Wrist and Hand Conditions
PTA 104 Orthopedic Dysfunctions
Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Objectives
- Review the major functions of the hand
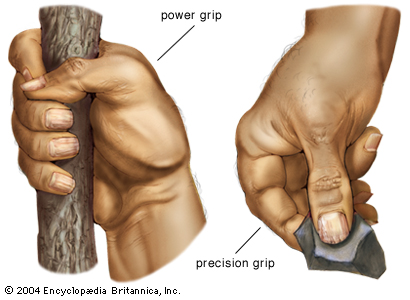
- Describe functional positions of the hand (resting, power grip, precision grips)
- Relate common contractures of the hand to specific pathology
- Describe special tests used to identify sources of wrist and hand dysfunction
- Apply principles of tissue healing to wrist and hand conditions throughout the tissue healing stage
- Describe precautions for stretching in post-operative and/or inflammatory conditions
- Select proper friction massage techniques for scar tissue management in the wrist and hand
- Select a correct exercise intervention for the wrist and hand based on tissue healing stage and case information
Hand Function Review

Wrist and Hand Pathology
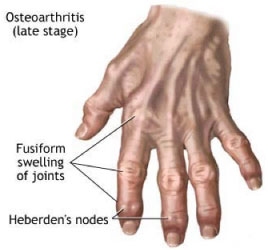
Osteoarthritis
Frequently involves the CMC joint of the thumb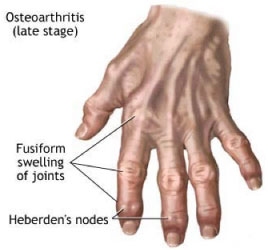
_553.jpg)
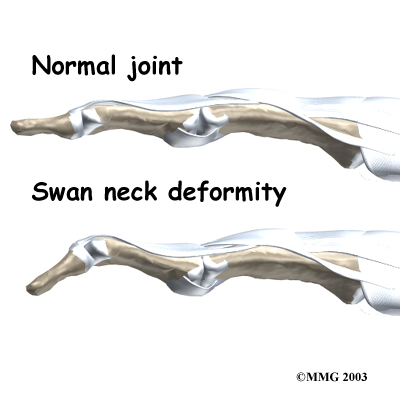
Rheumatoid Arthritis
Hand deformities, regardless of underlying pathology, may require joint replacement if pain and functional ROM (either due to stiffness or instability) markedly interferes with functional use of the hand.
Idiopathic Hand Deformities
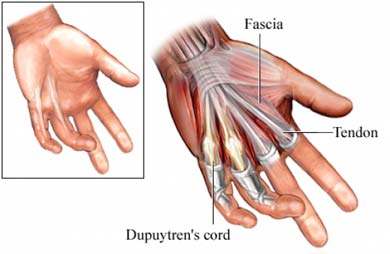
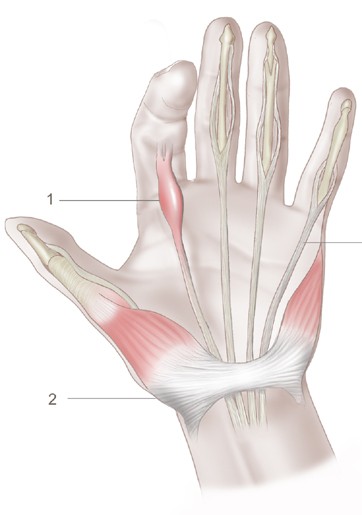
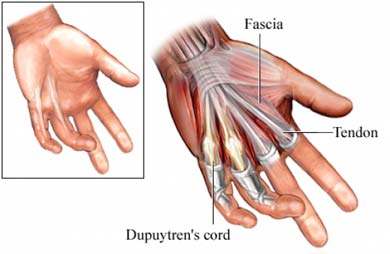
Dupuytren's Contracture
-
unknown etiology, however, incidence is associated with diabetes mellitus, genetics, smoking, alcohol use, and epilepsy
- more common in men
- progressive thickening and stiffness in palmar fascia of the hand:
Overuse injuries
- Carpal Tunnel Syndrome (CTS)
- compression to the median nerve can result in pain, sensory changes in the median nerve distribution, and hand weakness.
- nerve tension along the median nerve sheath can also produces symptoms associated with CTS.
