Therapeutic Heat and Cold
PTA 101 Introduction to Clinical Practice
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Heat and cold are commonly used at home and in the clinic to treat symptoms of discomfort and injury. In this lesson, we will learn more about the physiological effects of heat and cold in the treatment of soft tissue injuries
A brief video message from Christina about studying effectively
Heat can produce a multifactorial effects in body tissues and systems:
|
Hemodynamic |
Increased circulation |
|
Neuromuscular |
Increased nerve conduction velocity Increased pain threshold Changes in muscle strength |
|
Metabolic |
Increased metabolic rate |
|
Elastic |
Increased collagen extensibility |
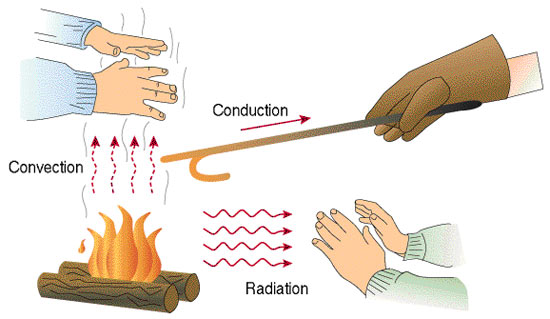
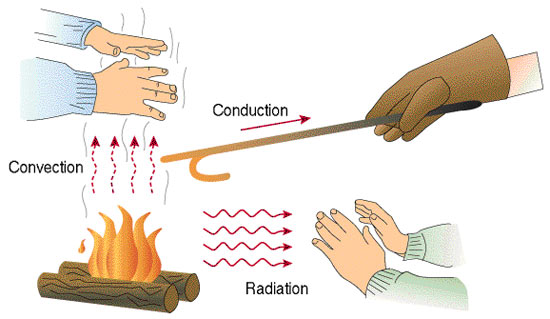
https://upload.wikimedia.org/wikipedia/commons/e/e6/Heat-transmittance-means1.jpg
Key point: superficial thermal agents (like a hot pack) do not increase temperature below a depth of 12 cm.Once the heat source is removed, temperature changes dissipate almost immediately.
The increased circulation rates to muscles results in bringing cooler blood to the treatment area, and homeostasis with muscle temperatures is maintained. Application of heat to reduce pain from a muscle strain is based on increasing the pain-inhibiting nerves and receptors found in the skin and tendons. Decreased muscle guarding decreases pain.
Exercise (isometric, or other) combined with heat produces the greatest increase to circulation and metabolic rates in body tissues
|
Impairments and Goals |
Treatment considerations |
Functional Outcome |
|
Decrease pain
|
Position patient for comfort |
Improve functional activity or improved functional ROM |
|
Decrease spasm |
Position patient so stretch to affected muscles is reduced |
Improved mobility |
|
Increase tissue extensibility |
Position patient so stretch on affected soft tissue is on slight stretch |
Improve functional ROM (e.g., reaching, bending) |
|
Increase circulation Promote tissue healing
|
Screen for benefits in facilitating inflammatory responses (histamine and prostaglandin release) |
Improve function
|
Chronic musculoskeletal conditions show ability to benefit from heat. Impairments resulting from chronic spinal pain, sprains and strains, and postural dysfunctions are examples where therapeutic heat can be an integral part of promoting functional recovery.
Conditions and impairments associated with loss of soft tissue extensibility (e.g. scar tissue, myofascial syndromes, joint disorders) can also benefit from thermal agents.
