
Shoulder Conditions and Considerations
PTA 104 Orthopedic Dysfunctions
PTAs apply rehabilitation exercises and injury management and prevention principles to patient with shoulder complex dysfunction. In order to safely and effectively select appropriate interventions specific to the patient's rehab stage and treatment response, PTAs must demonstrate understanding of protection, controlled motion, and return to function phases of rehabilitation.
By understanding the signs/ symptoms, impairments and functional limitations, PTAs are able to prioritize exercise and other interventions based on the understanding how inflammation and the stages of tissue healing effect recovery.
PTAs provide patient education and monitor progress to maximize patient compliance with activity modifications, postural corrections, joint protection, and exercise progressions. PTAs apply knowledge of surgical approaches and special tests in prioritizing interventions specific to the patient's current condition while strictly complying with post-operative surgical precautions and contraindications where indicated.
Recall structure and function of shoulder and shoulder girdle components
Peripheral joint mobilizations are manual techniques which use physiological motions or accessory joint motions to increase ROM, decrease pain, and facilitate neuromuscular re-education.
High velocity thrust manipulations (Grade V) are outside of the PTA scope of practice.
PTAs instruct patients in self-mobilization techniques to increase accessory joint motion, particularly in the shoulder region. PTAs also apply knowledge of postural factors on arthokinematics in order to progress toward return to function. PTAs may observe subluxations or other positional faults which may be impacting progress and, therefore, require further assessment from the PT.
Contraindications and precautions for joint mobilization are closely aligned with those for stretching.
The PT will select a joint mobilization technique based on the tissue healing stage and patient pain levels. Lower grades of joint mobilization are indicated for acute pain modulation and fluid mechanics in a joint and are performed in the available range without resistance. Higher grades of joint mobilization are indicated when it is safe to mobilize into and through tissue resistance.
PTAs should be able to describe and understand the grades of joint mobilization in order to safely progress mobility with therapeutic exercise and functional activities. PTAs should document response to the previous treatment(s), so the PT may use the data for clinical decision making regarding modifications or progressions to joint mobilization techniques.
Peripheral joint mobilization is described in detail in Chapter 6, Dutton. Key points are summarized in the Joint Mobilization Take Home Points handout (see sidebar on this page).
are treated with casting (closed reduction) or hardware (open-reduction/external fixation). ROM to prevent contractures are the primary component of early rehabilitation. Progressive strengthening and stretching for improving post-fracture weakness and atrophy will depend on integrity of bone tissue during fracture healing. A significant complication of humeral fracture is avascular necrosis of the humeral head. Indications for joint replacement secondary to avascular necrosis are discussed further in the section on Surgical Management.
Incidence of scapular fracture is highly associated with trauma, therefore, patients will often present with other fractures, glenohumeral dislocations, pneumothorax, and/or neurovascular injuries. Scapular body fractures are the most common scapular fracture and are generally treated non-operatively. As pain and swelling subside (2-3 weeks of immobilization), patients may progress from isometric to active exercises.
|
Presentation |
Associated conditions/etiology |
Clinical signs and symptoms |
Impairments |
Functional Limitations |
|
Joint is stiff, motion and muscle function is limited |
OA/RA, trauma, immobilization, idiopathic adhesive capsulitis |
limited external rotation>abduction, pain, limited functional motion |
Pain during sleep/lying, pain and limited motion, scapular compensation, decreased arm swing during gait |
Difficulty dressing, grooming, reaching and lifting; difficulty reaching behind back |
Joint stiffness and pain can result from overuse of contractile and non-contractile structures. Arthritic changes to the humeral head, glenoid fossa, acromion, or sternum can all impact function. Joint stiffness can evolve during or following hospitalization due to illness or decline in function. Patients who are confined to bed or have extended periods of compromised cardiopulmonary endurance may develop stiff and painful shoulders in as little as 1-2 days. PTAs play a significant role in patient, family, and staff education in correct ROM techniques for the shoulder for contracture prevention and management.
Adhesive capsulitis ("frozen shoulder") has a greater incidence in women (40-60 years old) and may be associated with diabetes and other chronic inflammatory conditions. Significant functional limitations can present in as little as 24 hours following initial symptoms. Depending on pain, length of symptoms, and functional limitations, patients may undergo manipulation under anesthesia to manually break through adhesions in external rotation and abduction without an inhibitory guarding response. PROM immediately following manipulation and patient education in ROM techniques follows this procedure.
