
PTA103Neuromuscular ConditionsW2021
PTA 103 Intro to Clinical Practice 2
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment. Marc Duyck PTA, MEd. CSCS

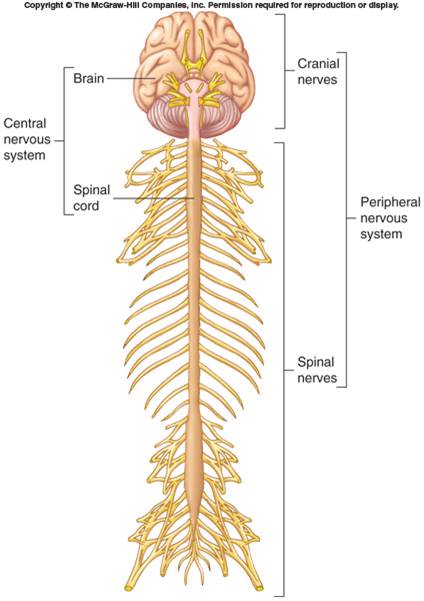
Image is of a brain and spinal cord
Image is of a neuron that is sending signals to other neurons
Here is a screen-cast introduction to this lesson builder
Readings:
Fun
In order to understand what can go wrong, we need to know what normal function looks like. It is easier to understand signs and symptoms of disease when you can reference the involved structures and processes. PT interventions, tests, and measures become more meaningful when you have a general understanding of deficits and potential for rehabilitation.
1. Sensory: Monitor internal and external stimuli
2. Integration: Brain and spinal cord process sensory input and initiate responses
3. Control: Muscles and glands
4. Homeostasis: Regulate and coordinate physiology
5. Mental activity: Consciousness, thinking, memory, emotion
![]()
Concepts and Terminology to Learn
Components on the Nervous System
–Brain, spinal cord, nerves, sensory receptors
Subdivisions
–Central nervous system (CNS): brain and spinal cord
–Peripheral nervous system (PNS): sensory receptors and nerves
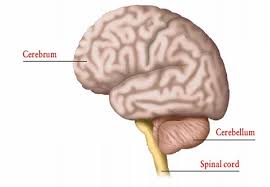
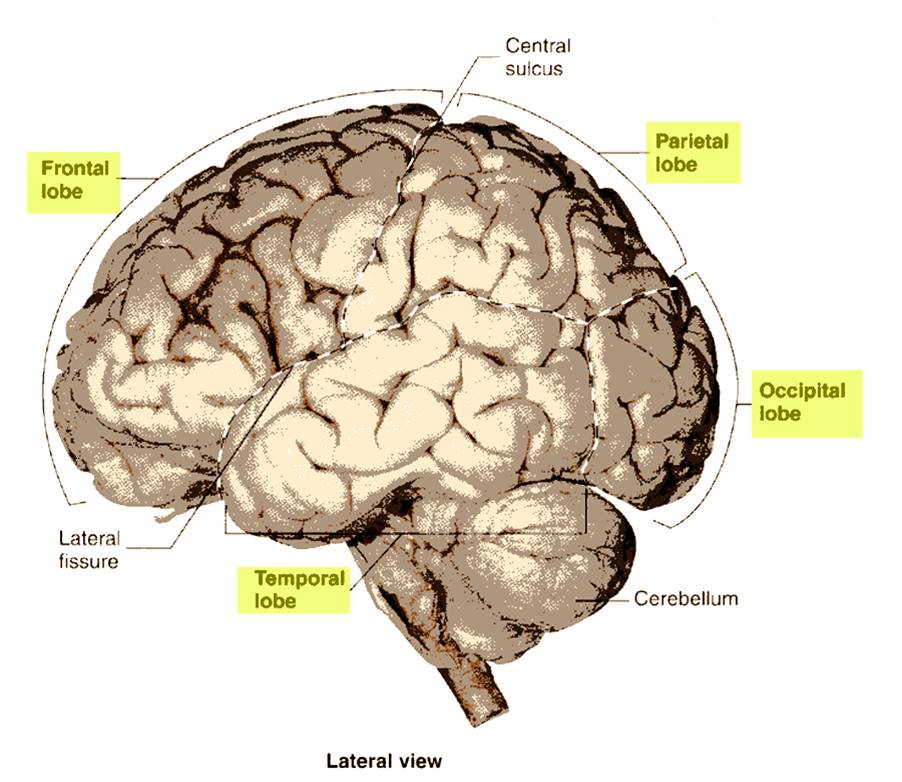
Brain
•Part of CNS contained in cranial cavity
•Control center for many of body's functions
Parts of the brain
•Cerebrum/cerebral cortex: conscious thought, control
