Foundations of Clinical Practice
PTA 101 Introduction to Clinical Practice 1
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions.
Apply problem-solving algorithms accurately during clinical case studies
Describe, select, and apply the PT Management and Disablement models/terminology to clinical cases
Identify the role of the PTA during application of physical therapy interventions covered in this course
Document accurate and thorough treatment information for course specific patient case simulations using SOAP and proper medical format.
In PTA 100, you will learn more about the origins of physical therapy, including the development of the PTA and the PT/PTA team. PTAs are trained to perform physical therapy interventions under the direct supervision of a physical therapist. PTAs engage in critical thinking, data collection, patient education, and discharge planning with the physical therapist. In order to help better understand your clinical role as a PTA, it is important to understand the role of the physical therapist.
Disablement models have been adopted to better describe the impacts of disease on function. This shift from focusing on the disease to the individual and their respective losses in function is a progressive shift toward a patient-centered versus pathology-centered health care.
Physical therapy plays an integral role in customizing a plan of care to meet the needs and goals of the individual based on the multiple impacts of the disease and/or medical condition. Terminology used in the Nagi model is commonly used in physical therapy and health care to describe and track the affects of disease on movement and life roles.
Key terms:
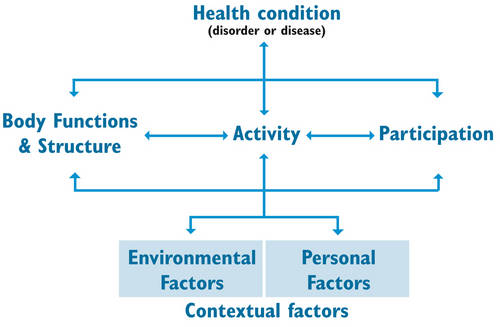
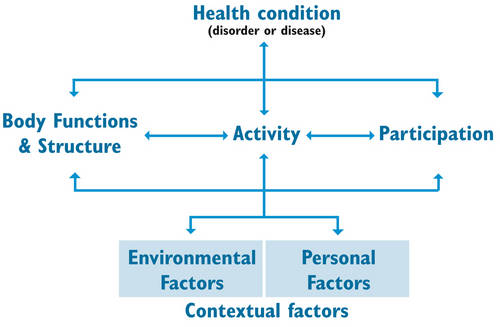
The Nagi Disablement model was adopted early as a means to describe how a disease or a pathology results in impairments, functional limitations, and disability and how this may vary across individuals. More recently, the Nagi Disablement model has been replaced with the World Health Organization (WHO) International Classification of Functioning (ICF) as a means to track how a health condition affects activity.
Key terms:
The International Functional Classification of Disability and Health (ICF) model takes Nagi's patient-centered concept a bit further by expanding on how contextual factors impact activity. This shift in thinking represents an increased focus on how one disease or condition can affect different people in different ways based on the person's unique situation. There is also a focus on improving health vs. disease. In particular the WHO ICF model includes what the person can do (positive impacts) as well as what remains limited (negative impacts).
Test your understanding of Disablement model terminology and classification by working through these self-assessments.
Labeling Activity
Multiple Choice
Physical therapy applies disablement models to clinical practice. By placing the patient at the center of the process, the PT team is always aware that the goals are individualized for each participant.
Physical therapy evaluation and treatment is illustrated and described as the Patient-Client Management Model. Take a moment to review the pathway, starting with examination and read the descriptions of each activity in the client management process.
After completing an examination, evaluating the data and selecting a diagnosis, the PT will develop a plan of care which includes the goals for treatment. It is in the plan of care where the PT selects appropriate interventions to facilitate progress toward patient goals. The PT will delegate appropriate interventions to the PTA and the PTA communicates treatment outcomes and/or any barriers to treatment to the physical therapist.
The plan of care is the road map for the PTA. It is often abbreviated POC. The POC will stipulate the number of visits, how many times a day/week a patient will receive PT, and the types of interventions which will be applied to reach goals.
The examination, evaluation, diagnosis and prognosis are the sole responsibility of the physical therapist.
PTs and PTAs provide skilled interventions and document treatment outcomes.
Let's try and simplify major components of a physical therapy examination. Elements of the Physical Therapy Examination - BSAP
| Background |
Includes patient history, time lines, mechanisms of injury, impairment, functional loss, comorbidities (other disease/health conditions), previous treatment and treatment results, etc). |
| Situation |
Home design and assistance available, work/home demands, supportive and/or adaptive equipment, other potential barriers to care/progress, etc. |
| Assessment |
Physical therapist's opinion of primary and secondary impairment, dysfunction, and/or disability, goals for treatment, prognosis for physical therapy treatment |
| Plan |
Includes frequency and duration of PT interventions to reach PT goals, discharge needs and follow-up referrals or testing. |
![]()
![]()
![]()
Documentation is the universal language of the health care record. Basically, if the treatment is not documented, it never happened.
In this program, we begin right away with introducing the role of documentation. Keep in mind that we will be working throughout the year on the key concepts and essential components of clinical documentation. Initially, you may find the information challenging. Be assured that as we integrate clinical examples in lecture and laboratory practice, you will become more comfortable with applying documentation skills.
Failure to document accurately and thoroughly, using neutral language which is clinically relevant to the case compromised patient safety, outcome measures and the continuum of care. Additionally, inaccurate, inappropriate, or incomplete documentation violates federal law, state practice acts, Medicare guidelines, and Standards for Ethical Conduct.
Be sure to check your study guide for some common abbreviations. We will start using some of these abbreviations in lab and lecture activities, so it will be helpful to keep your own copy for quick and easy reference.

American Physical Therapy Association. (2012). Defensible documentation for patient/client management.
Dutton, M. (2018). Orthopaedics for the Physical Therapist Assistant; Bartlett Publishers.
Gardner, K. (2011). Guide to Physical Therapist Practice.
Jette, A. M. (2006). Toward a common language for function, disability, and health. Physical Therapy (5), 726-734.
Be sure to check Moodle and Moodle calendar for assignments and due dates related to this lecture content.