Cardiac Conditions and Hypertension
PTA 103 Introduction to Clinical Practice 2
Cardiac conditions can follow a progressive continuum from single body system to multiple body system impairments and dysfunction. In this lesson, we will start understanding some of the cardiac conditions and cardiac procedures you will frequently encounter in all settings involving adults. There is a significant risk for true life and death situations when working with this population. While exploring this information keep in mind that the most common physical therapy intervention is exercise, and the heart is the literal primary driving force for exercise. Factors that affect exercise tolerance will be dealt with nearly daily in your career as a PTA. Furthermore, these conditions all exist on a continuum where hypertension (HTN) often contributes to common cardiac diseases and disorders, such as myocardial infarction (MI) and congestive heart failure (CHF). Your role in rehabilitation and patient education for health and wellness promotion could literally save a life.
During a written case simulation, you may be asked to demonstrate your ability to:

![]()
Symptoms for women experiencing a MI can be different. In addition to the above, symptoms may include
![]()
References
Mayo Clinic, 2019. Heart Attack. Know the Signs and Symptoms. Available at.
http://www.mayoclinic.org/diseases-conditions/heart-attack/in-depth/heart- attack-symptoms/art-20047744
![]()
The overwhelming evidence since the 1950's, 60+ years ago is the relationship between smoking and pre-mature death. This most recent article adds even more health problems to smoking: an addiction that destroys the cardio-pulmonary system and an addiction that kills over 400,000 Americans pre-maturely every year.
As prescribed by the PTA Standards of Ethical Conduct (Standard 8) PTA's are obliged to educate members of the community about the inherent risks of smoking, direct patients and others to smoking cessation resources in an effort to improve public health
Standard #8: Physical therapist assistants shall participate in efforts to meet the health needs of people locally, nationally, or globally (APTA, 2019)
![]()
Reference
Standards of Ethical Conduct for the PTA, 2019. American Physical Therapy Association.
Back in PTA 100....
In Unit 3 of PTA 100, we covered the role of physical therapy with patients with cardiovascular conditions. We encourage you to go back to your notes from Unit 3. Specific examples of stress testing is included in this section. You should start to recognize that the interventions for conditioning and cardiac conditions are similar in that the primary impairment is typically impaired aerobic capacity and endurance.
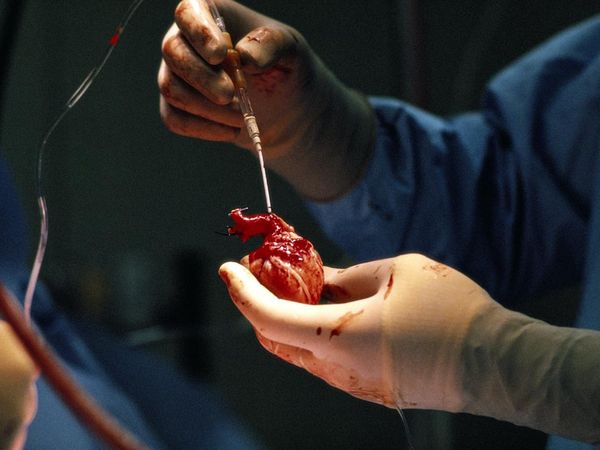
Donor Heart
The following information is all review from anatomy. Utilize it as personally needed.
Review anatomy of heart chambers, coronary arteries and heart conduction system in anatomy text. Tutorials to refresh your memory are included below:
Capillary Exchange
You are not expected to memorize the values contained in the above link
Specific anatomical references in the heart are below. You are not expected to recall anatomy at this level. These resources are included for your reference only if you would like more specific landmarks for cardiac anatomical terms
External Anatomy of the Heart (ASPSU, 2019)
apex - The tip or pointed end of the heart; in the anatomical position, the confluence of the inferior and left borders; it is a projection inferiorly, anteriorly and to the left of the left ventricle.
base - The broad superior surface of the heart, from which the great vessels emerge.
auricle - (1) The free portion of the myocardial wall of each atrium which has a superficial similarity in shape to an ear, it contracts along with the rest of the atrial wall to move blood from the atria to the ventricles; it is regulated by the Autonomic Nervous System; (2) The outer projecting portion of the ear, also called the pinna.
coronary sulcus - The slight groove seen on the external surface of the heart which indicates the borders between the atria and the ventricles; coronary vessels follow portions of the groove.
interventricular sulcus - The slight groove seen on the external surface of the heart which indicates the borders between the right and the left ventricles; coronary vessels follow portions of the groove.

