Gait Training with Ambulation Aids
PTA 104L Orthopedic Dysfunctions Lab
Many orthopedic conditions result in impaired gait. Deconditioning, weakness, pain, postural imbalances, and loss of joint mobility are some of the factors that impair safety, efficiency, and effectiveness of ambulation. PTAs apply knowledge of pathology, kinesiology and therapeutic exercise through progressive gait training techniques.
Ambulation aids are an invaluable tool to restoring functional ambulation. Selection of the most appropriate device is determined by medical status and patient goals. PTAs integrate body mechanics, motor learning principles, and safety awareness into mobility training interventions according to the plan of care.
Ambulation aids fitted correctly can allow patients/clients with chronic conditions can conserve energy and maximize participation with mobility. Individuals who are rehabilitating from illness or injury can increase strength, endurance, and confidence throughout the stages of healing and recovery.
This lesson reviews the basic components of the normal gait cycle, pre-ambulation considerations, and safe, effective techniques for gait training.
Activities in this lesson will apply directly to practice activities in lab. A successful student will complete pre-lab assignments and activities before coming to lab. Your lab partner(s) will appreciate working with someone who is prepared to be safe.
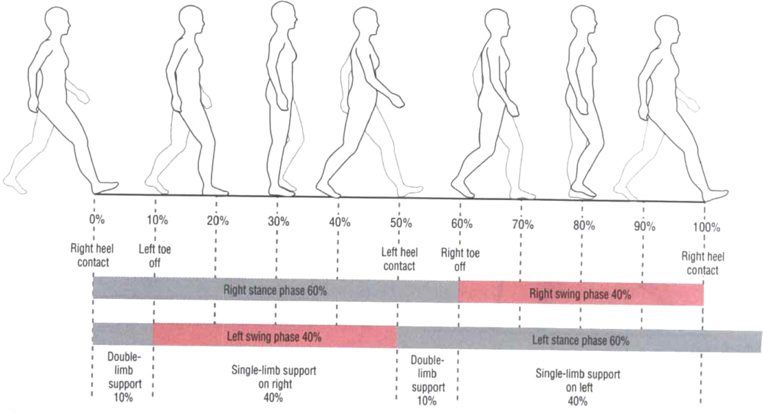
Stance phase: foot is in contact with the ground
subphases are
initial contact (heel strike/contact)
loading response
midstance (foot flat)
terminal stance (heel off)
preswing (toe off).
Swing phase: foot is in the air
subphases are
initial swing (acceleration)
midswing
terminal swing (deceleration).
Pierson, Frank M.. Principles & Techniques of Patient Care, 4th Edition. Saunders Book Company, 092007. 9.3.

Ambulation aides are designed to increase the base of support for standing and walking activities. Torque and other joint stresses can be minimized with an effective use of an ambulation aid. Selection of the most appropriate device is dependent on stability and mobility needs. Overall, ambulation aids can
The term "assistive device" can be substituted for ambulation aid, however, it is less specific and needs to be supported by language and instruction specific to its use in gait training.
Tilt tables may be indicated when the patient has experience extended bed rest, or if there are contraindications for joint motion(s). Gravity can be incrementally applied, resulting in increased demand to the cardiopulmonary system and postural muscles. Ankle plantar flexors and foot instrinsics are passively stretched and proprioception increases through WB in the feet.
Parallel bars can be fixed or folding are are most often found used in rehabilitation settings. Patients who have low endurance or need a significant amount of assistant to rise to sitting. The fixed nature of the bars can allow the patient to pull with the upper extremities when transitioning to standing.
