Lower Extremity Orthotics
PTA 103L Instruction and Activities
Objectives
- Understand medical terminologies and abbreviations used to describe lower extremity (LE) orthotics and orthotic fabrication
- Describe the objectives of orthotics as it relates to the physical therapy plan of care
- Relate the major parts of a shoe to the requirements of an individuals fitted with lower limb orthoses.
- Describe the main components of LE orthoses
- Compare the characteristics of plastics, metals, and other materials used in the construction of LE orthoses
- Explain the orthotic options available for patients with paraplegia
- Describe the role of physical therapy management of LE orthotics
- Recognize the role of the PTA in orthotics management
Tips for Success
Complete your assigned reading prior to completing this lesson
Definitions
- Orthotic
- "an orthopedic applicance used to support, align, prevent, or correct deformities of a body part or improve the function of moveable parts of the body" (Cameron, p. 897)
- Objectives of an orthotic
- restricts motion
- assist motion/function (e.g., standing, walking, etc.)
- transfer load from one area to another
- reduce joint and/or muscle strain
- prevent and/ or corrects deformities
- inhibit tone
- decrease/relieve pain
- Brace = Orthotic
- Splint = temporary orthotic
- CPO = Certified Prosthetist and Orthotist; one who constructs and fits prosthetic and orthotic device.
- FO = foot orthosis
- internal modication = insert attached or glued inside of the shoe
- external modification = device secured to shoe sole or heel
- AFO = ankle foot orthosis
- KO = knee orthosis
- KAFO = knee ankle foot orthosis
- HKAFO = hip knee ankle foot orthosis
- THKAFO = lumbosacral orthosis attached to KAFO
- RGO = reciprocating gait orthosis
Physical Therapy Management of Orthotics
Physical Therapy Examination
Pre-orthotic assessment includes an examination and evaluation of the following:
- Past medical history
- History of current condition
