Foundations of Electrical Stimulation
PTA 101 Intro to Clinical Practice 1
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution for commercial purposes. It is not intended to serve as or take the place of medial advice or treatment.
Contact howardc@lanecc.edu for permission
Electrical stimulation use dates back to ancient time when electric eels were used to treat painful spines and limbs. In this lesson, we will study characteristics of electricity, electricity effects in biological tissue, and its use in rehabilitation. By understanding how electrical stimulation effects muscle and nerve function, we can safely and effectively select the most appropriate "estim" to maximize patient progress toward goals in the plan of care.
After completing this lesson, the successful student will be able to:
All use of electricity to produce a change in body tissue is directly related to the properties of the cell membrane. Electricity can stimulate ionic flow, and therefore action potentials, which result in activation of nerve pathways, muscle tissue, and chemical changes
Review the process of an action potential at the cell membrane.
(Approximately 7 minutes)
This will refresh your understanding of cellular physiology and help make connections between physiology and electrical stimulation as a rehabilitation modality
Approximately 9 minutes
Approximately 3 minutes
This excerpt from the American Society of Neurological Monitoring has one of the best explanations I've seen to help understand ionic flow in biological tissue:
"How an Electrical Stimulator Works
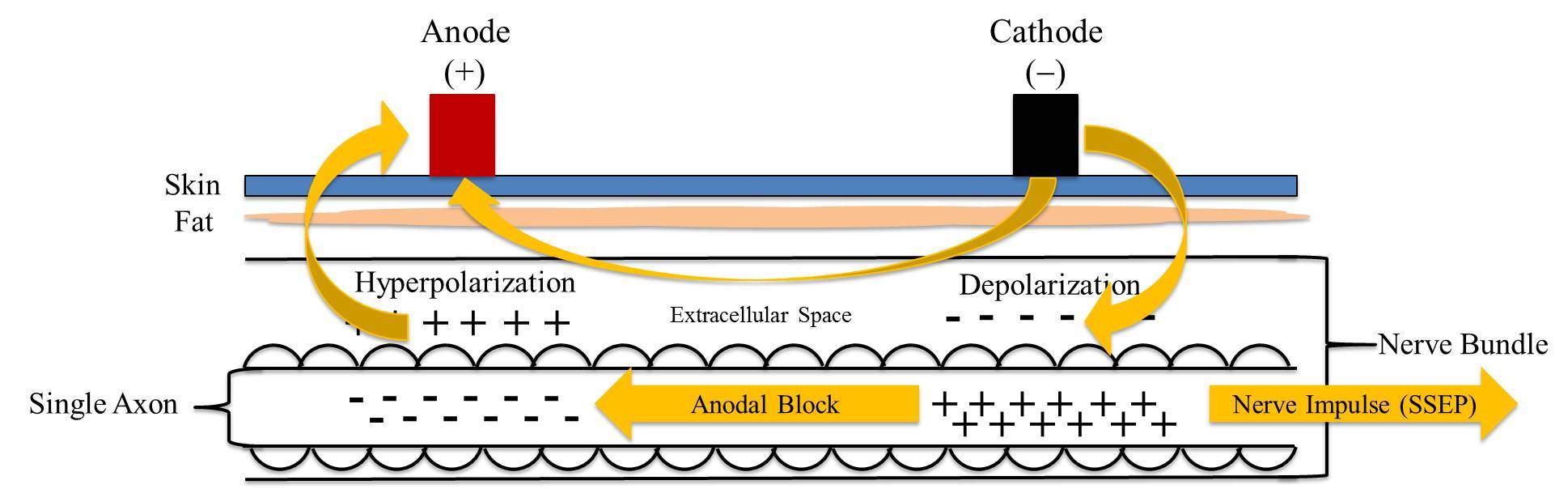
In an electrical stimulator, the flow of anions (-) and cations (+) is controlled by the mechanics of the circuitry within the stimulator. The stimulator is unique in that the cathode is the negative pole (-) because it discharges anions (-), and the anode is the positive pole (+) because it discharges cations (+). At the end of the day, that's the fundamental difference between a battery and a stimulator.
Depending on how we configure the polarity, the stimulator will discharge either cations or anions into the body part being stimulated.
In cathodal stimulation, anions (-) are discharged into the body as current flows from the cathode (-), through the tissue, and back to the anode (+).