During the maximum protection phase, PTs will use mid-range joint mobilizations to increase mobility without increasing pain.
|
Acute "freezing" (10 wks to 3 months) |
Subacute "frozen" ( from 4 months to 12 months) |
Chronic "thawing" (2 months to 24 months) |
|
Patient presents with pain at rest and with shoulder motion Controlled pain-free motion and interventions to promote relaxation of muscle guarding of the glenohumeral joint, cervical area, and scapulothoracic muscles Scapula stabilization exercises with correct technique Joint mobilization
Frequent ROM (3-5 x) during day and stretching in end-range
Modalities for pain relief: ice, US, estim |
Patients present with pain only with shoulder motions, scapula compensation with movement, and deltoid atrophy.
Exercise to restore glenohumeral and scapulothoracic motion and prevent scapula substitution; progressive strengthening of deltoid, scapula, rotator cuff and upper arm
Submaximal closed chain isometric shoulder strengthening |
Patients present with little to no pain, joint stiffness, and decreased muscular endurance
PT to Increase strength, endurance and functional use; continue self-stretching |
Precautions with Adhesive Capsulitis: Therapy is too aggressive if the patient reports increased pain or joint irritability
Contraindications with Adhesive Capsulitis: Stretching into end-range when there are signs and symptoms of active inflammation
Excessive motion at the glenohumeral joint can increase stress to bone, contractile and non-contractile tissue resulting in increased degeneration, instability with subluxation/dislocation, and overuse of static and dynamic stabilizers (sprain, tendinitis, etc.). Conditions which may result in hypermobility include:

https://www.ncmedical.com/item_669.html
Non-traumatic AC joint dysfunction is common in adults over 40. Correction of postural stressors and muscle imbalances can prevent or minimize progression of arthritis. Weight lifters and individuals who repetitively load the upper extremities are more likely to experience dysfunction in these smaller shoulder complex joints
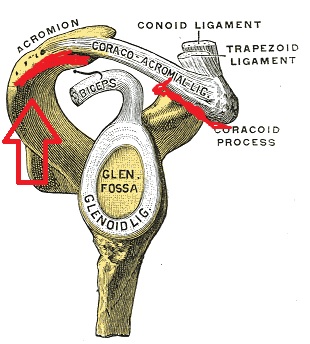
http://upload.wikimedia.org/wikipedia/commons/e/ec/Gray328.png
|
Overuse |
Subluxation or Dislocation of AC jt |
Hypomobility |
Impairments |
Functional Limitations |
|
Associated with repeated diagonal extension-adduction-internal rotation (tennis, volleyball) and repetitive motion at waist level |
Associated with direct fall onto shoulder and fall on outstretched arm May include partial or complete tear of supporting ligaments |
Associated with poor posture, especially scapular depression and retraction; OA common in AC joint after age 40 |
Localized pain; pain with shoulder elevation, horizontal adduction or abduction, hypomobility, neurovascular dysfunction |
Difficulty with repetitive motion forward/backward; limited participation in volley sports; decreased overhead reaching |
AC joint subluxations and dislocations can be graded by MDs and radiologists based on the amount of ligamentous damage. When reviewing the medical record, you may see reference to Grade I, II or III AC sprain. Higher grade sprains are less stable. AC joint disruption is also referred to as "shoulder separation"
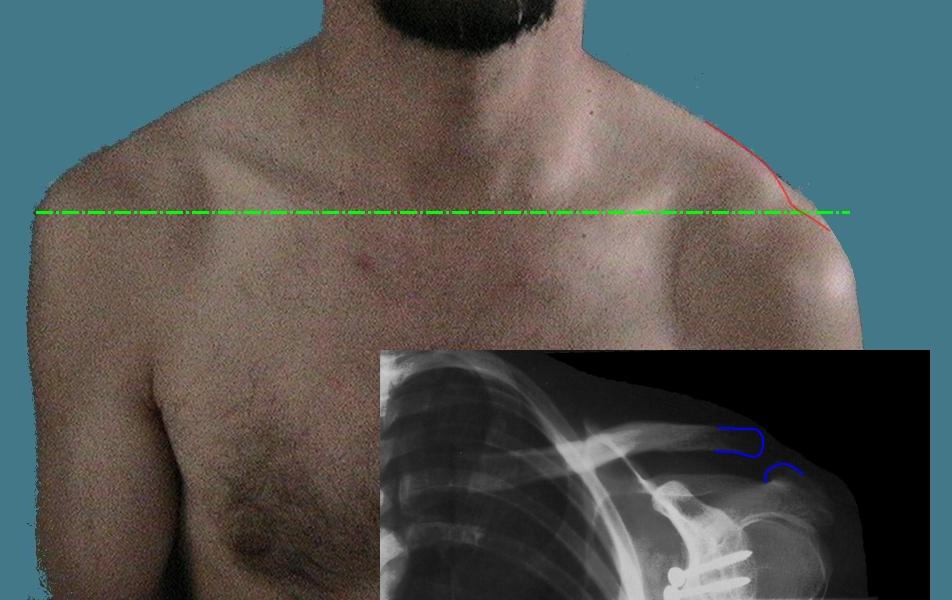
http://upload.wikimedia.org/wikipedia/commons/9/9e/Luxation_acromioclaviculaire.jpeg

Grades II and III A-C sprain benefit from a harness or sling for 3-6 weeks so that the torn ligaments can heal through superior pressure to clavicle. Clavicle braces are also prescribed following clavicle fracture
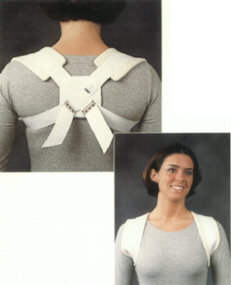 http://heritagemedical.typepad.com/heritage_medical/shoulder/
