Ultrasound
PTA 101 Intro to Clinical Practice
Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Lesson Objectives
- Describe how sound energy is transmitted through the body
- Define treatment parameters and units of measure used in ultrasound: (frequency, duty cycle, intensity).
- Describe the non-thermal effects of therapeutic ultrasound.
- Select continuous vs. pulsed ultrasound based on the intended tissue effect in a patient case scenario.
- Differentiate between absorption and penetration effects of ultrasound in soft tissue.
- Differentiate between reflection and refraction effects of ultrasound in soft tissue.
- Describe how the anatomy underlying tissues effects impedance and absorption of ultrasound.
- Define "unstable cavitation" and what a PTA can do to prevent it.
- Explain why understanding cardinal signs of inflammation is important in selecting and applying ultrasound.
- Explain why a coupling agent is recommended when administering ultrasound.
- Select an appropriate response if a patient reports pain during ultrasound application.
- Identify the role of the PTA during application of physical therapy interventions covered in this course.
- Discuss how the patient's age and medical status may influence selection and outcome of treatments with physical agents.
Overview of Ultrasound: The Physiological Effects of Sound
I've also created some videos for you here to help illustrate how ultrasound is converted within biological tissue
Now, these videos pull it all together in an example of treating a soft tissue injury with continuous ultrasound and pulsed ultrasound
Review of Non-Thermal Effects
Non-thermal effects are produced when the duty cycle is 20% (1:5) and may be included in the plan of care to support tissue repair. Some thermal effects are produced while ultrasound is pulsed (e.g., 50%), however, these effects result in minimal tissue heating.
- enhanced inflammatory response - plasma and cells which promote tissue regeneration may increase the efficiency and effectiveness of the inflammatory response
- enhanced elimination of debris and bacteria - the rate with which cells (macrophages - "giant eaters") break down exogenous (foreign) substances is increased, thus increasing the rate of tissue healing.
- enhanced formation and propagation (growth) of cells (fibroblasts and collagen) which repair and reconnect previously damaged tissue
- increased rate of capillary growth and regrowth - increased and improved circulation (blood flow) to the healing area
Safety Considerations
Contraindications
Therapeutic (not diagnostic) ultrasound may not be applied in the following situations:
- over a uterus during pregnancy
- over the gonads or eyes
- on malignant or precancerous lesions
- on irradiated skin
- in areas with vascular abnormalities (deep vein thrombosis (DVT), arteriosclerosis)
- ove an acute infection
- in the cardiac area when there is advanced heart disease.
Remember, ultrasound promotes tissue proliferation, collagen formation, and circulation. Therefore in conditions where there is circulatory or vascular disease, or when tissue growth could increase the spread of disease or result in burns, do not apply ultrasound.
Precautions
Ultrasound is a physical agent that may effect tissue properties. Precautions when preparing to apply ultrasound include
- impaired cognition - impact reliability in ability to accurately report sensory experiences
- peripheral vascular disease - systemic circulation disease may adversely effect tissue healing; may have intermittent sensory loss
- advanced age - tissue components are more fibroid, less hydrated, susceptible to heating quickly
- previous experience with ultrasound - some patients have had negative effects (e.g., hot spots) and will decline further ultrasound
- pain with pressure - patients with hypersensitivities may not be able to tolerate the pressure and weight from the transducer
Ultrasound Procedures
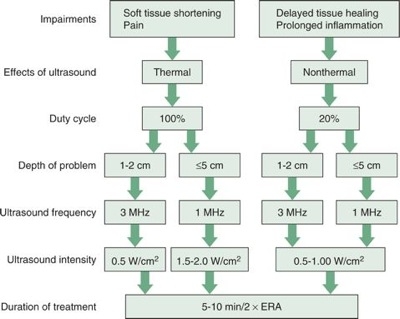
Clinical Decision Making
Before selecting ultrasound, a PTA must confirm that modalities are listed in the physical therapy plan of care (POC). It is common to simply see "modalities" checked in the plan of care without any stipulated treatment parameters.
A PTA must, therefore, be able to review the plan of care, identify an impairment (e.g., pain, soft tissue restriction, ROM restriction, edema, skin integrity) and select the most appropriate treatment parameters based on the patient case.
Patient communication is an essential component of effective ultrasound treatment. A PTA should ask the patient about any previous experience with ultrasound and confirm informed consent to the proposed treatment prior to applying ultrasound. A screen of precautions and contraindications may be indicated depending on the information a PTA can derive from the PT's initial evaluation. A patient may disclose a medical condition (e.g., cancer) to the PTA which was previously unknown to the PTA.
Any patient disclosure of a precaution or contraindication to ultrasound which is not reflected in the medical record shall result in immediate communication to the supervising PT before initiating treatment. If a PTA has questions about the safety and effectiveness of a prescribed modality in a POC, the PTA shall seek clarification from the supervising PT prior to administering the modality
A PTA must also be continuously monitoring the tissue and the patient in order to make timely treatment modifications as needed.