•Brainstem: connects spinal cord to brain; integration of reflexes necessary for survival
•Cerebellum: involved in control of locomotion, balance, posture
•Diencephalon: thalamus, subthalamus, epithalamus, hypothalamus
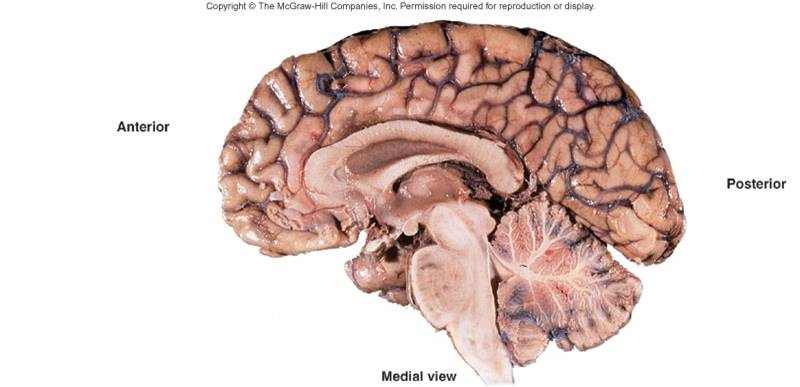
Cerebrum
•Largest portion of brain
•Composed of right and left hemispheres each of which has the following lobes: frontal, parietal, occipital, temporal, limbic, insular
Cerebral Lobes
•Frontal: executor of function: voluntary motor function, motivation, aggression, sense of smell, mood
•Parietal: sensory integrator for pain, temperature, detection of taste, and touch; coordinates reading
•Temporal: Reception and evaluation for smell and hearing; memory, abstract thought, judgment; Insula is within temporal lobe.
•Occipital: reception and integration of visual input
•Central sulcus: between the pre central gyrus/primary motor cortex and post central gyrus/primary somatic sensory cortex
Limbic System
•Part of cerebrum and diencephalon
•Basic survival functions such as memory, reproduction, nutrition
•Emotions
•Various nuclei of the thalamus
•Part of the basal nuclei, hypothalamus, olfactory cortex, fornix
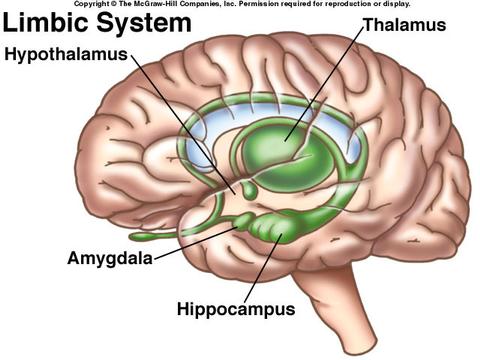
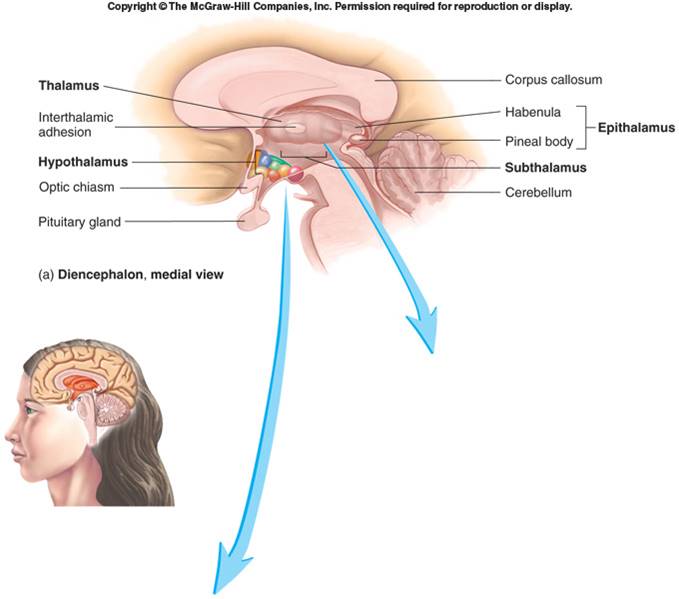
•Sensory information from spinal cord synapses here before projecting to cerebrum
•Relay information to motor, mood, emotion, and sensory integration areas in the cerebral cortex
•Involved in controlling motor function
•Contains subthalamic nuclei, parts of red nuclei and substantia nigra.