- Social history (caregiver support)
- Medications
- Living environment
- Systems review (C/P, Integument, M/S, Neuromusc.)
- Skin assessment
- Edema/girth measurements
- Postural tone assessment
- Pathological reflex assessment
- Sensation, proprioception, and kinesthesia
- Range of motion
- Motor assessment/strength
- Mobility skills
Physical Therapy Management
- Perform pre-orthotic assessment (Exam/Eval)
- Contribute to orthotic prescription
Physical Therapy Intervention
- Instruct in donn and doff
- Patient/caregiver teaching
- care of orthosis
- skin inspection
- wearing schedule
- facilitate orthotic acceptance
- Mobility training with orthosis
- Assess and ensure proper alignment and fit
- Assess and document prescribed orthosis for:
- improved function movement while patient wears orthosis
- practicality and ease of use
- safety
Physical Therapy Goals
- Maximize functional mobility skills with use of orthosis
- Maximize independence with donning and doffing
- Maximize independence with wearing schedule
- Maximize independence with skin inspection
- Maximize competence with care of orthosis
Role of the PTA
- Perform relevant interventions (see above)
- Suggest an orthotic or an alternative if prescribed orthotic plan of care is ineffective
- Suggest referral back to the PT, MD or CPO if there are s/sxs of ineffective or unsafe orthotic use and application
- Share fucntional information with the PT and CPO to assist in prescription and fabrication of orthosis
- Fabricate orthosis (within comfort level/ with adequate training)
Self-Test Knowledge of Scope of Practice
Materials
- Plastic
- lightweight
- strong
- easily cleaned
- corrosion resistant
- Thermoplastic
- heat molded; adaptable
- inherently weaker
- Metals
- strong
- stiff
- fatigue resistance
- alters shape somewhat under tension
- resistant to heat
- weight is dependent on components/alloy
- Silicone
- strong
- poor heat conductor
- effective in reducing friction between skin and orthotic
- Leather
- strong