In anodal stimulation, cations (+) are discharged into the body as current flows from the anode (+), through the tissue, and back to the cathode (-).
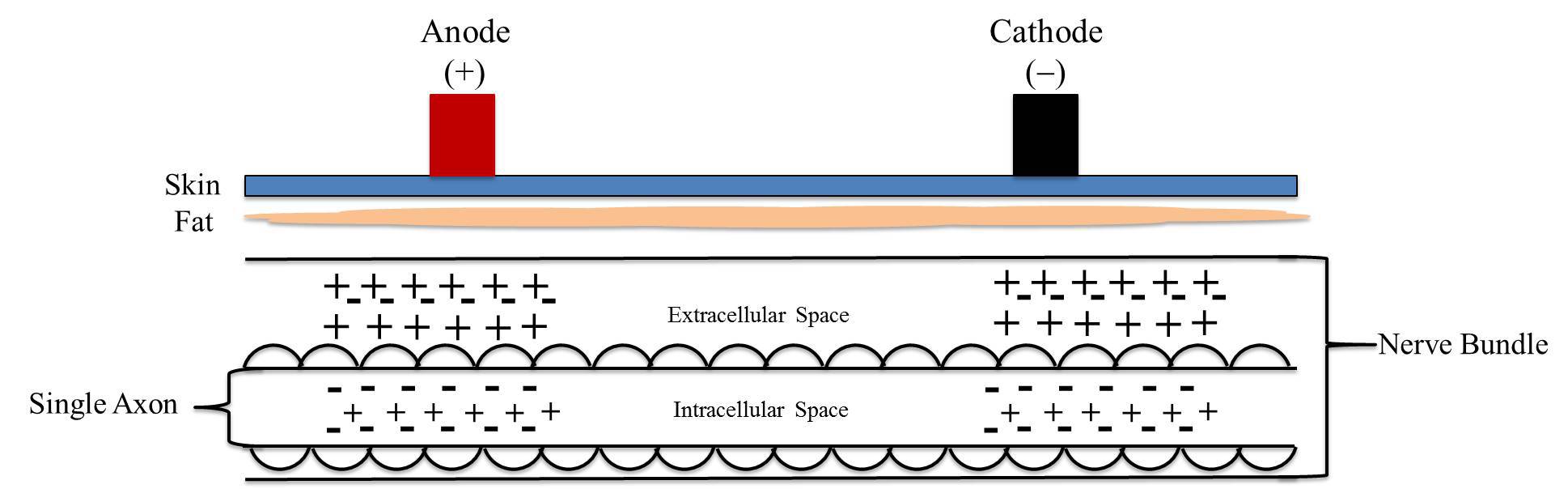
Now, let's imagine that we place an electrical stimulator on the surface of the skin with a nerve bundle running underneath (Figure 2). Within the nerve bundle is a single nerve fibre (axon) upon which we will focus.
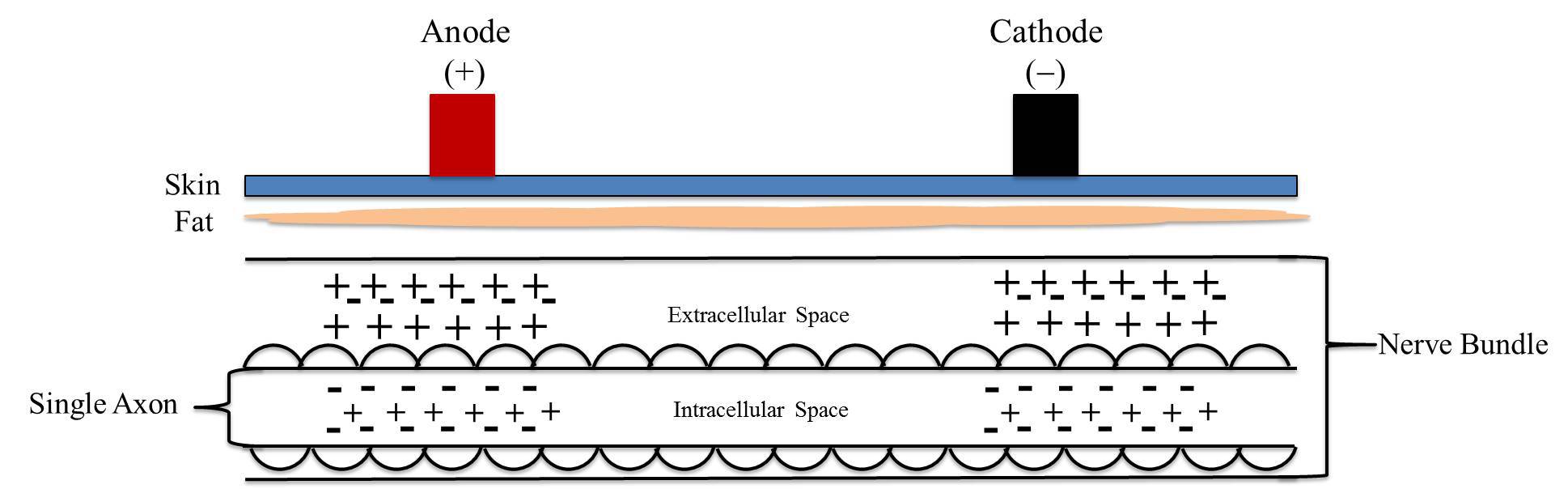
At rest, the inside of a cell is more negative than the outside of a cell.