•Several ascending and descending nerve tracts
![]()
•Pineal gland
•Most inferior portion of diencephalon
•olfactory reflexes and emotional responses to odors
•Controls endocrine system.
•Receives input from viscera, taste receptors, limbic system, nipples, external genitalia, prefrontal cortex
•Efferent fibers to brainstem, spinal cord (autonomic system), to posterior pituitary, and to cranial nerves controlling swallowing and shivering
•Important in regulation of mood, emotion, sexual pleasure, satiation, rage, and fear
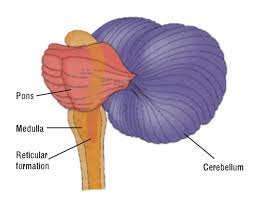
•Comprised of midbrain, pons, and medulla oblongata.
•Considered Peripheral Nervous System (PNS)
•These peripheral nerves originate from brain.
•Two pairs arise from cerebrum; ten pairs arise from brainstem
A pontine CVA is a stroke involving the brainstem.
•Continuous with spinal cord; has both ascending and descending nerve tracts
•Regulates: sleep, heart rate, blood vessel diameter, respiration, swallowing, vomiting, hiccupping, coughing, and sneezing
![]()
![]()
Crainial Nerves
•Indicated by
•May have one or more of three functions
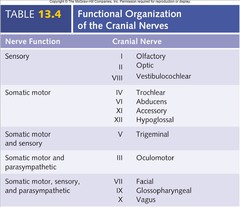
Trigeminal Nerve
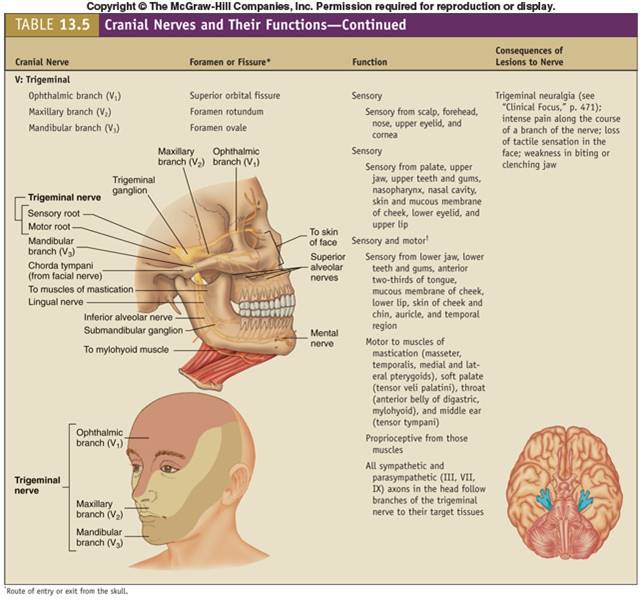
•Finger-to-nose test: what this is testing is coordination ruling out ataxia. If a pt had an impaired finger to nose test, the PTA would not interpret meaning, but give/chart this information as impaired or not impaired and share results with the supervising PT.
