Applications of Ultraviolet Light
PTA 101 Introduction to Clinical Practice
PHYSICAL PROPERTIES OF ULTRAVIOLET RADIATION
Reference: Cameron: Physical Agents from Theory to Practice
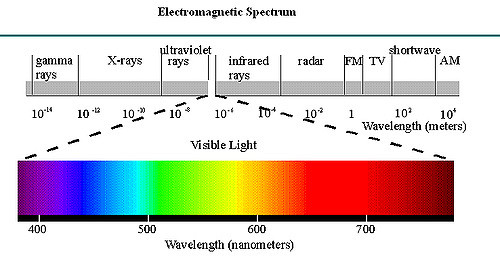
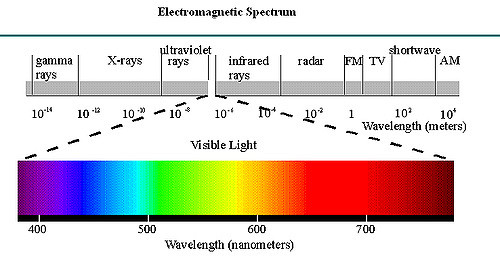
Ultraviolet (UV) radiation is electromagnetic radiation.
The frequency of UV radiation lies between that of x-rays and visible light.
(image: https://www.flickr.com/photos/scfiasco/110098808)
UV radiation is divided into three bands—UVA, UVB, and UVC—with wavelengths of 320 to 400, 290 to 320, and less than 290 nm, respectively
UVA, also known as long-wave UV, produces fluorescence in many substances, whereas UVB, or middle-wave UV, produces the most skin erythema. UVC, or short-wave UV, is germicidal.
Because UV does not produce heat, it is thought to produce physiological effects by nonthermal mechanisms. The most significant source of UV radiation is the sun, which emits a broad spectrum of UV, including UVA, UVB, and UVC. Both UVA and the UVB reach the earth from the sun; however, UVC is filtered out by the ozone layer. Patients can be treated with UV of specific wavelength ranges using a UV lamp.

Image https://uvb-lamps.com/product/uvb-lamp-psoriasis/?roistat_referrer=&roistat_pos=1o1&roistat=google2_s_21485685181_85909918621_&gclid=EAIaIQobChMI4PXpyca91wIV3LjACh13zwwREAQYASABEgJylPD_BwE
The physiological effects of UV radiation are influenced not only by the wavelength of the radiation but also by the intensity of radiation reaching the skin and its depth of penetration. The depth of UV penetration is affected by the:
When treating a patient with a UV lamp, the intensity of UV radiation reaching the patient's skin is proportional to the power output of the lamp, the inverse square of the distance of the lamp from the patient, and the cosine of the angle of incidence of the radiation beam with the tissue. Thus the intensity reaching the skin is greatest when a high-power lamp is used, when the lamp is close to the patient, and when the radiation beam is perpendicular to the surface of the skin.
The intensity of UV radiation reaching the skin is highest with a high-power lamp positioned close to the patient with the radiation beam perpendicular to the skin's surface. Penetration is deepest for UV radiation with the highest intensity, longest wavelength, and lowest frequency.
UVA penetrates farthest and reaches through several millimeters of skin, whereas UVB and UVC penetrate less deeply and are almost entirely absorbed in the superficial epidermal layers. The penetration of UV radiation is also less deep if the skin is thicker or darker.
Erythema, or redness of the skin as a result of dilation of the superficial blood vessels caused by the release of histamines, is one of the most common and obvious effects of exposure to UV radiation.
Erythema is produced primarily in response to UVB exposure, or in response to UVA exposure after drug sensitization. Without drug sensitization, UVA is 100 to 1000 times less potent in inducing erythema than UVB. With sensitization, the erythemal efficacy of UVA is similar to that of UVB alone, with less risk of overexposure or burning.
The precise mechanism of UV-induced erythema is unknown; however, it is known that this effect is mediated by prostaglandin release from the epidermis and that it may be related to the DNA-damaging effects of UV radiation. The severity of erythema, which can produce blistering, tissue burning, and pain, and the risk of cell damage are the primary factors limiting the intensity and duration of UV exposure that can be used clinically.
