
Endocrine and Metabolic Disorders
PTA 103 Introduction to Clinical Practice 2
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment. Contact howardc@lanecc.edu for permissions.
This resource is required reading and provides an excellent framework for the different types of diabetes and provides a strong example of effective patient education in heath promotion through effective disease management and lifestyle modification. Link to Content

• Improved medical management of DM results in long term survival (American Diabetes Association, 2016)
• Chronic pathological changes and conditions evolve over time
– Neuropathy: progressive increases in pain and sensation changes/sensory loss
• Neuropathy in autonomic nervous system can lead to impaired regulation of heart, lung function, and/or other function = high risk for silent MI (heart attack without angina)
– Cardiovascular disease leads to increased risk for MI
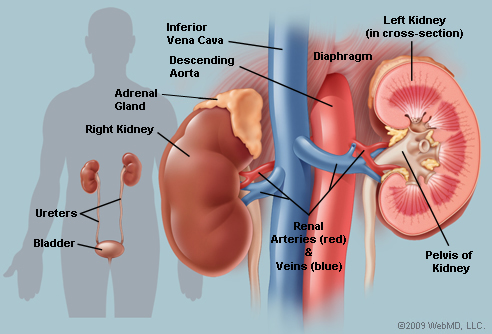
– Nephropathy leads to kidney failure
– Retinopathy leads to visual changes/loss of vision
– Impaired wound healing can lead to amputation
– Higher infection risk associated with hyperglycemia

Patient education in health promotion and self-management
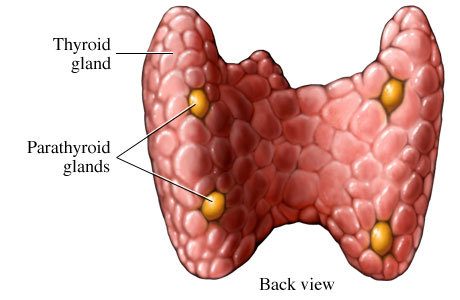
http://www.pauerhome.com/ryan/endocrine_system/pictures/parathyroid_gland_diagram_1.jpg
Primary cause are parathyroid tumors (adenoma) and can lead to hypercalcemia (calcium in blood stream)

Insufficient calcium effects multiple cellular functions: muscle contraction, bone growth, and blood coagulation. Symptoms include bony deformity in digits, cardiac dysrhythmia, infertility. In severe cases it can lead to seizures, tetany (maximal contraction without relaxation), and death
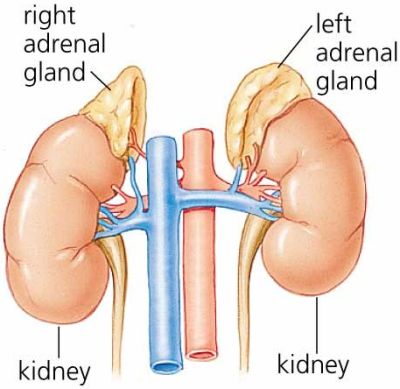
http://www.pyroenergen.com/articles10/images/adrenal-gland.jpg
Primary adrenal gland dysfunction, resulting in decreased cortisol production It may also result in decreased aldosterone.
Hydrocortisone is the principal glucocorticoid produced by the adrenal and is essential in times of stress. Reduced cortisol hormone levels results in decreased cardiac output and decreased vascular tone (difficult for blood vessels to constrict).
Weight loss, hypotension, weakness, fatigue, skin changes

Adrenal gland dysfunction, resulting in increased cortisol production.Some common observational and clinical findings include:
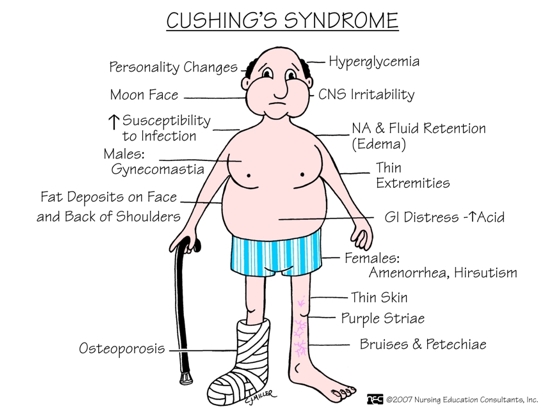
Excessive cortisol can affect body structures and functions at rest and during exertion. Examples include:

https://upload.wikimedia.org/wikipedia/commons/e/ed/ThyroidImage.jpg
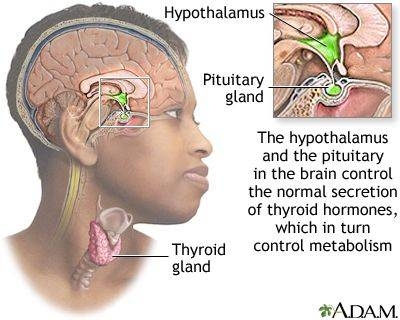
The thyroid gland synthesizes and releases thyroid hormones which have diverse physiologic effects including cardiac, pulmonary, hematopoietic, gastrointestinal, skeletal, neuromuscular and endocrine effects (growth, reproduction, energy metabolism). T4, and to a much lesser extent T3, is released from the thyroid. Thyroid hormone synthesis is mediated by an enzyme called thyroperoxidase (TPO) and this enzyme is the target in Hashimoto's (autoimmune thyroiditis).
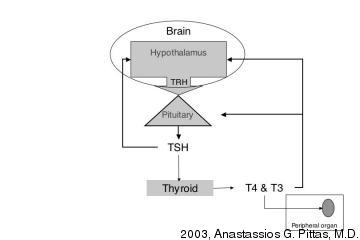
T3 is considered the active form of thyroid hormone. Thyroid function is regulated by the hypothalamic-pituitary-thyroid axis, shown in Figure 1. Synthesis and release of T4 and T3 are positively regulated by Thyroid Stimulating Hormone which, in turn, is positively regulated by TRH. Note the negative feedback by thyroid hormone on TSH secretion by the pituitary (as well as on TRH secretion by the hypothalamus).
| Figure 1. Hypothalamic-pituitary-thyroid feedback system for control of thyroid hormone secretion |
 |
Thyroid hormones are transported in serum bound to carrier proteins. The 0.04% of T4 and 0.4% of T3 that is free is the biologically active form.
Thyroid Binding Globulin (TBG) is the major thyroid hormone binding proteins. Alterations in thyroid binding proteins (especially TBG) will markedly change the total T4 and total T3 levels. Factors that influence thyroid hormone binding and therefore will alter total thyroid hormone levels include:
TSH positively regulates thyroid hormone synthesis and release while a a negative feedback exists by thyroid hormone on TSH secretion by the pituitary.
Serum TSH is the best SCREENING test for the diagnosis of hypothyroidism or hyperthyroidism in healthy ambulatory individuals. It is the initial test done to assess thyroid function and the only test needed if it is normal.
Serum TSH in patients with primary hyperthyroidism (which accounts for 99.9% of the cases of hyperthyroidism) is low. A very low value (<0.01) is diagnostic of hyperthyroidism while a low value (0.01-0.1) suggests hyperthyroidism. Exceptions include conditions that primarily affect the hypothalamus/pituitary.
Serum TSH is invariably increased in patients with primary hypothyroidism (which accounts for 99% of cases of hypothyroidism) and is one of the most specific tests in medicine; virtually nothing else raises the serum TSH.
The incidence of hypothyroidism varies based on sex, age and geographic/environmental factors (most important being dietary iodide), but over 5-10% of individuals over 65 may have hypothyroidism. Hypothyroidism can occur as a result of a defect within the thyroid gland itself (primary hypothyroidism) or from a deficiency of TSH secretion (secondary hypothyroidism) or TRH secretion (tertiary or hypothalamic hypothyroidism). Thyroid insufficiency can also arise from peripheral tissue resistance to thyroid hormone. The treatment of hypothyroidism is oral thyroxine (T4). Secondary hypothyroidism may be treated with additional medication
Primary hypothyroidism is due to defect within the thyroid gland. This is by far the most common cause accounting for 98% of cases of hypothyroidism.
Chronic thyroiditisis almost always due to Hashimoto's thyroiditis which is the most common cause of hypothyroidism. The etiology of Hashimoto's thyroiditis is autoimmune destruction of the thyroid gland. Similar to other autoimmune conditions, Hashimoto's is more common in women with age. There is a strong familial component. Thyroid destruction is irreversible and slowly progressive. Thyroid antibodies (anti-thyroglobulin and/or anti-TPO antibodies) are present in the majority of patients. Autoimmune thyroiditis may coexist with other autoimmune disease such as pernicious anemia, rheumatoid arthritis, and diabetes mellitus. "Burnt out" Graves' disease also belongs in this category.
In adults, it is almost always due to pituitary disease. These patients often have other associated pituitary dysfunction. Selective TSH deficiency is a very rare genetic cause of newborn hypothyroidism and may also be seen in adults.
Hypothyroidism may be suspected by symptoms and signs, but the diagnosis needs to be confirmed biochemically (laboratory testing).
The most common features of hypothyroidism include fatigue, dry skin, cold intolerance, constipation, menstrual irregularities and possibly weight gain.
The skin appears pale and waxy due to vasoconstriction, increase in carotene concentration and anemia. Coarse dry hair and hair loss especially from the temporal aspect of the eyebrows. Decreased activity of sebaceous glands contributes to the dry skin
Bradycardia, impaired muscular contraction and decreased cardiac output are seen. Cardiomegaly and pericardial effusion may be present. Pleural and peritoneal effusions also may be encountered. Angina may occur due to coronary artery disease upon initiation of thyroid replacement. There is evidence to suggest that incidence of coronary atherosclerosis is elevated in hypothyroidis. Dyspnea and anemia is common. Appetite is reduced. Modest weight gain may be seen due to water retention.
Thyroid hormone is essential in nervous tissue development. Children born hypothyroid suffer from severe brain damage (cretinism). The earlier the initiation of treatment, the better the results for normal intellectual development. Decreased concentration, lethargy and coma may be seen in adults. Sedatives (morphine, barbiturates, etc.) may precipitate C02 narcosis and coma. Carpal tunnel syndrome may be seen. Reflexes are characteristically slow (relaxation phase) due to decreased muscle function. Muscle stiffness, aching, cramps very common. Lack of thyroid hormone during development can result in skeletal deformity and can have similar effects of degenerative arthritis in adults.