- Review the instructional video on carpal tunnel syndrome for the take home points on this overuse injury
Video Approximately 3 minutes
Special tests for CTS
Phalen's Test (Video Approximately 2 minutes)
Tinel's Sign (Video Approximately 2 minutes)
Allen's Test (Video Approximately 2 minutes) - assesses circulation in the hand
- Wrist sprain
- Most common ligaments involved in strain are:
- lunate-capitate ligament (dorsal)
- radiocarpal ligament (palmar)
- Onset is usually traumatic and involves compression with hyperextension
- Fall striking the dorsum of hand can result in end-range flexion compression
- DeQuervains Syndrome
- most common tendinitis of the wrist in athletes
- involves the common sheath of the abductor pollicis longus and the external pollicus brevis where they pass along the distal aspect of the radius
- Special test: Finkelstein's
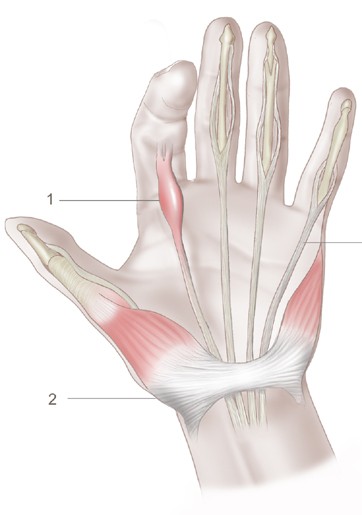
- Trigger finger
- thickening of the flexor tendon sheath from repetitive microstrain
- may be caused by repetitive handiwork (knitting, beading, etc.) or unconscious fist clenching
- acute onset is associated with sustained, direct pressure to the flexor tendon sheath during sport (i.e., gripping baseball bat, racquet, golf club)
- digit locks into flexion, typically after sleep
- may be treated with cortisone injection to reduce localized inflammation in the affected tendon
Bony Trauma
fractures or bony disruption to the wrist and hand are most commonly associated with falls. Careful screening for balance training or home safety should be considered for patients where falls are suspected or reported.
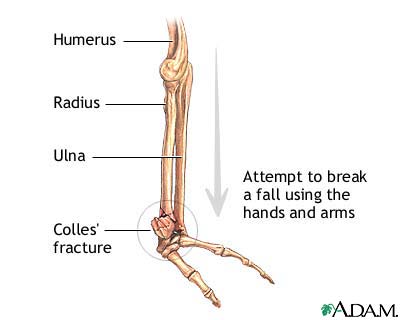
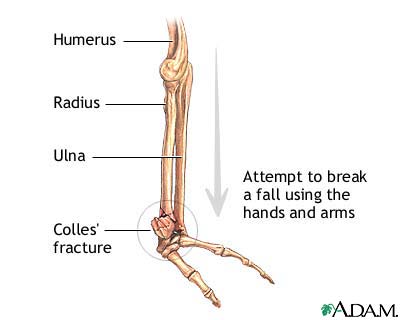
- Colles' fracture
- fracture of the distal radius and may or may not involve the ulna
- incidence is higher in women
- associated with falls
- most common diagnosis associated with wrist dysfunction
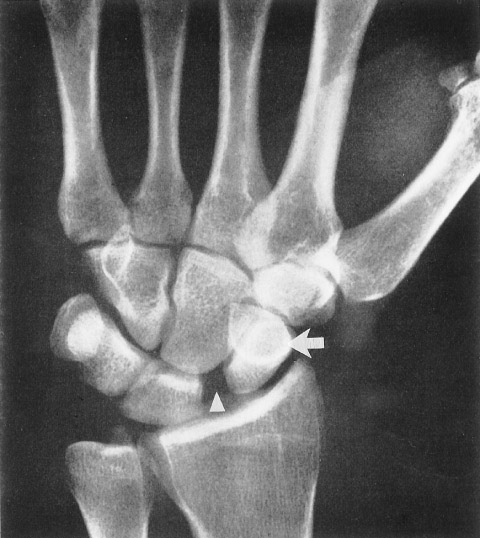
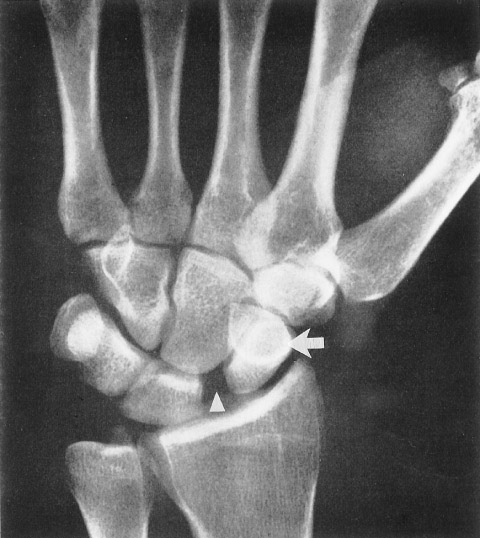
- Scaphoid and lunate dislocation: associated with fall on the outstretched hand with impact on the distal row of carpals
Management of Wrist and Hand Conditions
Approaches in PT will depend largely on the level of acuity, pain, surgical precautions and restriction, and patient goals.