Because patients vary in their degree of erythemal response to UV, a minimal erythemal dose (MED) is determined for each patient before initiating treatment with UV radiation. Progressively higher doses of UV radiation are generally needed during a course of UV treatment due to skin changes from tanning and hyperplasia. In the laboratory setting UVC in adequate doses can be bactericidal. UVC radiation is used to kill bacteria in food and, in one small study, UVC was found to be as effective as standard hospital cleaners in removing pathogens from hospital surfaces. One clinical study also found that UVC radiation may help reduce bacterial load in open wounds and improve wound healing.
When applying UV radiation for therapeutic purposes, one must first determine the individual patient's sensitivity to UV radiation. This varies widely among individuals and can be affected by skin pigmentation, age, prior exposure to UV radiation, and use of sensitizing medications. For example, even for Caucasians, there can be a fourfold to sixfold variation in minimal erythemal dose. Sensitivity to UV radiation is assessed using dosimetry procedures described in the next section. Because the response to UV radiation can vary significantly with even slightly different frequencies of radiation, the same lamp must be used for assessing an individual's sensitivity and for all subsequent treatments. For example, the skin is 100 times more sensitive to UV with a wavelength of 300 nm than to UV with a wavelength of 320 nm. If the lamp must be changed, the individual's response to the new lamp must be assessed before it is used for treatment. Reassessment is also necessary if there is a long gap between treatments because lamp output intensity decreases with prolonged use and skin tanning and hyperplasia decreases over prolonged periods. Once the individual's responsiveness to a particular UV lamp has been determined, the treatment dose can be selected to produce the desired erythemal response.
At this time, UV radiation is used primarily in the treatment of psoriasis, and there are also recent reports of UV therapy being used for the treatment of other dermatological conditions, including:
These treatments may be applied in conjunction with the use of photosensitizing drugs. UV is also used occasionally as a component of the treatment of chronic open wounds. Although the clinical application of UV radiation for the treatment of skin disorders is within the scope of physical therapy, such treatments are generally provided by dermatologists or their assistants. Physical therapy providers may be promoting wound healing in a plan of care, which may include UV radiation for chronic wounds.
Video (approximately 5 minutes) about Vitiligo
Care should be taken when applying UV radiation to patients who are taking photosensitizing medications or supplements. Photosensitizing medications include sulfonamide, tetracycline, and quinolone antibiotics; gold-based medications used for the treatment of rheumatoid arthritis; amiodarone hydrochloride and quinidines used for the treatment of cardiac arrhythmias; phenothiazines used for the treatment of anxiety and psychosis; and psoralens used for the treatment of psoriasis. Certain dietary supplements, including St John's wort, are also known to be photosensitizing. While patients are taking these medications or supplements, they have increased sensitivity to UV radiation, resulting in a decrease in the minimal erythemal dose and an increased risk of burning if too high a dose is used. A patient's minimal erythemal dose must be remeasured if the patient starts to take a photosensitizing medication or supplement during a course of UV treatment.
No dose of UV radiation should be repeated until the effects of the previous dose have disappeared. Because of the potential cumulative adverse effects of repeated low-level exposure to UV radiation, it is recommended that clinicians avoid frequent or excessive exposure during patient treatment. This can be achieved by wearing UV-opaque goggles and UV-opaque clothing.
Burning by UV radiation will occur if too high a dose is used. Burning can usually be avoided by careful assessment of the minimal erythemal dose before initiating treatment and by avoiding further exposure when signs of erythema from a prior dose are still present.
Chronic exposure to UV radiation, including sunlight, is associated with premature aging of the skin. This effect, known as actinic damage, causes the skin to have a dry, coarse, leathery appearance with wrinkling and pigment abnormalities. It is thought that these changes are primarily the result of the collagen degeneration that accompanies long-term exposure to UV radiation.
Most of the information regarding the carcinogenic effect of UV radiation concerns the effect of prolonged or intense sunlight exposure. Prolonged exposure to UV radiation, as occurs with excessive exposure to sunlight, is considered to be a major risk factor for the development of basal cell and squamous cell carcinoma and malignant melanoma. A review of the literature on the carcinogenicity of UV phototherapy, with and without psoralens, concluded that the therapeutic use of UVB has a low risk of producing cutaneous cancers, except possibly on the skin of the male genitals; however, there is a definite cutaneous carcinogenic risk from PUVA treatment when oral systemic psoralens medications are used. The increased cancer risk with PUVA may be a result of the carcinogenicity of the psoralens or may be a response specific to the wavelength of UV radiation used for this treatment application. PUVA treatments may also exacerbate the effects of previous exposure to carcinogens.