 http://abwwc.com/images/Cycle%20of%20Pain%20-%203.jpg
http://abwwc.com/images/Cycle%20of%20Pain%20-%203.jpgIntroduction to Tissue Injury and Physical Agents
PTA 101 Introduction to Clinical Practice
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Pain is the most common complaint for which we seek medical and physical therapy treatment. For the remainder of this class, we will focus on foundations for utilizing physical agents as interventions for tissue healing and pain management. We will apply documentation principles to case simulations and select standardized assessment tools for tracking pain and pain responses during a course of physical therapy.
Pain presentations can be complex, localized, referred, and chronic. Individuals who seek physical therapy must be assured that their complaint is heard and that treatment planning is focused on minimizing the impairments, functional limitations, and disabilities associated with painful symptoms.
Pain is a protective sensory experience that alerts the mind-body of a trauma, injury, or illness. The body's response to injury and subsequent pain is swift and complex.
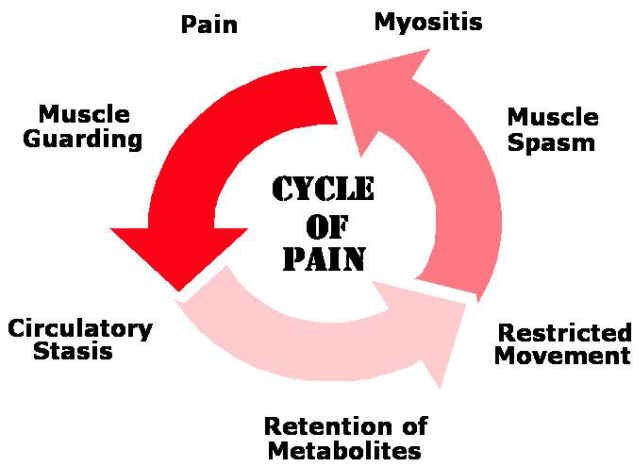
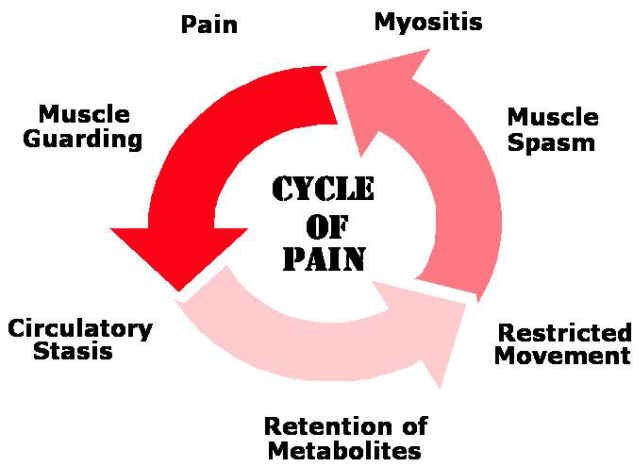
The primary pain cycle illustrates physiologic tissue responses during acute tissue injury and inflammation. Following a tissue injury, muscles maintain high levels of resting tension to protect healing tissue and prevent motion. Because muscles are continuously in order to guard the region, circulation to the affected muscle tissue decreases. This triggers a cycle of swelling, impaired circulation, inflammation, fatigue, and soreness.
Watch and listen to a description of this process:
 http://abwwc.com/images/Cycle%20of%20Pain%20-%203.jpg
http://abwwc.com/images/Cycle%20of%20Pain%20-%203.jpg
The "cardinal signs of inflammation" indicating tissue injury are often included in the patient subjective complaints following trauma.
The ascending and descending pathways for sensory and motor pathways are described in your text. The level of detail concerning lamina within the spinal cord and the subdivisions of the ascending and descending tracts are beyond the scope of this lecture.
Sensory pain stimulus from the external or internal environments travel up the nerve and cross over to the contralateral side at the level of the spinal cord/brainstem
Ascending sensory tracts synapse in endocrine, motor, sensory, and limbic (emotional) and memory cortical areas, resulting in a complex response we call PAIN.