- porous
- indicated for patients with metal allergies or other contact dermatitis
- can be molded to fit body part/angle
- Cork
- lightweight
- flexible
- absorbs shock
- can be molded
- Cotton/wool
- absorbs moisture/protects skin
- high durability
Consequences of Poor Fit
- Uncomfortable = decreased use by patient/client
- Too tight
- excessive pressure from contact areas/straps can result in pain and potential skin breakdown
- Too loose
- excessive friction can result in skin irritation and breakdown
Shoes
- Transfer body weight to the ground
- Protect from terrain/weather
- orthopedic shoes
- reduces pressure on sensitive and deformed area by force distribution
- provides a suitable foundation for LE orthotic application
Selection of Appropriate Footwear
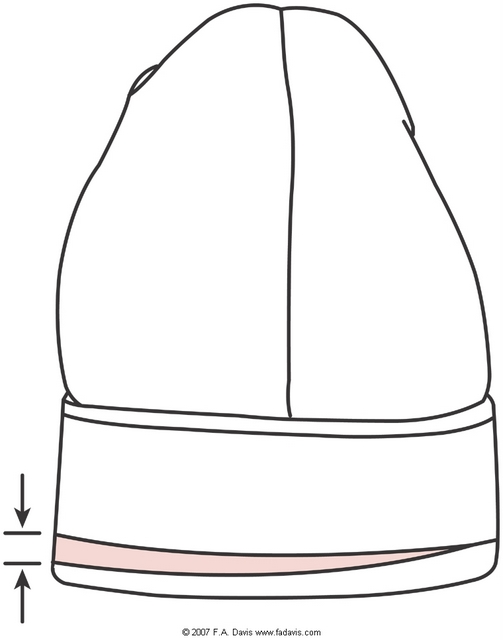
Image A represents the 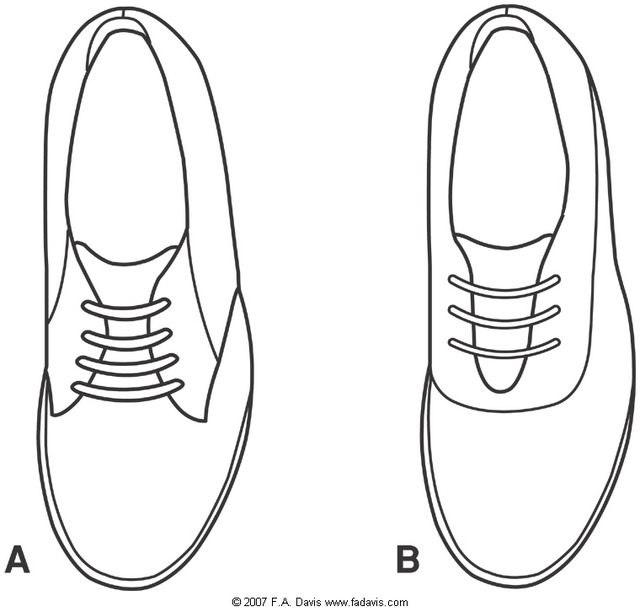 Blucher upper pattern which is most recommended for patients with foot edema, internal shoe modifications and LE orthoses
Blucher upper pattern which is most recommended for patients with foot edema, internal shoe modifications and LE orthoses
Foot Orthoses
Inserts
placed inside a shoe, can be transferred from one shoe to another
up to 3/8" inch can be added inside a lower quarter shoe without negatively impacting fit
Internal modification
glued inside a shoe, for exclusive use with a single shoe
Heel cup or lift - 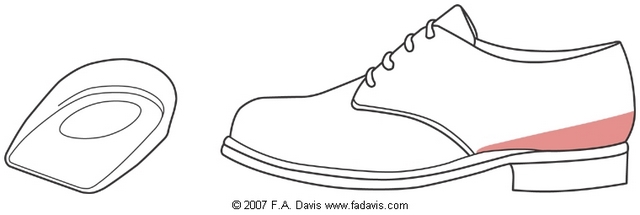 slightly increases plantar flexion and distributes force off of heel
slightly increases plantar flexion and distributes force off of heel
Scaphoid paid - medial support 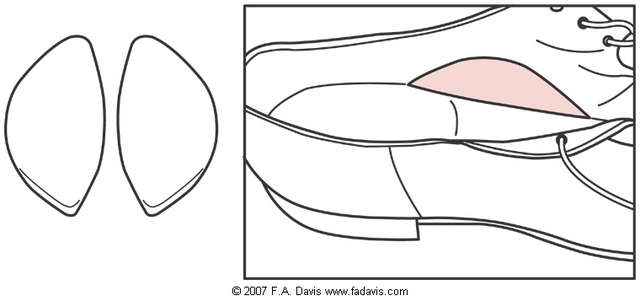 to decrease or control pronation in mid-stance
to decrease or control pronation in mid-stance
Metatarsal pad - placed posterior to MT heads 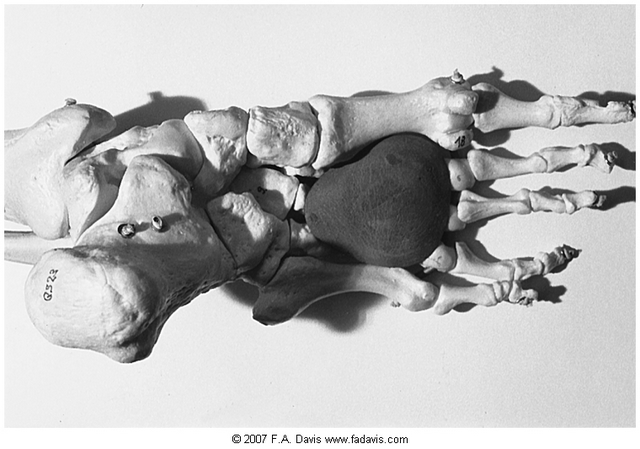 to relieve pressure off MT heads during late stance
to relieve pressure off MT heads during late stance
External Modifications