Hyperthyroidism refers to excess thyroid hormone from hyperactivity of the thyroid gland (excess production or release). This is called thyrotoxicosis.
Graves' disease is the most common form of hyperthyroidism accounting for 60-70% of all cases. It occurs in up to 3% of the population. There is a strong familial component and the disease is more common in women (F:M ratio 5:1) in the third and fourth decade. It is an autoimmune disorder.
The symptoms and signs of hyperthyroidism, shown in Table 1, and their severity correlates with the level of circulating thyroid hormone.
| Table 1. Symptoms and Physical Signs of Thyrotoxicosis | |
| General | Weight loss, heat intolerance, insomnia |
| Skin | Sweating, palmar erythema, onycholysis (nail separation from nail bed) |
| Nervous System | Tremor, Nervousness, anxiety, hyperkinesis |
| Cardiovascular | Dyspnea on exertion Palpitations, arrhythmia (atrial fibrillation) Increased systolic BP, decreased diastolic BP, Increased cardiac output |
| Reproductive | Irregular menses, amenorrhea, infertility |
| Gastrointestinal | Increased frequency of bowel movements |
| Musculoskeletal | Myalgia, proximal muscle weakness Osteopathy (subperiosteal bone formation and swelling) |
| Head and Neck | Lid lag, stare, lid retraction Goiter |
Understand how the reason for the PT referral medical history and contributing factors influence the focus of the PT intervention plan and goals. Specific elements in these conditions include
• Review of clinical and lab tests and medications
• Review of body systems
Assess prior use of assistive devices, such as adaptive footwear, braces, device for gait
Selected tests and measures will be driven by clinical need and are based on the goals and plan of care. Due to the intricate involvement of the endocrine system on blood glucose and homeostatic regulation, care must be taken to
Cardiac, pulmonary, neuromuscular and integument conditions are systems that may influence optimal movement. Considerations for test include

• Exercise produces an insulin-like effect in that blood sugars are mobilized and utilized quickly in response to an increased demand for energy/ fuel
• Persons with DM are more at risk for hypoglycemia with exercise
• Persons with DM may choose to temporarily stop insulin infusion prior to exercise or may be encouraged to eat a small snack before exercise

Simple messages for type 2 diabetes control: advise consulting with attending physician and or nutritionist
Content adapted under Creative Commons 3.0 from