Ambulation aids are organized on the table based on progressively increasing patient mobility/safety levels. In the clinical setting, patients may be progressed through all of these devices. PTAs can select/modify the assistive device to meet the needs of the patient. Abrupt changes in mobility status (e.g., declines) must be communicated to the PT for reassessment and treatment planning
|
Ambulation Aid |
Types |
Advantages |
Disadvantages |
|
Tilt-table |
-- |
Allows for progressive transition to upright position; can adapt for NWB situations |
Dependent; tilt is functional up to ~70 degrees |
|
Parallel Bars |
Folding Floor Mounted
|
Allows for maximum stability, support and safety in a functional position |
Some challenge with body mechanics by PT/PTA Stability may be challenged with larger/weaker patients |
|
Walkers
|
Front-Wheel Standard or Pick-up Four-Wheel Hemi |
Allows for maximal stability for ambulation/gait training; Potential to increase mobility in community Adjustable Some fold |
Some environmental limitations
Walking speed is slower Challenging to use with stairs
|
|
Axillary Crutches |
Wood Aluminum |
Allows for increased variability in gait patterns Provides support with increasing mobility adjustable Can be used on stairs |
Less stable Requires relatively good trunk and UE strength Risk for nerve/vessel damage with improper fit/use |
|
Forearm Crutches |
Lofstrand Canadian |
Allows for increased mobility in patients who are unable to use a cane adjustable Functional on stairs and in narrow areas |
Forearm cuff can make it difficult to remove crutch Dynamic qualities may make some patients feel insecure (e.g., elderly) |
|
Quad Cane |
Crab Large Base (LBQC) Small Base (SBQC) |
Provide a broad base with four points of contact on floor Height adjustable |
Can feel unstable with transitioning weight through the device; Results in a slower gait pattern |
|
Cane |
Wood (standard) Aluminum Offset handle Pistol grip
|
Allows for progressive increased mobility Used for added stability during upright activities Aluminum varieties are easily adjusted Offset handle allows for weight distribution through shaft of cane Less environmental constraints; easily stored Inexpensive |
Standard variety is not adjustable; must be cut to fit patient Function is to widen BOS and improve balance Relatively small BOS compared to other AD Unable to use with 3-point gait pattern |
Specific guidelines for each ambulation aid are provided in Procedure 9-2 in Therapeutic Exercises (pg. 225)
Gait patterns are determined by the patient's status ( WB restrictions, musculoskeletal/neuromuscular impairments, safety) and the environmental constraints. As we discuss weight bearing status, we will integrate specific gait patterns to address the stability, mobility and safety needs of the patient.
Weight bearing status can be physician ordered, established by the PT, and/or modified during treatment based on the patient response. A physician's order for weight bearing status is in place until changed/updated by the MD/PCP. Radiographic or other diagnostic imaging, mobility status, and patient response (pain, safety) are all considered in clinical decision making for weight bearing activities.
A patient information sheet is included in this course to provide you with some patient-based descriptions of weight bearing status. Refer to your text for detailed definitions and use the table below to help summarize descriptions and gait pattern indications.
|
Weight bearing status |
Description |
Gait Pattern |
Pattern description |
|
NWB |
No weight on the extremity |
Three-Point |
Use of walker or two crutches; Step to Step through Aid is advanced alternately with affected limb |
|
PWB, also TTWB TDWB |
Partial weight bearing |
Three-One-Point |
Use of walker or two crutches; Heel touch or flat foot with a fixed or proprioceptively-determined amount of WB in the affected limb Aid is advanced simultaneously with affected limb |
|
WBAT |
Weight bearing As tolerated |
Three-One-Point, Four point, or two point (progress from most to least support from aid)
|
Use of walker or bilateral ambulation aids (crutches, canes); progression to more reciprocal pattern is dependent on patient safety, strength, confidence, and symptoms |
|
FWB |
Full weight bearing |
Four point, or two point |
Use of walker or bilateral ambulation aid Reciprocal pattern (slow to fast progression) |
|
Unequal WB |
Hemi pattern |
Modified four-point Modified two-point |
Use of one ambulation aid (crutch, cane, hemi walker) or for patients with functional use of one upper extremity LE and aid advance alternately (four-point) or simultaneously (two-point) ; aid is typically used on the contralateral side |
Use a patient-centered approach to critically assess which side of the body will most benefit from the cane. Specific considerations include:
Various patient handouts for sequencing gait with a variety of assistive devices and on a variety of terrains are available on the University of Pittsburgh Medical Center Patient Education Materials page
We will be practicing gait training in lab. Be prepared with appropriate footwear and clothing.