Cerebrum versus Brainstem
The two systems interact in automatic and conscious ways throughout the life cycle
•Anterior Cerebral Artery (ACA)
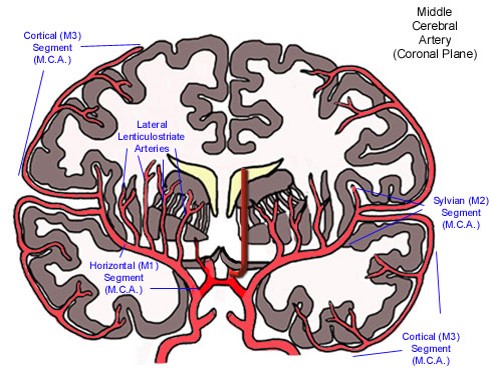
•Middle Cerebral Artery (MCA)
•Posterior Cerebral Artery (PCA)
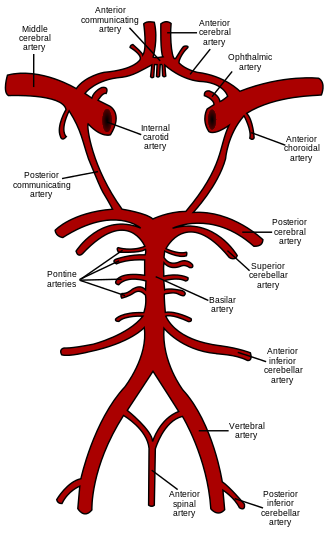
Image is of the various arteries that supply blood to the brain
–Includes anterior inferior cerebellar artery (AICA), superior cerebellar artery
–Supplies pons and cerebellum
–Primary blood supply to midbrain
–Complete occlusion can be fatal
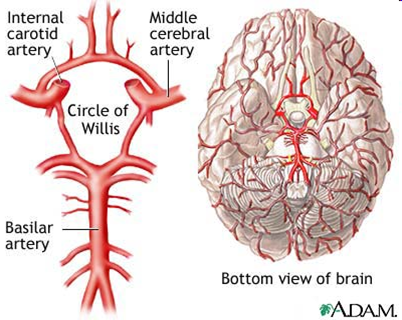
•Ring of 9 arteries
•Provides multiple sources of circulation/blood supply to the cerebrum
–Carry one-third of blood supply to the brain
–Originate from the subclavian artery
–Branches into three parts
–All three branches supply blood to medulla
–PICA supplies inferior cerebellum
–Originate from the common carotid
–Becomes the posterior communicating arteries (PCA)
–Divides into anterior and middle cerebral arteries
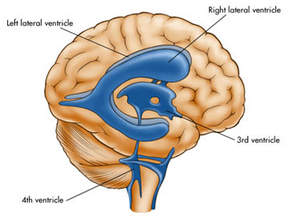
Ventricles are interconnected by aqueducts and wall openings
Blockage in the central canal or fourth ventricle can lead to hydrocephalus (enlarging ventricles) and may require an external shunt for treatment
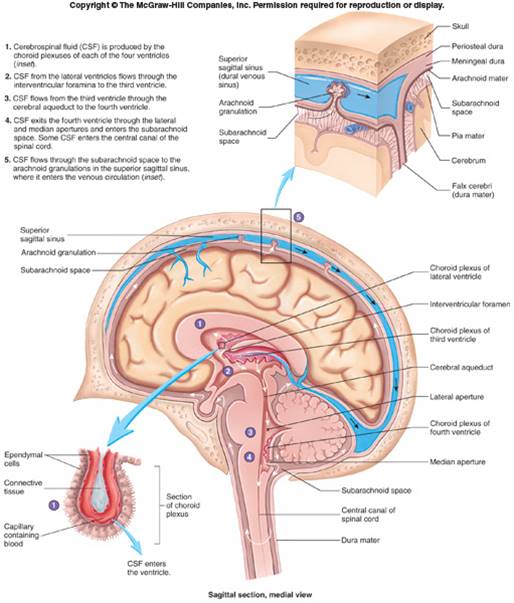
CSF
Similar to serum, but most protein removed
Composed of ependymal cells, their support tissue, and associated blood vessels
Blood-cerebrospinal fluid barrier
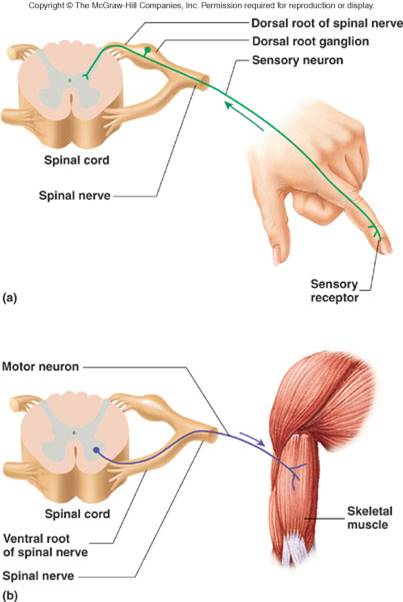
Peripheral nervous system image is of a sensory and afferent: action potentials toward CNS
•Functional classification
•Structural classification
Most nerves contain a mixture of neurons
Afferent pathways: sensory responses from the periphery (touch, position, pain)
Efferent pathways: motor responses from the center/spinal cord to the periphery
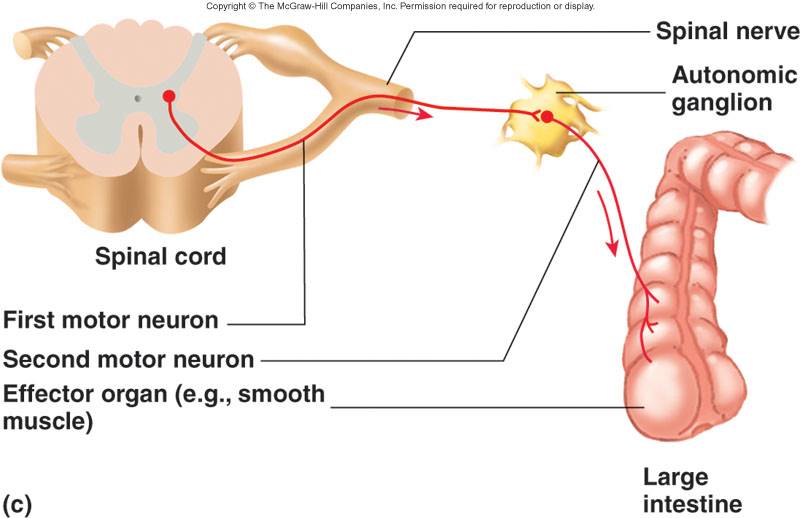
Organs receive dual innervations from both sympathetic and parasympathetic branches to maintain homeostasis
Divisions of ANS
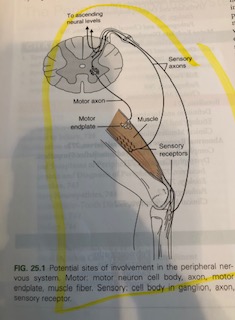
Connection between the PNS and ANS broken down.
Take home message:Example: If while chewing/digesting an orange (ANS/parasympathetic branch), I receive a stimulus such as noxious heat from a stove to my finger/part of the peripheral nervous system, a response occurs involving sensory receptors (heat to my fingers) and a motor response (motor axon to motor endplate) when I pull my finger off of the stove. In the meantime my ANS is stimulated specifically the parasympathetic branch, and my digestion stops because my ANS and PNS communicate and right now the focus is getting my finger away from the noxious heat/stove!
Image is of a neuron that is excited and communicating with other neurons!

Image is of an older adult