Does not reduce internal shoe volume (does not take up space in shoe), subject to wear and changes look of shoe
Medial heel wedge - can aid in reducing or controlling pes valgus (pronation)
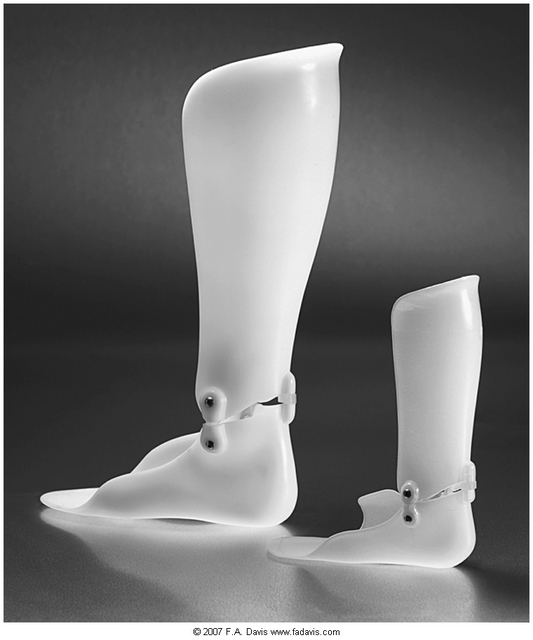
Ankle Foot Orthosis
Function - limits plantar flexion and/or dorsiflexion, or assists ankle motion
Composed of foundation, ankle control, and foot control
Foundation = shoe and a plastic or metal component
steel stirrup = metal components 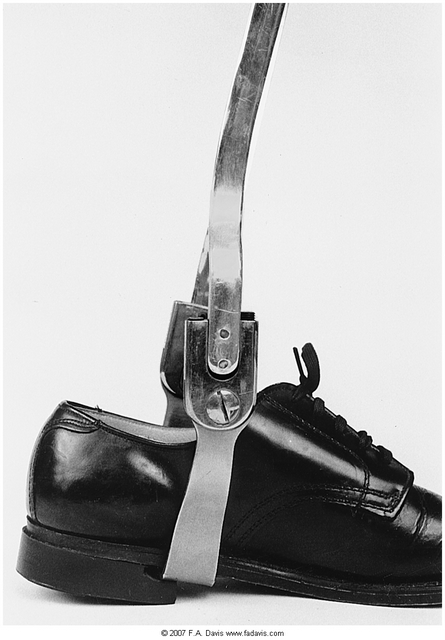 riveted to shoe
riveted to shoe
Preventing toe drag
Dorsiflexion Assist
tension coils prevent toe drag during swing phase of gait
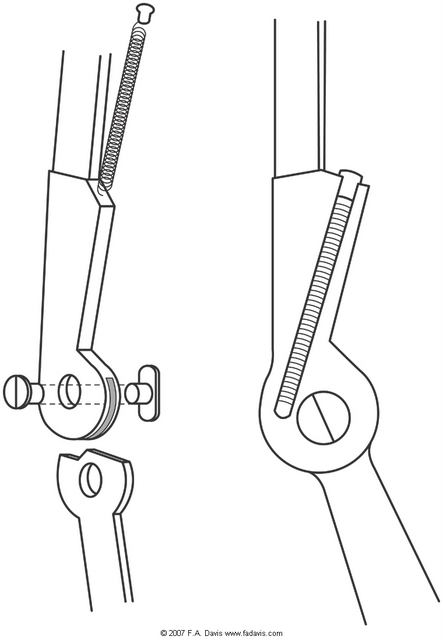
posterior leaf spring  assists dorsiflexors during pushoff
assists dorsiflexors during pushoff
Plantar flexion stop
Resists plantar flexion, and therefore toe drag, with a rigid stop
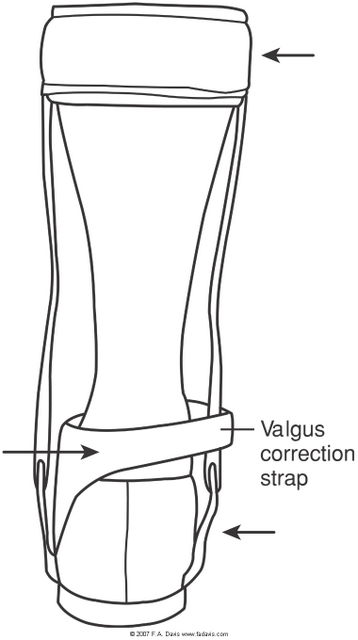
Pronation control
May be achieved through a 3-point soft strap (Valgus correction or "T" strap)
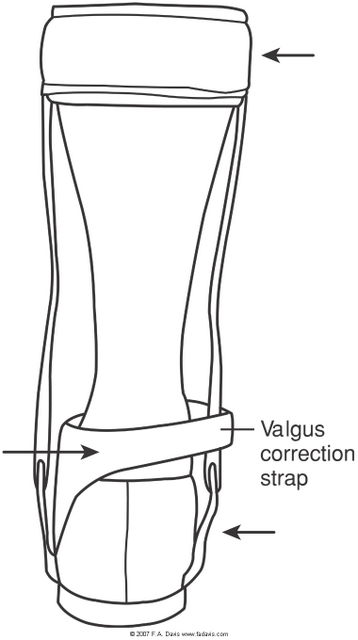
Increases complexity of donning/doffing. Requires some fine motor control to manipulate independently
Knee flexion control
Floor reaction force orthosis: Rigid posterior lower leg with strap around proximal tibia provides a posteriorly directed force which facilitates knee extension with weight acceptance.
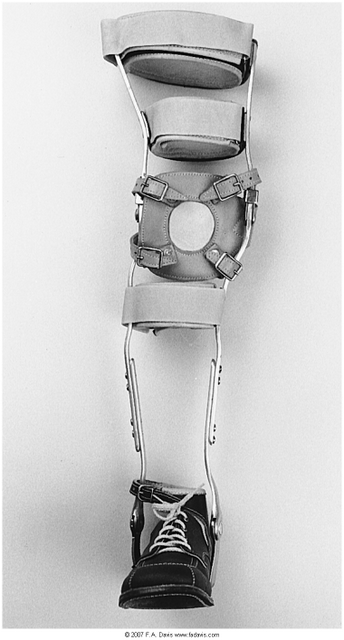
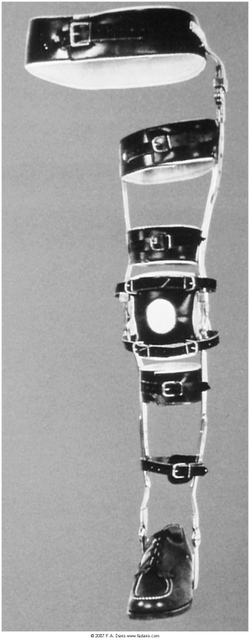
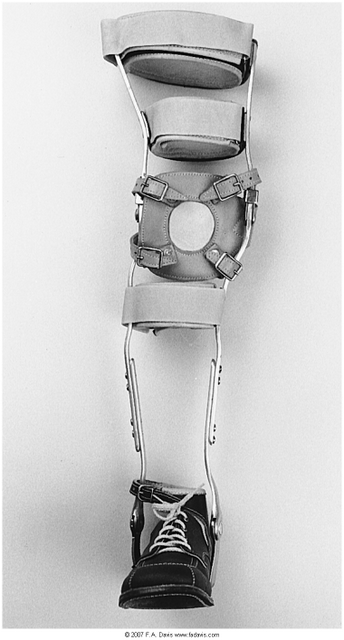
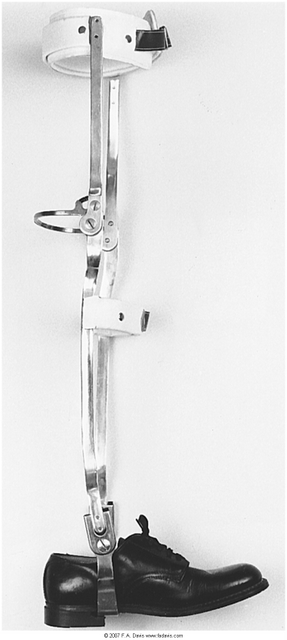
Knee Ankle Foot Orthosis
Includes all components of an AFO, with knee control and superstructure
Indicated for patients/clients with LE weakness which includes the proximal LE; increases limb stability in knee extension. Knee is locked in extension and locks are released (typically manually) to allow for knee flexion (as in return to sitting)
Superstructures: proximal aspect includes a weight bearing brim to allow for distribution of forces, proximal and distal anterior straps provide added stability and force distribution
