Vital Sign Assessment
PTA 101 Intro to Clinical Practice 1
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Click here to test your understanding of blood pressure measurement rationale and procedures
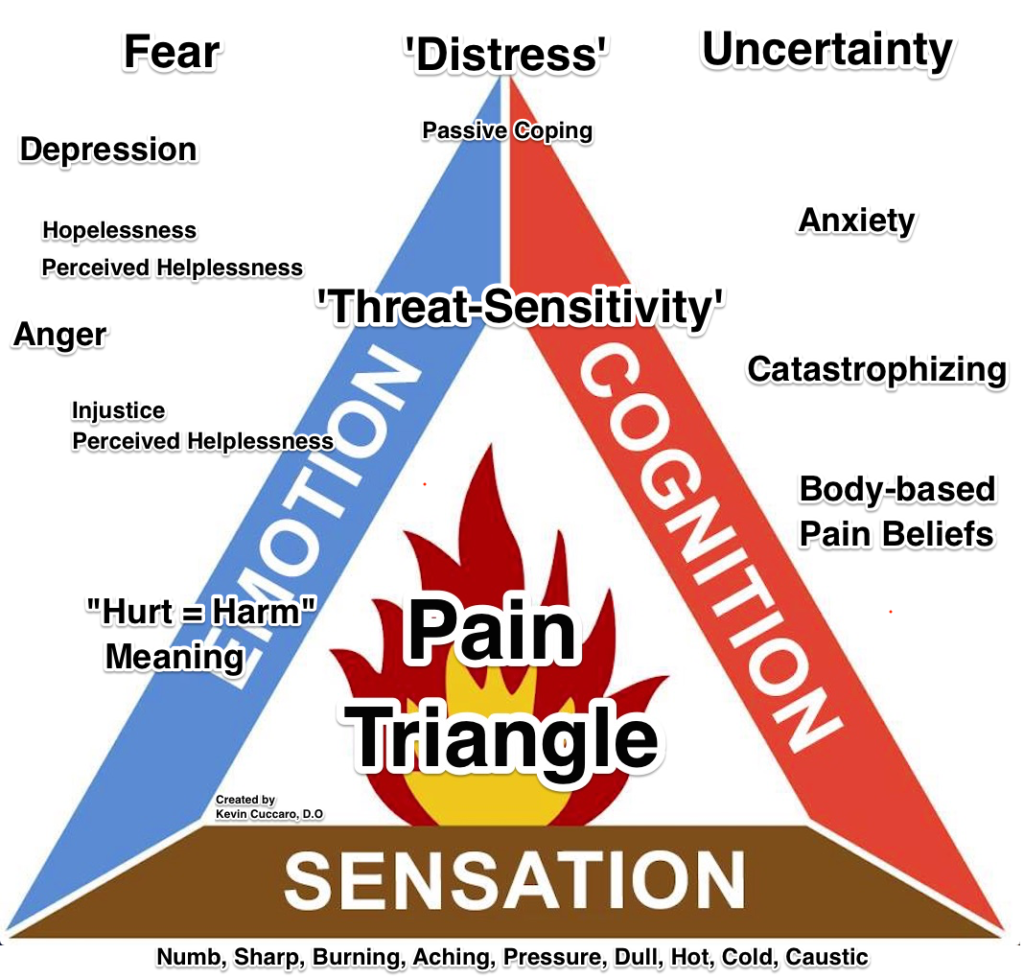
How we think about pain is changing. In the recent past, pain was referred to as the "fifth vital sign". With the development of pain science knowledge, more providers are considering pain as an experience that can be complex, measured and treated in multiple ways. This diagram from Dr. Cuccaro represents cognition, sensation, and emotions as the fuel for the "pain experience".
This video provides a five-minute summary of explaining pain as an experience and may expand your understanding of how physical therapy providers and others are talking about pain:
There is a variety of general-to-specific methods of measuring and documenting pain. Next week, you have an essay on the clinical application of pain scales. A few are included in your text, and I have linked some additional, standardized assessment tools for pain in the table below. Standardized measures can be very powerful tools to document changes in quality of life and in functional activities as a result of physical therapy. Progress and declines (regressions) are easily supported by changes in pain measures.
You can prepare for your essay assignment and for the exam/lab by completing the following table
|
Assessment Tool |
Advantages |
Disadvantages |
|---|---|---|
|
Visual Analog Scale (VAS) |
|
|
|
Faces Pain Rating Scale |
|
|
|
Mc Gill Pain Questionnaire |
|
|
|
Oswestry Disability Questionnaire |
|
|
When you were observing therapists at the clinic, how did therapists gather information about pain? Think about age, culture, cognition (thinking), time, relevance, and function. (links to podcast) All of the assessment tools listed above are used to collect data about pain. Could you explain to your supervising PT why you selected a particular tool? Critical thinking wtih decision-making is demonstrated by your ability to provide a rationale for your choice that is patient-specific and evidence-based.
Podcast on documenting vital signs
Vital signs are objective data that provide information about physiological status and responses to stress. Ideally, vital signs are collected before engaging in physical activity, particularly in the deconditioned population. When vital signs are abnormal, the PTA may need to modify treatment approaches or consult with their supervising PT or nursing staff. Documenting vital signs taken throughout the physical therapy session provide evidence of ongoing patient assessment and monitoring.
PTAs make informed decisions when selecting exercises and other interventions by interpreting vital sign measures prior and during treatment. Document findings using consistent terminology and include patient position/situation (lying, sitting, standing) so that the data is transferable and can be interpreted by a multidisciplinary team. Pain documentation may include a rating, location, and other information about its quality and should include its impact on activity and participation. Events or other contextual factors that may contribute to the pain experience are also considered.
:
|
Vital Sign |
Documentation |
|
Heart Rate (HR) |
# bpm |
|
Respiratory Rate (RR) |
# / min |
|
Blood Pressure (BP) |
systolic (mm Hg)/ diastolic (mm Hg) |
|
Temperature (temp)
|
°C or °F
|
|
Oxygen Saturation (O2 sat)
|
# %
|
S: Pt lying with HOB elevated. Eager to work on getting OOB. Slept better last NOC. Agreeable to in bed exs.
O: Pain 2/10 ache R hip, VS â Rx: BP 146/82, HR 74bpm, RR 14/min, O2 sats 95%
{additional treatment information would follow here, including any additional VS measures collected during the session}
![]()
Show/hide comprehension question...
Show/hide comprehension question...
Show/hide comprehension question...
Show/hide comprehension question...
Show/hide comprehension question...
Did you take advantage of the self-checks?
Have you tried the Can You Help Me? forum
Did you check for related assignment due dates and TIMES?
Do you have any other questions? Let me know!