Decreased sensory receptors on skin
ANS Parasympathetic Responses: Changes in Bowel/bladder, BP regulation, H20 regulation
.
|
Class |
Description |
Risk Factors |
Common Symptoms |
Examples |
|
Upper Motor Neuron Disease |
Lesions in descending motor tracts Includes the cerebral cortex, internal capsule, brainstem, and spinal cord |
Hemodynamic compromise Diabetes Cardiovascular disease Advanced age Closed head injury Arteriovenous malformation |
Weakness of many involved muscles Hypertonicity (increase in muscle tone) Hyperreflexia (exaggerated responses of spinal reflexes) Pathological reflexes Spasticity |
Cerebral Vascular Accident (CVA) ("stroke")
Cerebral Palsy Spinal Cord Injury Multiple Sclerosis Amytrophic Lateral Sclerosis (ALS) is classified as an upper and lower motor neuron lesion disease
|
|
Lower Motor Neuron Disease |
Lesions involving nerves and axons at or below the alpha motor neurons |
Under investigation Suggested linkages include genetic and environmental triggers |
Weakness of single or multiple involved muscles Hypotonicity (decrease in muscle tone) Fasciculations (small, local, involuntary contractions) Muscle atrophy Decreased or absent reflexes |
Amytrophic Lateral Sclerosis (ALS) is classified as an upper and lower motor neuron lesion disease
Myasthenia Gravis Guillain-Barre Syndrome |
|
Disorders of the Basal Ganglia |
Lesion of specific deep nuclei (centers) in the brain Characterized by either 1) large involuntary movements (dyskinesias) or 2) abnormal static postures (akinesias) |
Under investigation. Hereditary factors; Long-term use of anti-psychotics |
Dyskinesias Resting tremor Athetosis (slow, involuntary, writhing, twisting movement) Chorea (involuntary, continuous, rapid, irregular and jerky movements) Akinesias Rigidity (resistance to passive movement of the limb) Dystonia (involuntary adoption of abnormal postures) Bradykinesia (decreased amplitude and velocity of movement; slowed movements)
|
Parkinson's Disease Huntington's Disease
|
|
Disorders of Cerebellum |
Lesion in the cerebellum |
Much like CVA risk factors Congenital malformation Genetic contributors |
Changes are ipsilateral (same side) Ataxia Dysmetria Dysdiadochokinesia Hypotonia Speech changes
|
Cerebellar stroke Ataxia disorders |
|
Peripheral nerve disorders |
Localized or diffuse trauma to the nerve structure |
Repetitive use Traction (stretching forces) from trauma Difficult birth or can occur during pregnancy (Linder, 1997) Prolonged compression |
Weakness in select muscle groups Atrophy Persistent pain |
Carpal tunnel syndrome Tarsal tunnel syndrome Diabetic neuropathy |
|
Ischemic |
Hemorrhagic |
|
Most common (about 80% incidence) |
Less common 20% occurrence |
|
Caused by emboli or arterial narrowing |