Chapter 25 in Cameron and Monroe, pages 348-352 on BP.
This section is a review of BP content from PTA 101. Basic vital sign information can be cross referenced in Week 1. Be sure you make special note of Table 22-3. Focus your studying on recognizing risk factors and BP values which may result in cessation of activity.
![]()
![]()
Go back through your notes from Cameron and Monroe, pages 359-360, 361-362, and 363-366 (stopping at case study) 23-1. Again, the emphasis will be on reinforcing strategies for assessing exercise tolerance and safe exercise progressions. The Borg RPE scale is a reliable measurement for patients with cardiac conditions (Box 23-1).
![]()
![]()
This is one option for patients to monitor energy expenditure and conservation.
to watch and for a brief explanation on video
Here is the You Tube address if you are having trouble opening the video
http://www.youtube.com/watch?v=487nEIm2UCs&feature=player_embedded
Below are the primary cardiac conditions that you may encounter. Realize that all the safety considerations for applying exercise are aimed at avoiding causing another MI or sudden cardiac arrest. The role of the PTA is to recognize the signs and symptoms that may indicate excessive stress and possible and/or immediate danger to the cardiovascular system. PTAs should also be able to appropriately monitor and modify exercises consistent with with safe activity guidelines.
Pathology of conduction in the heart. Can occur at the SA node, AV node, Purkinje fibers, and bundle branch blocks
Can you think of how the use of beta blockers may affect a patient during exercise?
![]()
Angina Pectoris:stable angina - chest pain with exertion
Acute coronary syndrome:unstable angina - chest pain at rest
Read the linked web resources and be able to distinguish between the tow and discriminate the appropriate response if these symptoms present in a clinical situation.They can be frequently encountered when working with any population aged 40+.
![]()
![]()
Web exploration: Myocardial Infarction:
Web exploration: Hypertension Tutorial:
Note that hypertension definitions fluctuate. For the purposes of this course, we will use current guidelines by the American Heart Association: 130/80.
Scope of practice alert: 130/80 is a blood pressure measure. Hypertension is a diagnosis. PTAs report outcomes of tests and measures, but DO NOT classify readings in diagnostic terms. In short, do not report to a patient that they have "hypertension" if you get a high blood pressure measure.
PTAs are work with patients with recent or prior history of one or more invasive cardiac procedures. A PTA is an educator, so must have a basic understanding of procedures and their resultant influence on activity and exercise:
In your note taking, be sure you can identify the procedure's purpose for improving cardiovascular function
![]()
Careful, systematic, and continuous data collection is essential when you are engaging in activities to restore function. With movement comes increase demand on the body systems and structures, and PTAs are using clinical reasoning from the data collected to make decisions that are safe and provide the appropriate workload to the system so that it can improve.
A PTA may observe one or more of the following indicators to guide exercise effort and modify interventions:
Depending on the severity and associated signs and symptoms, this may indicate a need to stop the intervention.
This may be collected at baseline, during activity, following activity, or referenced from prior sessions to guide treatment planning. Examples include:

Answer the following questions:
Reference:
American Physical Therapy Association. 2019. Standards of Ethical Conduct for the PTA. Available at: http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/Ethics/StandardsEthicalConductPTA.pdf?navID=10737423626
Austin Pea State University. 2019. Anatomy of the Heart. Available at: http://www.apsu.edu/
Cleveland Clinic. 2019. Rate of Perceived Exertion. Available At: https://my.clevelandclinic.org/health/articles/17450-rated-perceived-exertion-rpe-scale
Mayo Clini 2019. Sign and Symptoms of a Heart Attack: Available at: https://www.mayoclinic.org/diseases-conditions/heart-attack/symptoms-causes/syc-20373106