Inflammation is an essential component for tissue healing. Without inflammation, there would be no tissue repair.
Inflammation and its effects need to be addressed to optimize tissue healing and interrupt the pain cycle
Acute pain is the symptom associated with how the brain interprets direct tissue trauma and the subsequent inflammatory response which initiates the tissue healing processes. Over time, as endogenous opiates have an effect and as tissue sensitivity decreases, injured tissue heals within 2 weeks to 3 months and function is restored. Acute pain is usually easily to localize (e.g, the patient can point to it or name a specific body part/structure/area).
Persistent pain is defined as:
Common causes of recurrent or persistent pain:
Psychosocial impact of persistent pain are significant and can lead to disability. Unrelenting pain sensations can result in chemical changes which impact appetite, mood, mobility, body system function, sleep, libido, and participation in work/social life. Patients who are unable to adequately manage persistently painful conditions may lose employment and strain family relationships. Individuals with persistent pain are at higher risk for depression and addiction disorders.
The role of the PT and the PTA in the treatment of persistent pain is to be an active participant in a multidisciplinary team that guides pain management. Cardiovascular endurance, pacing and prioritizing, body mechanics and posture, counseling and imagery/cognitive behavioral therapy (CBT), nutrition, stress management, and medication management comprise best practices for persistent pain management.
Subjective reports of pain include a description of the pain quality. Pain descriptions may provide some insight into level of acuity and the involved structures. It is important to know that people who persons persistent pain may report a multiple and fluctuating descriptions of somatic (felt in the body) pain, without any evidence of recent tissue trauma.
A PTA must be able to make comparisons in subjective reports of pain quality and decide if interventions should be modified or discontinued based on the patient response. Marked changes in pain presentation and quality may require consult with the supervising physical therapist.
Watch and listen to "Christina describes pain qualities"
|
Pain Quality |
Associated Involved Structure* |
|
cramping, dull, aching |
muscle |
|
sharp, shooting |
nerve root |
|
sharp, burning, lightning-like |
nerve |
|
burning, pressure-like, stinging, aching |
sympathetic nerve |
|
deep, nagging, dull |
bone |
|
sharp, severe, intolerable |
fracture |
|
throbbing, diffuse |
vasculature |
pain can also perceived in one area while being generated from a distant structure
|
Plexus |
Spinal Levels |
Example Signs and Symptoms |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
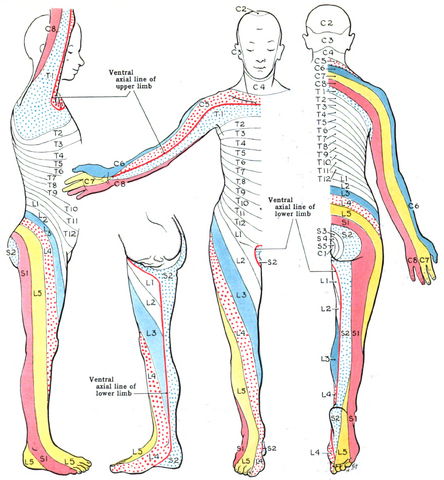
"Grant 1962 663" by Grant, John Charles Boileau - An atlas of anatomy, / by regions 1962. Licensed under Public domain via Wikimedia Commons - http://commons.wikimedia.org/wiki/File:Grant_1962_663.png#mediaviewer/File:Grant_1962_663.png
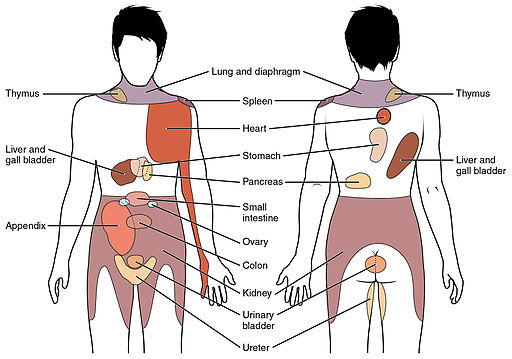
By OpenStax College [CC-BY-3.0 (http://creativecommons.org/licenses/by/3.0)], via Wikimedia Commons
Again, pain is complex, and many patients want an explanation and relief. There are several theories around pain and pain suppression that have served as a foundation for the use of some physical agents (e.g., electrical stimulation) and others that are developing with ongoing study and research.