Caused by rupture of vessels
|
|
Damage follows vascular distribution
|
Damage can extend into multiple vascular territories
|
|
Symptoms of stroke develop and worsen over time
|
Symptoms are usually sudden
|
|
Warning symptoms (changes in vision, balance, cognition, speech) often precede ischemic stroke |
Warning symptoms (vomiting, severe headache, impaired consciousness) often precede hemorrhagic stroke |
|
Impairments are somewhat predictable |
Impairments will vary with the individual and size
|
Most CVAs occur due to a blockage or bleeding in the middle cerebral artery. The vessel in red illustrates the distribution of the middle cerebral artery and its respective branches.
Common characteristics of cerebral CVA are:
|
Right CVA |
Left CVA |
|
L sided paresis (neurological weakness)
|
R sided paresis (neurological weakness)
|
|
Decreased attention span selective awareness of the environment or responsiveness to a stimulus or task without being distracted by other stimuli
|
Decreased initiation of tasks
|
|
Decreased awareness and judgment
|
Decreased R and L discrimination
|
|
Memory deficits
|
Dysphagia - impairment of strength and coordination of chewing and swallowing
|
|
L hemianopsia - loss of left half of the visual field
|
R hemianopsia - loss of right half of the visual field
|
|
L inattention
|
Increased frustration
|
|
Decreased abstract reasoning
|
Apraxia - inability to perform skilled purposeful movements
|
|
Emotional lability
|
Aphasia - inability to produce functional (expressive) or integrate (receptive) speech
|
|
Impulsivity
|
Compulsive behavior
|
|
Decreased spatial orientation
|
|
![]()
![]()
![]()
![]()
![]()
The Guide to Physical Therapy Practice frames seven, impairment-based patterns that are consistent with patients and clients encountered in the physical therapy service. The language in practice patterns reflects the commitment to documenting and tracking how a person functions within their disease versus focusing on the disease.
Physical Therapy practice patterns connect affected body structures and functions with outcomes in the examination process. The result is a clear application of the International Classification of Functioning, Disability, and Health (ICF) which aids in evidence-based treatment planning. Within practice patterns, the physical therapist evaluates how body systems and conditions and the associated impairments impact function and disability within the patient's individual circumstance.
The table below outlines how physical therapy approaches establishing a PT diagnosis. A PT prognosis will factor in specific patient situations and circumstances (such as co morbidities, support systems, etc., work/home activities) in order to set treatment goals, frequency and duration.