http://heritagemedical.typepad.com/heritage_medical/shoulder/
Video is approximately 3 minutes
Impingement typically presents as subacromial impingement; however impingement can also occur between the glenoid, the glenoid labrum and the suprapinatus and infraspinatus
|
Associated condition/etiology |
Clinical s/sxs |
Impairments |
Functional Limitations |
Goals and Treatment(s) |
|
Overuse from repetitive motion (overhead, throwing) Overuse from repetitive eccentric loading (racquet sports, volleyball, etc.) History of joint stiffness, OA, acromion shape precursors History of fall on outstretched hand History of MVA (holding steering wheel at impact) Poor posture (thoracic kyphosis, ant-posterior muscle length-tension imbalances Poor glenohumeral joint stability |
Painful arc of motion (usually 60-120 degrees of abduction) Pain with sidelying, reaching overhead, reaching behind back, lifting Point tenderness at musculotendinous junction of involved structure
|
Pain, muscle guarding, posture, weakness, joint dysfunction |
Decreased lifting, pushing, pulling, overhead reaching, dressing, grooming |
Control pain and swelling, increase and maintain maximum pain-free range of motion, modify activities/ADLs, increase scapular control and stabilization, restore strength and timing of scapular and RTC during AROM, increase muscular endurance and postural control, progressive return to functional and sports-specific activities
Ice, NSAIDS, Iontophoresis, ultrasound, progressive strengthening, joint mobilization, stretching, postural education and re-education |
During the initial immobilization, the PT documents all limitations of specific joint motion. Each limitation is addressed as part of the rehabilitation program. However, if the PTA recognizes delayed restoration of motion, reduced motion, or increased pain during the rehabilitation program, then he or she immediately must communicate this to the PT.
(Frozen Shoulder) may require surgical intervention to restore function. PTAs can help patients with post-operative education by understanding the structures involved and the expectations for post-operative recovery. Take a moment to review the Animation of Surgery for Adhesive Capsulitis (approximately 20 minutes) to reinforce information from your text book readings.
Surgical techniques can include resurfacing of existing bone, replacement of the humeral head (hemiarthroplasty) or replacement of the humeral head and the glenoid fossa (total shoulder arthroplasty/replacement (TSR)). Traumatic fracture of the humeral head may lead to avascular necrosis and necessitate a TSR to restore arm function.
Choice in surgical procedure will depend on the involvement of articular surfaces and associated soft tissues.
Primary goals for TSR are
Surgical approaches vary with patient condition and surgeon preference. Your text discusses general surgical procedures for a variety of shoulder prostheses. The take home message for the PTA is SURGEONS ESTABLISH ROM LIMITATIONS AND RESTRICTIONS FOR EACH CASE. If you are not sure of the ROM limitations for a post-operative TSR patient, consult with the supervising PT or contact the physician's office for clarification. Err on the side of caution and choose interventions which do not involve GH motion, such as pain management, postural instruction, activity modification, and alternatives for cardiovascular exercise.
In general, TSH without repair of the rotator cuff will have a maximum of 140 degrees of abduction range available. Patients who undergo a rotator cuff repair and TSH average 60 degrees of abduction post-operatively.