Be sure to spend time with the "application of heat" linked slide show in preparation for the unit and for lab
A brief video message from Christina on how to use tables like the one below to develop clinical decision-making skills
|
Contraindications |
WHY? Apply knowledge of physiological responses Explain why the contraindications "make sense" |
Precautions |
WHY? Apply knowledge of physiological responses Explain why the precautions "make sense"
|
|
Acute injury or inflammatory response |
|
Pregnancy |
|
|
Recent or potential hemorrhage |
|
Impaired circulation |
|
|
Thrombophlebitis |
|
Poor thermal regulation |
|
|
Impaired sensation |
|
Edema |
|
|
Altered mental status |
|
Cardiac insufficiency |
|
|
Malignancy |
|
Directly over an open wound |
|
|
Infrared irradiation of eyes |
|
Implanted metallic devices in the area |
|
|
|
|
Directly over an area where topicals have been applied |
|
|
Hot packs |
15-20 minutes; at least 2 hours wait between applications |
|
Fluidotherapy |
15-20 minutes at 100-118 degrees (pt tolerance monitoring) with simultaneous AROM |
|
Paraffin wax |
6-10 "dunks", dip-wrap method with wax paper/plastic bag and a towel for insulation at 10-15 minutes while elevated |
A brief video messages about program expectations for learning about diathermy
|
|
Continuous SWD |
Pulsed SWD |
|
Hemodynamic |
Increased circulation |
Increased circulation
|
|
Neuromuscular |
Increased nerve conduction velocity Increased pain threshold Changes in muscle strength |
|
|
Metabolic |
Increased metabolic rate Increased enzymatic activity |
Increased microvascular profusion Increased local tissue oxygenation increased cellular nutrient availability increased phagocytosis by activating macrophages Activate growth factor in fibroblasts Accelerate cell growth and division |
|
Elastic |
Increased collagen extensibility |
|
Much like superficial heat, diathermy can be used effectively in conditions resulting from chronic spinal pain, sprains and strains, and postural dysfunctions. Pulsed diathermy can be used much like our non-thermal agents to control pain and edema. Most specifically, pulsed SWD is used to facilitate wound healing (post-surgical, decubitus ulcers, burn-related injury)
|
Hemodynamic |
Decreased circulation, then increased circulation |
|
Neuromuscular |
Decreased nerve conduction velocity Increased pain threshold Decreased muscle spasticity |
|
Metabolic |
Decreased metabolic rate |
|
Impairments and Goals |
Treatment considerations |
Functional Outcome |
|
Decrease pain
|
Position patient for comfort |
Improve functional activity or improved functional ROM |
|
Control spasticity |
Close monitoring of skin and elapsed time, especially when there is associated sensory loss |
Improved mobility and functional use |
|
Decrease edema |
Position to facilitate fluid return to circulatory system (e.g. elevate affected area) |
Improve functional use |
|
Decrease circulation Promote tissue healing
|
|
Improve function |
Acute soft tissue injury and post-surgical conditions show ability to benefit from cold, primarily through pain and edema reduction. Neuromuscular conditions that include increase spasticity (e.g. neurologically-mediated resistance to stretch) can be treated with cold to decrease nerve firing and improve available ROM. Pain from chronic spine and joint conditions can also be reduced with cold.
Depth of penetration is up to 5 cm and and application effects can last 1-2 hours
Be sure to spend time with the "Cold Application" linked slide show in preparation for the unit and for lab
|
Contraindications |
WHY? Apply knowledge of physiological responses Explain why the contraindications "make sense" |
Precautions |
WHY? Apply knowledge of physiological responses Explain why the precautions "make sense"
|
|
Cold hypersensitivity |
|
Poor sensation |
|
|
Cold intolerance |
|
Over an open wound |
|
|
Cryoglobulinemia |
|
Hypertension (HTN) |
|
|
Paroxysmal cold cryoglobulinema |
|
Altered mental status |
|
|
Raynaud's disease and phenomenon |
|
Pediatric and geriatric patients |
|
|
Directly over a regenerating peripheral nerve |
|
Directly over the superficial or main branch of a nerve |
|
|
Directly over and area with circulatory compromise or peripheral vascular disease |
|
|
|
|
Cold packs |
15-20 minutes; or 15-20 on: 10 minutes off x 2 |
|
Ice massage |
5-10 minutes or until pain is reduced/region is numb "CBAN" |
|
Vapocoolant sprays |
2-5 parallel sweeps at 10cm/sec with bottle 45cm from skin and at a 30 degree angle |
In the literature, particularly in studies whose aim is to systematically review intervention effectiveness, there is weak evidence supporting the use of heat and cold as pain reducers or in impacting function. Parameters for treatments have been derived from research studies and analysis of effectiveness is ongoing. As a PTA, you are responsible for understanding and applying treatment parameters that are consistent with today's literature and in the PT plan of care. Selecting parameters will always include careful analysis of each patient's condition and interests at the time of treatment. You are also equipped, through evidence-based research skills, to engage in discussions and best practices as we work to restore function with our patients.
![]()
![]()
![]()
![]()