When treating a post-surgical patient (i.e. joint replacement, tendon repair, internal reduction), always observe ROM precautions and do not progress into active or active-assisted ROM activities until cleared by PT/MD.
Acute wrist and hand management principles:
- Immobilization
- attention to preserving maximum hand function and length tension relationships
- allowing repaired or replaced structures to rest according to post-operative guidelines and tissue healing principles
- FAILURE TO PROVIDE ADEQUATE PROTECTION TO INJURED STRUCTURES CAN RESULT IN COMPLETE TENDON AND/OR LIGAMENTOUS TEAR AND PERMANENT LOSS OF HAND FUNCTION
- Joint protection - Splinting
- custom or prefabricated splinting to allow for rest and tissue healing
- dynamic splints may be prescribed to allow for some motion in a limited range
- patient education in donn/doff, wear time, skin inspection, hygiene
- may include use of a platform attachment on crutch or FWW to allow continued ambulation while patient is NWB in the wrist
- Edema management - emphasis on relieving and reducing pressure to neurovascular structures to avoid secondary injury to surrounding nerves and tissue
- ace wrapping or compressive bandages
- contrast baths (hot/cold) for facilitating fluid reduction
- modalities
- instruction in positioning for edema management
- Soft tissue mobilization
- gentle scar mobilization and fascia mobilization for pain, swelling, and contracture management
- static stretching should precede friction massage to allow for creep of constrained soft tissue
- manual friction force is applied longitudinally to flexor tendons, both proximally and distally, while the tendons are on stretch
- Progressive early active motion (flexor tendon)
- Static, isometric exercises
- need MD clearance following any tendon or joint repair
- may need PT/PTA supervision to prevent inadvertent motion during muscle contraction
- "place and hold": patient is placed in position to challenge involved tendons and then is asked to "hold" the position
- ROM to uninvolved distal hand and proximal UE
- focus on maintaining ROM in unaffected joints and preventing secondary stiffness and weakness in shoulder, scapula, elbow, or forearm
- Activity modification
- instruction in alternative ways to lift, carry, dress, bathe, etc to allow affected wrist and hand structure sufficient protection for healing
- Coordination with OT
- in cases of significant hand trauma, patients may be referred to a certified hand therapist (CHT) for rehabilitation.
- Occupational therapy is likely to be involved to insure progressive return to function
- OTs fabricate and modify custom splints for the hand and can instruct in methods to modify grip to allow hand function without excessive stress to healing structures.
