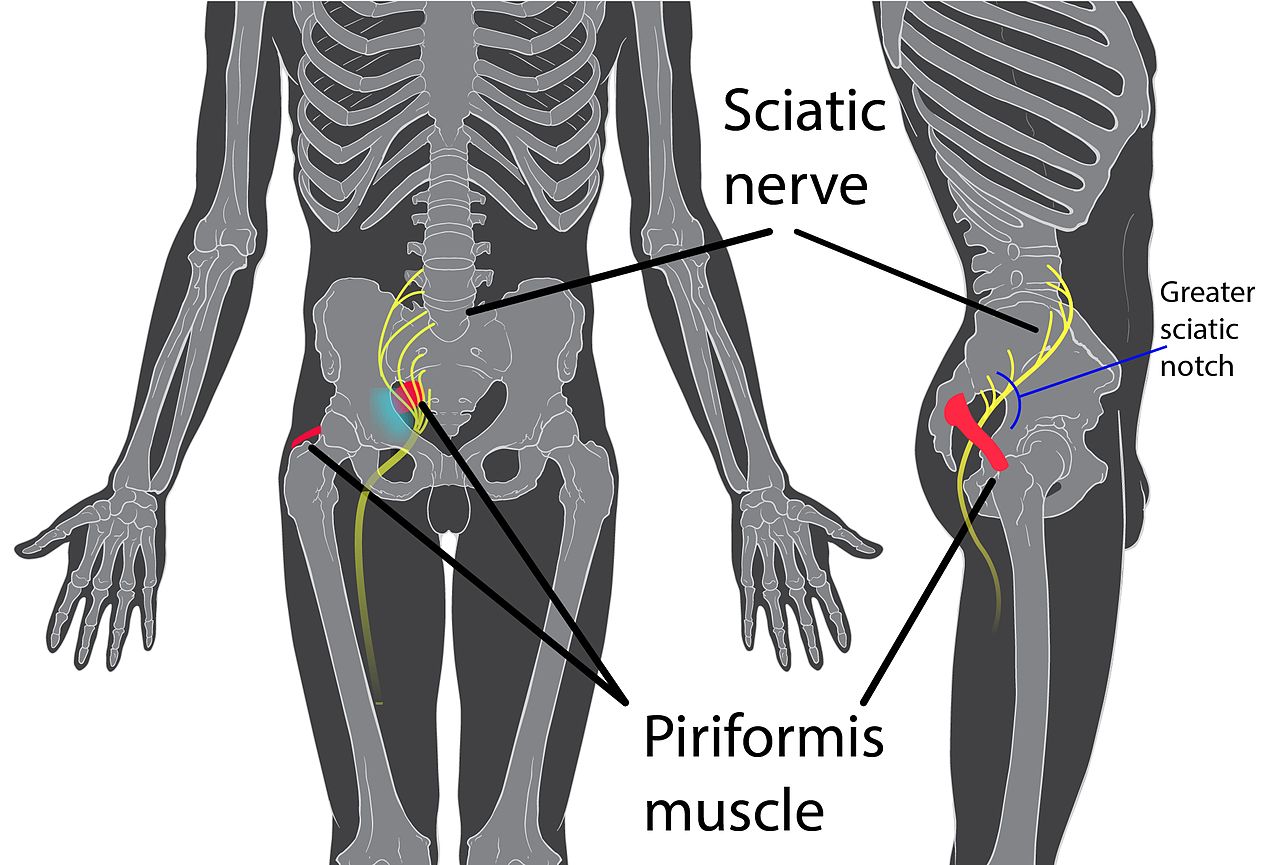
https://en.wikipedia.org/wiki/Piriformis_syndrome
Immobilization and interventions for controlling inflammation and reducing swelling is the primary focus. Gentle AROM in unaffected areas and in pain-free ranges to help maintain nerve mobility above and below the injury is introduced. Care is taken to avoid positions and motions that increase nerve symptoms (pain and sensory changes). Close monitoring of skin for lesions, such as blisters to rule out possible infectious or systemic sources of nerve function loss.
Wrist and hand conditions: Avoid hot, cold or sharp objects; Do not prolong grasp positions, change hands frequently; Utilize built up handles to distribute pressure
Lower extremity conditions: Wear well fitting, protective shoes, have closed toes and heels; Inspect feet daily for signs of pressure or abrasion; Do not walk barefoot; Frequently shift weight during all standing activities
The nerve is demonstrating recovery through increasing sensory activity or muscle activity. Motor retraining begins with isometrics in shortened positions and electrical stimulation to promote motor recovery is introduced.
Desensitization may be used by application of various sensory inputs to the affected area, such as placing soft and rough textures on the affected skin.
Discrimination retraining may be used to reteach differentiating 2 points of simultaneous contact. Begin with visual input, then remove it.
Interventions are largely compensatory, such as using assistive devices, alternative movement strategies, activity modification, and patient education in activities that may increase strain to the nerve. Interventions for these more complex conditions are addressed in PTA 204/204L; may include interventions, such as the use of a mirror box or guided imagery for pain management and sensory reorganization.
Congratulations - you've finished your final lecture as a first year SPTA!