Nociception is the ability to detect and perceive pain from an external stimulus. Persistent pain is increasingly considered a pain experience - one that can present without a preceding external stimulus.
Caution: Pain is a perception. Pain has shifted toward a biopsycholsocial (body, behavior, and environment) model for the pain experience, and involves cognitive and physiological processes. Be very careful when trying to explain or account for pain using theories as a basis for your explanation. Speak to what you can support with resources and evidence, and simply be aware that theories around pain and pain modulation continue to be studied and evolve.
Endogenous opiates are neurotransmitters released in the body which provide analgesic effects (block effects of pain signals). Some are short-acting (enkephalins) and others are longer acting (endorphins). Endorphins concentrations in the tissues have been shown to increase with:
Persistent pain management includes patient education in building confidence in movement, developing skills in pacing and prioritizing, using self-care tools for modulating autonomic nervous system (ANS) arousal (the "fight or flight" response). Tools for ANS regulation include topicals, aromatherapy, journaling, breathing and imagery. Fear avoidance behaviors around movement and activity can increase nervous system irritability and trigger the primary pain cycle from prolonged tension or holding patterns.
As discussed in the "Explain Pain" video from Unit 1, patients who experience persistent pain should coached in methods to distinguish "hurt from harm" and to "go to the pain, not through the pain". For some, pain is constant. Pain management are skills a patient learns to maximally function while applying techniques that use the brain to change pain.
A PTA must have a solid understanding of tissue healing stages in order to select the most appropriate intervention from the plan of care. Although pain is the main reason people seek physical therapy, the underlying cause of pain is an injury or repetitive strain which results in inflammation and tissue strain.
Your text summarizes common musculoskeletal conditions (see Dutton, Table 4-1). In addition to those listed in Table 4-1, study tendinopathy, tendinosis, and, tenosynovitis, Take some time to make it relevant to your understanding of the WHO-ICF and future clinical practice (and support your learning) by developing hypothetical examples of a patient's "history" and "subjective complaint" that fits with the type of injury. Note: you may need to refresh your prior knowledge of musculoskeletal anatomy to come up with credible examples, or simply use the example you generated for the PTA 101 Week 2 Discussion.
For example, this could be an example of knee synovitis:
S: "patient reports swelling, stiffness and difficulty bending and straightening the right knee after prolonged kneeling while repairing her hardwood floors"
What is the health condition?
What is the subjective complaint? How does this inform understanding of involved body function and structures?
What is the history that informs understanding of health condition?
All of the examples in the text describe tissue injury due to mechanical or chemical stress. Biopsychosocial factors will influence the patient's pain response and pain behaviors, including prior medical and related history. Therefore, interventions available in the physical therapy plan of care shall consider the context of the individual situation and reflect realistic patient goals.
Link to podcast

Following examination and evaluation, the physical therapist develops a plan of care which may include goals to minimize the impairments, functional limitations, and disabilities associated with tissue injury. Physical agents use heat/cold, light, water, vibration, current, compression, and stretching stimuli to facilitate functional recovery. Physical agents may also be referred to as "modalities" in the physical therapy plan of care.
Maturity of scar tissue must be taken into consideration when choosing a modality.
The following impairments may be justifications for selecting a biophysical agent to promote tissue healing and recovery.
A PTA must complete a review of the physical therapy evaluation and related information in the medical record, gather subjective information, and make observations and comparisons in order to select a modality which will optimize recovery. A PTA must be able to distinguish between typical and atypical presentations across a number of systems observations, tests and measures:
![]()