This occurs because there is a slightly greater number of negative charges than positive charges inside of the cell (intracellular space), and a slightly greater number of positive charges than negative charge outside of the cell (extracellular space). Because of the electrical difference, the cell is said to be polarized- just like a magnet, one side is more positive and the other side is more negative. If the electrical gradient were suddenly reversed, the cell would be depolarized, and we might see an action potential."
(Reference: Vogel, R. W. (2017, December). Understanding Anodal and Cathodal Stimulation [Blog post]. American Society of Neurophysiological Monitoring. Retrieved from
https://www.asnm.org/blogpost/1635804/290597/Understanding-Anodal-and-Cathodal-Stimulation
Below is a table view of the difference between a contraction elicited through normal central nervous system function as compared to that via electrical stimulation.
|
Motor Unit Recruitment - Central Nervous System |
Motor Unit Recruitment and Contraction - Electrical Stimulation |
|
Active |
Passive |
|
Small type I motor units are recruited first then larger type II motor units for smooth and gradual tension |
Large superficial fatigable type II motor units are recruited first, then smaller motor units |
|
Asynchronous firing in off and on pattern - energy efficient and slower onset of fatigue |
Synchronous firing - motor units stimulated continue to fire until stimulus removed, causing quick onset of fatigue |
|
Action potential moved away from the nerve cell body |
Action potential generated in two directions, away from the cell body and back toward the cell body |
Approximately 6 minutes
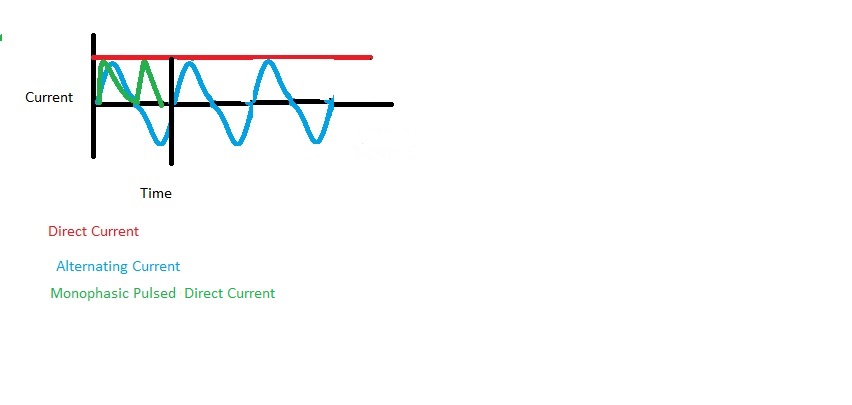
There are three basic waveforms used in commercial therapeutic electrical stimulation units: direct current, alternating current, and pulsed current.