|
Practice Pattern |
Practice Pattern Description |
Example Diagnoses |
|
Pattern A
|
Impaired Motor Function and Sensory Integrity Associated With Congenital or Acquired Disorders of the Central Nervous System in Infancy, Childhood, and Adolescence
|
Cerebral Palsy (CP) Spina Bifida Myelomeningocele Spastic Hemiplegia Spastic Diplegia Epilepsy Autism Spectrum Disorders Fetal Alcohol Syndrome |
|
Pattern B
|
Impaired Motor Function and Sensory Integrity Associated With Acquired Non progressive Disorders of the Central Nervous System in Adulthood
|
Traumatic Brain Injury (TBI) Cerebral Vascular Accident (CVA) Transient Ischemic Attack (TIA) Burns |
|
Pattern C
|
Impaired Motor Function and Sensory Integrity Associated With Progressive Disorders of the Central Nervous System in Adulthood
|
Multiple Sclerosis (MS) Amyotrophic Lateral Sclerosis (ALS) Parkinson's Disease (PD) Myasthenia Gravis Huntington's Disease Alzheimer's Disease |
|
Pattern D
|
Impaired Motor Function and Sensory Integrity Associated With Peripheral Nerve Injury
|
Ischemic compression stretch inflammation chemotoxicity |
|
Pattern E
|
Impaired Motor Function and Sensory Integrity Associated With Acute or Chronic Polyneuropathies
|
Guillain-Barré Syndrome (GBS) Autoimmune diseases Diabetic Neuropathy Alcoholism Nutritional Deficits (e.g, B12) Infection (Herpes, Polio) |
|
Pattern F
|
Impaired Motor Function and Sensory Integrity Associated With Non progressive Disorders of the Spinal Cord
|
Spinal Cord Injury (SCI) Degenerative Joint/Disc Disease in Spine |
|
Pattern G
|
Impaired Arousal, Range of Motion, Sensory Integrity, and Motor Control Associated With Coma, Near Coma, or Vegetative State
|
Minimally Responsive State Anoxic Brain Injury Toxicity or Metabolic Dysfunction |
Many providers are involved in coordinating care for patients and clients with neuromuscular dysfunction. All health care providers share a commitment to patient and family education and patient-centered practice. Examples of providers and some of their focused scope of practice include:

Image is of a PT evaluating a pt with a
neurological condition
Key elements of a physical therapy examination includes
![]()
![]()
Tests and measures provide data that informs the physical therapy plan of care. Outcomes of tests and measures may prompt communication with the supervising PT and other health care personnel, particularly when there are marked changes over time that suggest a need for care plan review or emergency action. Examples of common tests and measures in this population include:

Image is of an adult with a spinal cord injury
|
The Functional Independence Measure is an interdisciplinary measure of function. It may be scored entirely by a nurse from information provided in the medical record and treatment notes.
Typically, the PT team member will be responsible for rating mobility and locomotion. Nursing and/or nursing will rate the self-care items. Nursing or speech language pathology will rate communication problems and cognitive function. Psychosocial status may be a collaborative process and based on consensus from team members.
Levels of Assistance |
||||
|
LEVEL |
ABBREVIATION |
FIM LEVEL |
DEFINITION |
NO HELPER |
|
Complete Independence |
I |
7 |
All tasks are performed safely without modification, assistive devices or aids and within reasonable time |
|
|
Modified Independence |
Mod. I |
6 |
One or more of the following are true about the activity: --requires assistive device --takes more than reasonable time --there are safety (risk) concerns |
|
|
Stand by Assistance
Supervision or Set-up |
SBA Or S |
5 |
Requires no more than standby, cueing or coaxing without physical contact or helper sets up needed items or applies orthoses |
HELPER |
|
Contact guard assistance |
CGA |
4 |
Variation of minimal contact assist where subject requires contact to maintain balance or dynamic stability |
|
|
Minimal contact assistance or minimal assistance |
Min contact A Or Min A |
4 |
Requires no more than touching & expends 75+% or more of the effort; assistance is needed to lift one limb |
|
|
Moderate assistance |
Mod A |
3 |
Requires more help than touching or expends 51% to 75% of the effort; assistance is needed to lift two limbs |
|
|
Maximal assistance |
Max A |
2 |
Subject expends 26% to 50% of effort |
|
|
Total assistance |
Total A |
1 |
Subject expends less than 25% of effort; two or more provide assistance |
|

Image is of a physical therapist assistant working with a RN
in the care of a person with a neurological health condition
Key terms for understanding descriptions of neuromuscular conditions are listed below. They are used throughout your text resources and in medical records. Refer to this list during lecture presentations and course reading in order to differentiate between signs and symptoms of neurological and neuromuscular conditions
Terms associated with impairments and dysfunction of the neuromuscular system
1. Muscle groups working together to perform a task during a voluntary movement (timing, accuracy, sequence) = synergy.
2. Level of skill and efficiency of movement with the nervous system as a key variable.
3. Start, control and stop muscle activity according to activity/environment demand with the nervous system as a key variable to accomplish the task.
References:
Cameron. M. 2011. Physical Rehabilitation for the PTA. Elsevier. MO
Goodman. C. 2018 Pathology for the PTA. 2nd Edition. Elsevier. MO.
Linder, A. et al. 1997. Postpartum obturator nerve syndrome: case report and review of the nerve compression syndrome during pregnancy.
Zentralbl Gynakol1997;119(3):93-9