Subacute Wrist and Hand Management
- ROM with gentle stretching
- care with patients who have RA: no over stretching of involved joints
- Static isometric exercises - progress to different positions in the range
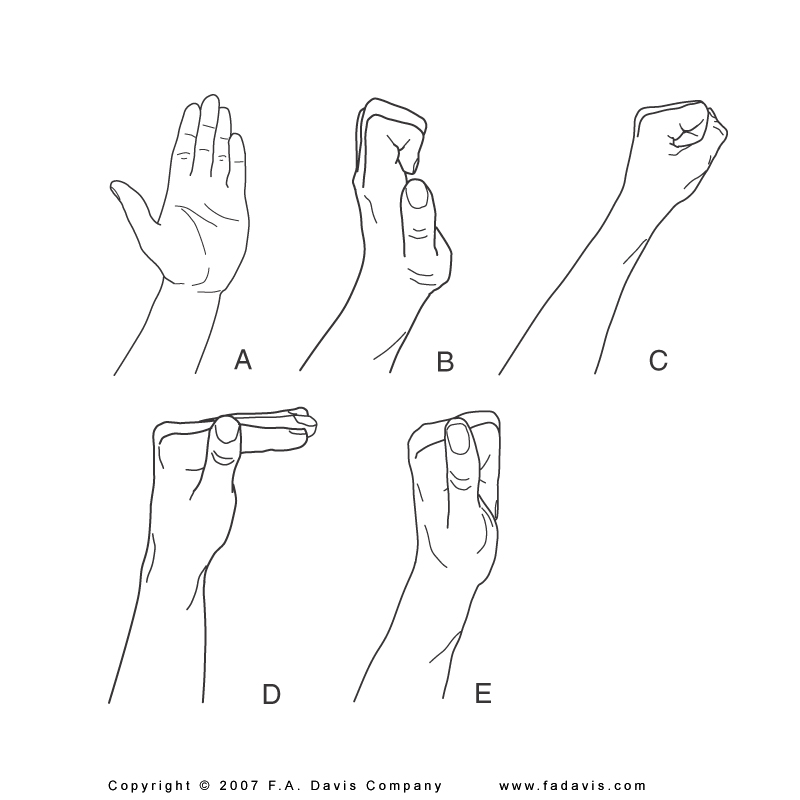
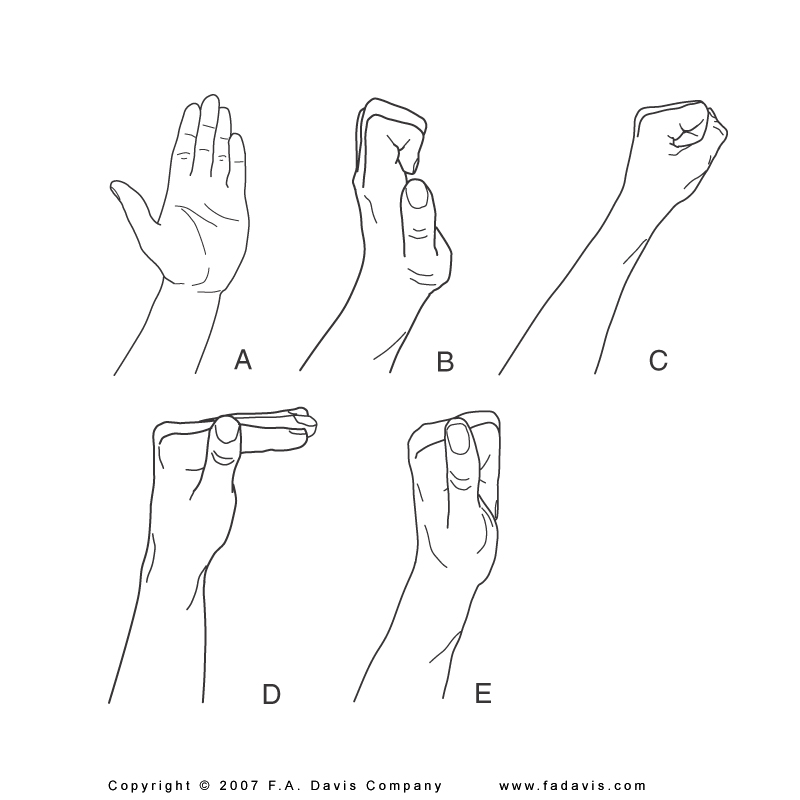
- Flexor Tendon-Gliding Exercises. The illustrated exercises below progressively challenge movement of the flexor tendons:
- Straight Hand
- Ape hand or claw hand
- Full fist
- Table top
- Straight fist
Return to Function
- Ergonomic assessment for injury/reinjury prevention
- Screen for future fall risk and coordinate recommendations with PT and health care team (e.g., considerations for home safety assessment)
Hand Return to Function
Active learning
- You will be tested on your ability to correctly describe precautions and stretches (stretch position and stretch selection)
- Perform strengthening exercises to reinforce your understanding of hand position and motions for specific muscle groups. For example, you should be able to correctly describe the point of manual resistance (i.e., dorsal, volar, etc) to activate muscles of the wrist and hand.
- Pertinent stretch and exercise material is found in Dutton, pages 557-564 (pay special attention to 564) and 579-581. You should also be able to identify where to apply appropriate resistance for general strengthening of flexors, extensors, radial deviators, etc.
End of Lesson

_553.jpg)