 http://nothings.livejournal.com/222931.html
http://nothings.livejournal.com/222931.htmlPosture and Body Mechanics
PTA 101 Intro to Clinical Practice 1
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Specific Lesson Level Objectives include:
 http://nothings.livejournal.com/222931.html
http://nothings.livejournal.com/222931.html
The supervising PT may indicate "impaired posture" in a patient problem list and include goals related to posture (static and dynamic) in the plan of care.
For example, a patient with a medical diagnosis (pathology) of osteoporosis may present with impaired posture (increased thoracic kyphosis), which impacts pain and endurance for standing and walking.
Treatments for impaired posture include effecting a change in muscle length and strength and adapting for fixed, structural changes.
Muscles change length and muscle fiber type changes over time due to habitual postures, under use and misuse of structures. Shortened muscles become stiffer, less likely to respond to stretch, and the cycle continues.
A little asymmetry is normal. For example, in standing the dominant hand (i.e., left or right handed) is typically lower with reference to the acromion than the non-dominant hand. This is generally attributed to more developed (i.e., larger) muscles on the dominant side. This can then be compensated for by a higher pelvis on the non-dominant side.
Many large muscles cross multiple joints. Therefore, an over-lengthened or shortened muscle can influence the resting postions throughout the spine, pelvis and extremities.
Common faulty postures include: kyphosis-lordosis, sway back, and flat back
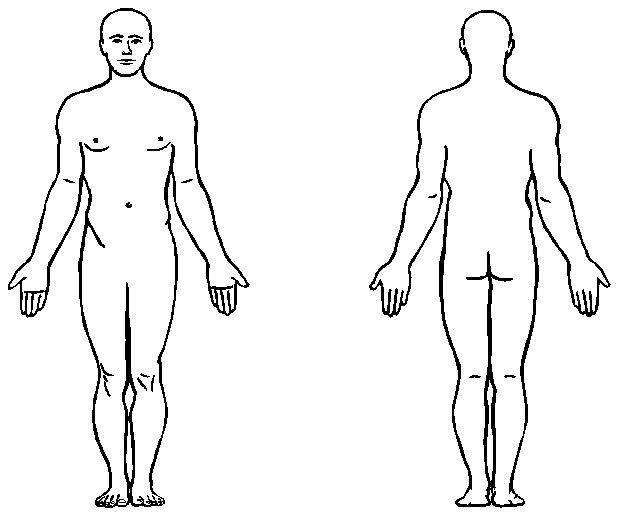
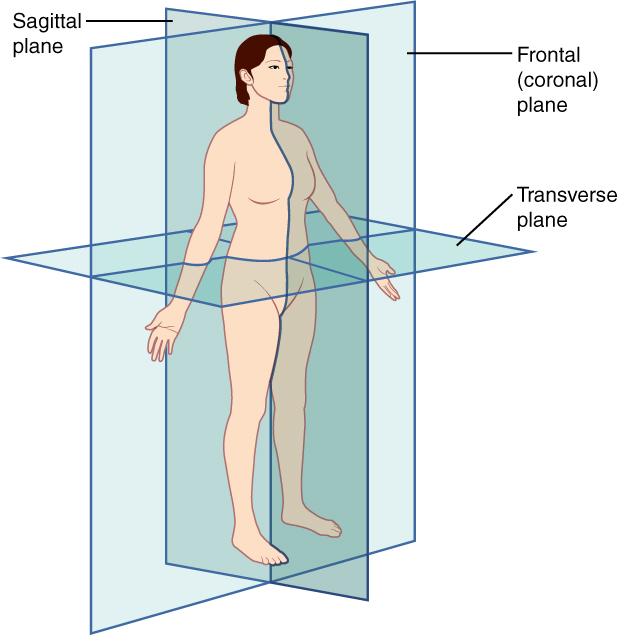
Active Learning: See if you can apply your knowledge of anatomical planes and observational skills to describing changes at the spine, head and lower extremity
Click here for an example of how posturography is used with tablet applications (e.g. PostureScreen) to assist in assessing posture. How would you document your observations of these postural asymmetries?
![]()
![]()
Specific interventions for posture are introduced in Kinesiology. In this class, we set the foundation for postural assessment by ensuring you are able to recall anatomical planes, movement planes, and begin working on observation and documentation of those observations in static (non-moving) positions.