Direct Current (DC) - Galvanic
Alternating Current (AC) - Biphasic
Pulsed Current (pulsed - AC and DC)
Approximately 9 minutes
There are four common clinical names that describe electrical stimulation devices:
|
Electrical Stimulation Device |
Type of Current |
Summary of Action |
|
Russian |
AC - Burst modulation |
uses current to depolarize muscle and stimulate a muscle contraction |
|
High Volt Pulsed Current (HVPC) |
monophasic, pulsed |
uses high intensity, short duration, pulsed current to promote charge accumulation in the tissue |
|
Interferential Current (IFC) |
amplitude- modulated AC |
asynchronous waves interfere and produce a pain modulating effect; uses four electrodes |
|
Low intensity direct current (LIDC; Microcurrent) |
DC or monophasic pulsed |
uses unidirectional flow of current to accumulate a charge in tissue |
In addition to the common practice of referring to electrical devices when talking about electrical stimulation (ES or "estim), there are three common acronyms that describe types of electrical stimulation:
|
Acronym |
Description |
Effect |
Sample conditions |
|
NMES (motor effect) |
neuromuscular electrical stimulation
|
activation of skeletal muscle for strengthening Measure: manual muscle test or dynamometry |
Post-operative joint repair or replacement Muscle is innervated |
|
FES (motor effect) |
Functional electrical stimulation |
activation of skeletal muscle for reactivation or movement training and recovery of purposeful movement Test or measure: functional task performance |
Post-stroke, spinal cord injury or other paralytic conditions Peripheral nerve innervation is intact |
|
TENS (sensory and circulation effect) |
Transcutaneous nerve stimulation |
applied over skin for pain modulation referred to as "conventional", "sensory" or "high frequency" |
Low back pain; neck pain |
|
TENS (motor and circulation effect) |
Transcutaneous nerve stimulation
|
Twitch motor response applied to affected areas related to the pain referred to as "acupuncture" or "low frequency" |
Generalized pain |
|
HVPC (edema reduction effect) |
High Volt Pulsed Current |
Applied to joints and limbs to reduce acute swelling. The active electrode is the cathode (-) in acute stages |
Acute ligament sprain |
|
HVPC (tissue repair) |
High Volt Pulsed Current |
Applied to wound in the inflammation and proliferation stages; changes in cell membrane and influx of calcium ions promotes tissue healing early stages of healing: cathode (-) is treatment electrode debridement stages (e.g. remodeling): anode (+) is the treatment electrode |
Decubitus ulcers; pressure injury |
Naming can be confusing! To recap, you may hear or read any of the following terms about electrical stimulation applications:
Russian, HVPC, IFC, Microcurrent, NMES, FES, or TENS
In order for therapists to reproduce the effect of electrical stimulation, best practice is to make decisions based on the waveform (e.g., DC, AC, burst or modulated AC, low intensity direct current), pulse frequency, and pulse duration
Approximately 6 minutes
When selecting electrical stimulation, a therapist must select a device and an application that will support achieving the desired effect. Common goals that may be achieved with including electrical stimulation into the treatment include:
The physical therapist will screen each patient for contraindications. Precautions are conditions to consider when selecting and applying electrical stimulation
There are times when a Physical Therapist may decide to use a modality that is normally contraindicated after discussion with the patient's physician. For example, a patient with a history of cancer in the distant past or application of the modality at an extremity away from the cancer site may not pose more risk than benefit.
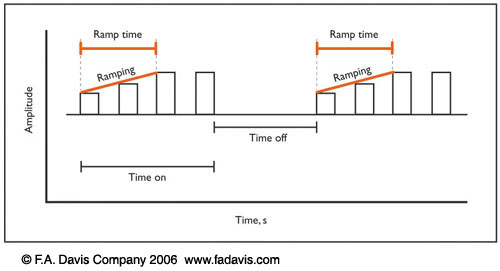
Electrical stimulation parameters are intentionally selected to produce the desired effect. Electrical stimulation parameters are frequency, duty cycle, ramp time, and duration. For direct current and monophasic pulsed current, the active electrode is set for a positive or negative tissue charge.
Frequency - number of electrical pulses delivered to the body in one second
|
low |
medium |
high |
|
<= 1 kHz "microcurrent" |
1-100kHz IFC, Russian, LIDC |
>100kHz TENS, HVPS |
Duty Cycle - percentage of on time to total time between pulses
Ramp Time - the time it takes to increase wave amplitude to its peak amplitude
Duration - the total time providing electrical stimulation. Treatment times can range from 10 to 45+ minutes
This table provides a summary of conditions that may be treated effectively with electrical stimulation.