Fusion of the shoulder is generally selected when there are no other non-operative or operative approaches which will minimize instability in the shoulder complex. PTAs should understand the significance of post-operative precautions and maintain mobility in distal joints during the recovery phase
Following fusion, ROM is generally limited to the following
Functional use of the arm is achieved through scapular motion. Consider the muscle origin and insertions at the scapula: what overuse or secondary conditions may evolve with repetitive scapular motions?
The procedure is also referred to as acromioplasty and can be abbreviated 'SAD' in the medical record. SAD can uses arthoscopic techniques to remove bone spurs in the subacromial area and to remove debris associated with overuse. Surgical decisions to try SAD are based on patient symptoms and previous response to conservative treatment (PT, cortisone, meds, etc. ). Once the surgeon has visualized the RTC tendon during SAD, he/she can assess if a rotator cuff (RTC) repair is indicated.
Video of SAD arthroscopic surgery. Approximately 1.5 minutes
Recovery from SAD is typically 3-6 months. Rehabilitation processes are similar to management of impingement syndromes, with an emphasis on maintaining soft tissue mobility and preventing overuse. Patients may initiate RTC strengthening exercises soon after SAD as long as there has been no surgical repair of the RTC.
RTC tears can be due to repetitive motions or from trauma. Non-surgical and surgical management is largely driven by patient symptoms, surgical approach, and tissue healing times to allow repaired and/or fragile structure to heal. Too much too soon in these patient can result in total loss of RTC function.
Factors influencing RTC surgical approach include history of chronic impingement, size of RTC tear, associated pathologies in the shoulder, and general medical condition/stability.
Video is approximately 1.5 minutes
Special test for SLAP is the O'Briens (Video is approximately 2 minutes)
Rehabilitation protocols and progressions can vary from patient to patient and from surgeon to surgeon. In your text, you will find some guidelines for PT interventions based on the tissue healing phase. Note: most of the progressions are based on patient pain response, quality of shoulder motions (degree or absence of compensation), and surgical approach. All interventions consider pain levels and interventions to decrease pain and inflammation associated with exercises and functional use. Techniques to mobilize soft tissue (cross friction massage, joint mobilization) are introduced incrementally and respect pain limits and capsular barriers. Active exercises are generally progressed when there is no pain; resistive exercises are progressed (weights/bands) later in the rehabilitation stage when normal shoulder mechanics are restored. Proprioceptive activities in closed chain are only initiated when there is evidence of both increased strength and endurance in the rotator cuff (RTC) muscles without pain. Posture is ALWAYS included to prevent or minimize recurrence.
When referencing your text, formulate patterns for intervention based on the protection phase of the condition. For example, how does ROM exercise classification change as you progress the patient from maximal to moderate to minimal protection phases?
|
scapula |
glenohumeral |
tight |
weak |
|
forward tilt downward rotation of glenoid |
relative abduction relative internal rotation |
pectorals minor levator scapula scalenes |
serratus anterior trapezium shoulder external rotators |
Manual stretches for increasing flexibility are illustrated on pages 504-505 in your course text.
Early on in RTC repair rehabilitation, care must be taken to minimize anterior translation of the humeral head to avoid compression forces to the repaired structures. Techniques during PT include:
Exercises in the scapular plane are preferred for rehabilitation and home exercise programs for rotator cuff dysfunction. In addition to greater tubercle clearance, scaption allows muscles to strengthen in the most functional position and produces less tension on the joint capsule compared to straight plane motions (e.g., flexion and abduction
When progressing PROM to AAROM, continuously monitor for normal scapulohumeral rhythm; compensatory motions are an indicator of RTC insufficiency and care should be taken to instruct the patient in risks for reinjury/recurrence associated with abnormal mechanics
Scapular "setting" exercises are essential to restoring shoulder function. Consider these the "core strengthening" of the shoulder complex. Supine positioning can be used to assist with scapular setting during early ROM activities
During closed chain activities, monitor your patient for signs and symptoms of scapular muscle insufficiency. Scapular winging during wall push-ups or quadruped activities indicate poor stability of the scapula
During the acute healing phase, ROM exercise for the forearm, wrist and hand can maintain mobility, provide pain relief and indirectly and gently mobilize recently injured and repaired structures.
In addition to ChoosePT, an extensive amount of patient resources for multiple shoulder conditions are available for downloading and printing through eOrthopod