Posture is a component of every PT examination, regardless of pathology. The PT is responsible for establishing or elaborating on movement/activity precautions, contraindications, safety considerations, and differentially diagnosing the role of posture as a primary impairment contributing to functional limitations and disability. The PT documents postural observations in supine, sitting, standing, and/or functional activities depending on the patient's level of function at the time of the assessment. Muscle atrophy, hypertrophy, spasm and symmetry are noted, along with the postural impacts of ligamentous laxity, footwear, and assistive devices.
PTAs review the medical record and reassess posture using observations and patient instruction.
PTAs follow up on safety considerations and evaluate the patient and situation for ability to safely participate in postural interventions
PTAs can assess muscle length using multiple intervention strategies. PTAs provide exercise instruction, make recommendations for activity, equipment and workplace modifications in order to optimally affect modifiable contributors while minimizing stress to non-modifiable contributors to impaired posture.
PTAs make comparisons between the patient's current status and their baseline postural examination in order to determine if there is progress or if there is some barrier to progress which required further assessment by the supervising PT. PTAs actively listen to patients and relay information (through documentation and meetings) about additional contextual factors impacting progress.
PTAs document preferred posture and postural observations using appropriate medical terminology. PTAs document progress toward postural goals so the PT and the health care team are well-informed of the patient's participation, response, compliance, and safety throughout the treatment plan.
Boxes 4.5 through 4.9 in Pierson outline some clinical examples of how principles of postural control are integrated into patient education and exercise recommendations.
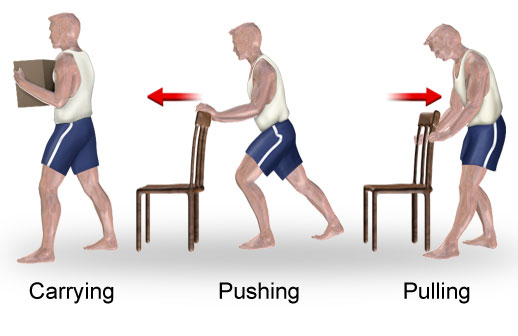
"Body mechanics can be described as the use of one's body to produce motion that is safe, energy conserving, and anatomically and physiologically efficient and maintains body balance and control." - Pierson & Fairchild, Principles and Techniques of Patient Care, 5th Ed.
PTs and PTAs apply their knowledge of posture and how forces act on the body to teach and practice proper body mechanics. Why? Because PTs and PTA do a lot of lifting, stooping, carrying, bending, standing, kneeling, sitting, and squatting during patient care activities. Our patient's and clients are at risk for injury or reinjury during healing if everyday movements are not balanced and efficient. Repetitive microstrain leads to tissue failure, pain, loss of work, and risk for permanent disability. For a long, successful, and healthy career, we start with learning how to protect ourselves so that we can teach others how to recover from or prevent injury.
For each situation, consider the effects of gravity (VGL) and friction when performing an optimal push, pull, lift, and carry.
Take home messages for body mechanics are succinctly stated in Procedure 4-1 of Pierson
Remember: gravity is POWERFUL. Do what you can to minimize the effects of gravity and you will minimize your risk for injury.

These specific lifting techniques will not be on your exam, yet are listed here for your reference in preparing for lab practice.
|
Lift Type |
Advantages |
Disadvantages |
|
Deep Squat |
Good for light weight objects at floor level Can use one hand to lift and one to stabilize object on thigh |
Challenging if there are hip or knee pathologies |
|
Power Lift |
Good for heavy or bulky objects at knee height (Stoop lift is a power lift when lifting an object from the side) |
May result in strain if there are no handles |
|
Traditional Lift |
A version of power lift where arms bring object close, then legs push up from squat |
Requires increased upper arm strength with abdominal control |
|
Golfer's Lift |
Good for light objects at floor level; object can be lifted with one hand; functional lift when there are painful knees |
Limited to light objects, requires near full WB on one leg; need to place one hand on object or thigh to increase stability |
|
Overhead Lift |
Allows for function |
Requires good upper body strength; increased risk of hyperextension in low back; fall risk |
A little more about overhead lifting
PTs and PTAs assess strength, ROM, motor skills, pain, and function during body mechanics training activities. If proper posture or lifting can not be performed by an individual, we work to modify and accomodate limitations so there is minimal risk for injury and optimal efficiency.
After reviewing proper posture and lifting mechanics, self-assess your own readiness to perform lifting tasks:
If the answer to any of the above is "yes", consult with your instructor prior to engaging in lab practice.
Did you take advantage of the self-checks?
Have you tried the Can You Help Me? forum
Did you check for related assignment due dates and TIMES?
Do you have any other questions? Let us know!