Key point: You will find variations in the literature about parameters with respect to pulse frequency, pulse duration, and duration. For this reason, you will not be teste on pulse frequency or pulse duration or duration. In clinical practice, you will consult the literature and use observation, patient feedback, and measures to inform your effectiveness.
|
Indication |
Type |
Waveform |
Pulse Frequency (pps) |
Pulse Duration (µS) |
Intensity |
Duration |
|
Muscle strengthening |
NMES |
AC, Russian
|
50-80 |
200-800 |
to 60&-70& max voluntary contraction |
10-20 strong contractions |
|
Contraction for function |
FES |
AC, Russian |
20-60 |
200-800
|
to the desired effect |
task specific |
|
Pain Modulation |
High frequency TENS |
pulsed AC or DC |
>50; generally 80-110 |
50-100 |
to perception of stimulus; no motor response |
20-30+ minutes |
|
|
Low frequency TENS |
pulsed AC or DC |
<10 |
> 150 |
to point of visible muscle twitch |
20-45 minutes |
|
|
Hyperstimulation |
DC or pulsed DC |
(High) 100 (Low) 1-5 |
250. up to 1 second |
to highest tolerated painful stimulus |
30-60 seconds each area |
|
Edema Management (acute) |
Sensory stim |
pulsed DC |
100-125 |
2-100 |
to comfortable sensory threshold; just below motor response |
20-45+ minutes |
|
Edema Management (subacute/chronic) |
NMES |
AC, Russian |
20-80 |
100-600 |
to tetanic muscle contraction |
3 seconds on: 3 seconds off x 10-20 minutes |
There are many choices of electrode shape, size, and configuration to fit the need of the patient and therapeutic goal for electrical stimulation.
Carbon - Impregnated Rubber Electrodes - degrade over time and become non-uniform with "hot spots", many shapes and sizes, rinse and dry after each use and replaced every 12 months to ensure conductivity.
Self-Adhering or Single use Electrodes - flexible conductors, convenient application, no strapping or taping to keep in place, resealable bag for multiple uses, often high impedance, possibility of cross-contamination, used most frequently these days. Single use electrodes MAY NOT be shared between patients.
Electrode Size and Current Density
Completing the Circuit - an electrical stimulation treatment must include a full circuit. To complete the circuit, there must be:
Monopolar - always two poles: cathode (-) is active and produces cell depolarization. Produces a net charge
Bipolar - two electrodes in a single circuit; each electrode alternates between positive and negative; electrodes are of equal size; no net charge is produced
Patient will feel excitatory response under both electrodes, eliciting motor response or electrode placed over motor point, other electrode over muscle belly and may be larger
Quadripolar - four electrodes in two circuits that operate independently, yet interact
Interferential, large area, pain management, sensory stimulation of larger fiber
Note: electrical stimulation units will call the circuits "channels"
|
Treatment Goal |
# Leads and Electrodes |
Monopolar |
Bipolar |
Quadpolar |
|
Muscle (motor) Stimulation |
One channel per muscle with both electrodes on the same muscle, two leads if it Is a larger muscle or if the device has more than one head
|
|
X |
|
|
Sensory Stimulation |
One or two channels depending on the size of the area; use as many electrodes as possible to achieve the desired sensory stimulation
One channel only if two electrodes fit in the treatment area
|
|
X |
X
|
|
Tissue repair |
One channel: active electrode in the treatment area and the dispersive is placed proximally to target area >12-18" away |
X |
|
|
Evidence is emerging constantly and it is important to consider both the theoretical effects and the strength of the evidence, while keeping PICO in mind. It is a best practice to consider the patient population (P), intervention (I), comparison group (C) and outcomes (O) when making decisions about evidence-guided practice.
The PTA is given a Physical Therapy evaluation with patient medical history, diagnosis, goals, and plan of care (POC). Often, simply 'modalities' or 'electrical stimulation' is listed but no specific treatment parameters. Based on this information and subjective information gathered from the patient at the time of treatment, the PTA determines the most appropriate modality and parameters for that specific treatment as it falls within the POC. PTAs should also consider evidence and make evidence-guided decisions.
Patient response to treatment is always monitored and reported back to the PT. It is the responsibility of the PTA to make modifications within the plan of care and consult with the PT as needed. Since there is an object or substance being applied to the body, remember skin checks before and after application of any modality.
Communication with the patient is crucial, including informed consent, and checking for changes in the patient's medical history since the last visit. There may have been a medical test, appointment with a physician, or changes in physician's orders since the previous therapy appointment. The PTA must decide if and how the changes may affect the impending treatment and communicate with appropriate staff.
Refer to Table 10-8 in your Dutton text "Key Points to Remember When Using Electrotherapeutic Modalities"