A PTA must also recognize signs of equipment malfunction. PTAs monitor clinical ultrasound equipment for signs of wear and tear, including integrity of electrical cords and the transducer . A PTA can place the sound head underwater at an angle to the surface and increase intensity to 1.0 W/cm2. Water should lightly ripple/displace, indicating an active sound head. A biomedical inspection should occur at least annually.
Dosages
- Mode (continuous or pulsed). The intended thermal or non-thermal (acoustic streaming and stable cavitation) effects determines the mode
- Continuous (100% duty cycle) - sound energy is constant during treatment
- Pulsed (10%, 20%, or 50% duty cycle) - sound energy has quiet periods where no energy is transmitted. For example at 50%, the ratio of on time to off time is 1:1.
- Frequency (MHz). This is typically 1 MHz or 3 to 3.3MHz depending on the manufacturer. The depth of target tissue determines the frequency
- The higher the frequency, the less the sound wave will spread out in the tissues.
- The higher the frequency, the more the quickly the tissue absorb the acoustic energy.
- Therefore, ultrasound delivered at the lower frequencies (e.g., 1 MHz) allow the acoustic energy to reach the deeper tissue
- Intensity (W/cm2). This is the power of the sound energy and drives temperature effects. The higher the power and intensity, the shorter the treatment time to produce a thermal effect. Understanding of the mix of tissues within the treatment area (e.g., fat, muscle, bone, edema) guides power and intensity decision-making.
- Time (min). This is determined by patient comfort and the tissue effect you are trying to achieve. Higher frequencies need less treatment time to achieve target tissue effect. Lower intensity needs a longer treatment time to achieve the desired effect.
|
Temp Increase
|
Tissue Effect
|
|
1°C
|
Increases metabolism, reduces mild inflammation
|
|
3.6-5.4°C
|
Reduces pain and muscle spasm; increases blood flow
|
|
7.2°C
|
Increases ROM and tissue extensibility (in combination with stretching and exercise)
|
Redrawn from Cameron MH: Physical Agents in Rehabilitation: From Research to Practice, ed 2, St. Louis, 2002, WB Saunders.
Keep in mind that the effective radiating area (ERA) is determined by the manufacturer of the clinical unit. The ERA is determined by the type and integrity of the crystal in the transducer (sound head). In general, the treatment area is generally about twice the size of the transducer in order to produce thermal and non-thermal effects.
Tissue Properties
- Each soft tissue has its own acoustical properties, effecting how much ultrasound energy it will absorb
- The denser the tissue, the more resistance there will be to acoustical energy - dense molecules and not be "moved" by sound waves
- The lowest resistance to acoustic waves is found in blood and water - ultrasound energy travels freely through without losing its strength
- scar tissue, tendon, and ligaments easily absorb sonic energy
- Bone is very dense - it will create a barrier preventing additional flow of ultrasound from the sound head into surrounding tissue
- Bone can also reflect and refract sonic energy (think of an "echo" effect), resulting in a "standing wave" (wave flowing toward bone crashes into wave reflecting from bone) and increase risk to surrounding tissue from a sudden additive effect of combining waves (unstable cavitation)
Documentation
Essential elements of documentation include:
- Subjective: Specifically, some statement from the patient which includes their opinion on their pain, function, swelling, motion restriction, skin condition and/or response to previous treatment.
- Objective: Patient consent, position, treatment area, frequency, intensity, duration, time. Tests and measures related to selection of ultrasound (pain levels, girth measurements, observations (redness),etc.)
- Assessment: clinical opinion of therapeutic effects (reduced pain, swelling, etc.) as it relates to the POC and pt goals.
- Plan: any follow up for next visit regarding application of modality.
Sample note - 10/19/18 11:00-11:35
S: Patient reports modest changes in R hip pain from in her bursitis area. Pain is 6/10 with activity, like walking. Unable to walk > 2 blocks due to hip pain.
O: Pt consent to US: Pain to palpation R trochanter bursa 6+/10. Applied US 0.6 W/cm2 @ 1 MHz, 50% x 6 min to bursa, followed by gentle soft tissue mobilization abductor strengthening activities in partial WB. Instructed in HEP for PWB functional abductor strengthening exercises (see handout). Pain with palpation decreased to 4/10 after US application
A: US appears beneficial in reducing pain, allowing for manual stretching and progressing HEP with stable pain levels.
P: Continue with POC, assess pain response and functional changes next visit
Layne Coledge, SPTA
Self Assessments
End of Lesson
Consider testing your knowledge of therapeutic ultrasound application using the case study at the end of your text. Use the CAN YOU HELP ME? forum to share your thoughts and present alternative cases which would change your clinical decision.
References: Knight, K.L. & Draper, D.O. (2008). Therapeutic modalities: the art and the science. Lippincott Williams & Wilking: Baltimore, MD.
![]()
![]()
![]()
![]()
![]()
![]()
![]()