Energy consumption with ambulation can increase to > 2x compared to normal ambulation; gait speed is significantly slower
Hinged
Restricts mediolateral, rotational and hyperextension motions
Offset hinge places the hinge posterior to midline of the knee joint, which allows for some knee flexion
Knee cap
Provides increased sagittal stability
Frontal Plane Control
Rigid plastic shell in the medial aspect of the thigh can extend more proximally to prevent genu valgum
Rigid plastic shell in the lateral aspect of the thigh can extend more proximally to prevent genu varum
Craig-Scott KAFO
Can be prescribed for adults with paraplegia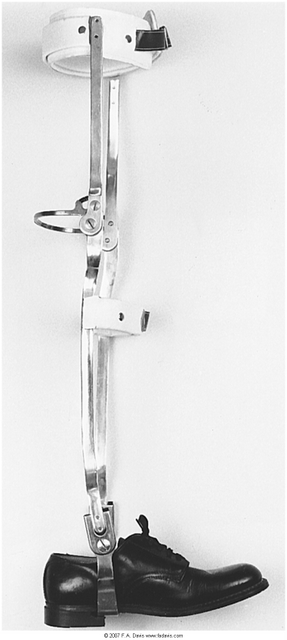
Allows patient to ambulate with crutches or a walker using swing to or swing through pattern; requires patient to lean slightly backward with trunk to prevent trunk or hip flexion (thus LOB forward)
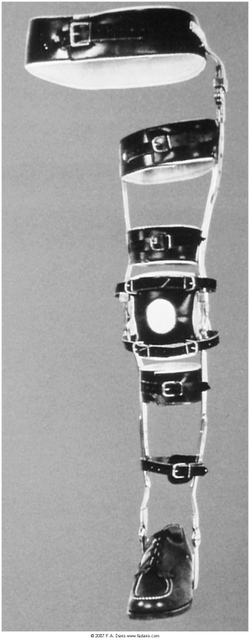
Hip Knee Ankle Foot Orthosis
Includes KAFO, pelvic band, and hip joint
Prevents hip abduction, adduction, and rotation
Can include one or both hip joints
Upholstered metal band connects HAFO to the trunk
Indicated for patient/client with significant LE paraparesis/plegia
Orthosis for Bilateral Paraplegia
Videos are hyperlinked in underlined areas
Trunk Knee Ankle Foot Orthosis
Used primarily in individuals with SCI for assisted ambulation
Requires assist for donn/doff; worn for short periods, typically under supervision during rehabilitation
Reciprocating Gait Orthosis
Allows paraplegics to ambulate with an assistive device; one limb is always in full contact with ground; when a patient shifts weight onto one limb, the cable system advances the opposite lower extremity
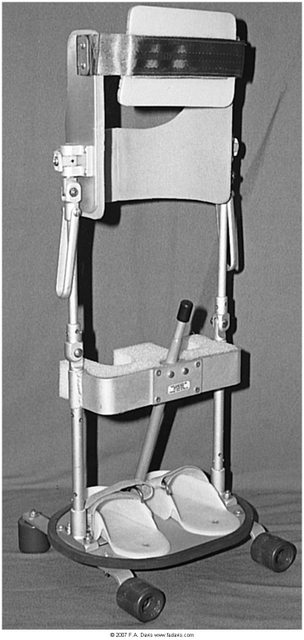
Parapodium
Standing frame that allows the user to assume a sitting position; 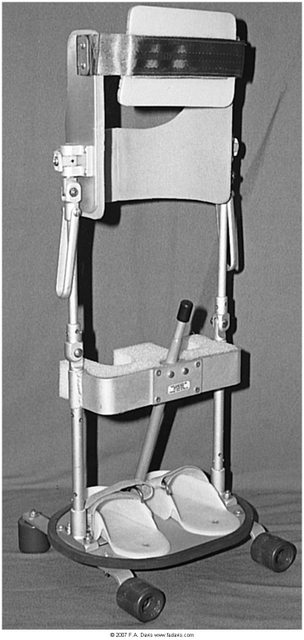 may allow the user (typically a child) to move around using trunk motions
may allow the user (typically a child) to move around using trunk motions
End of Lesson
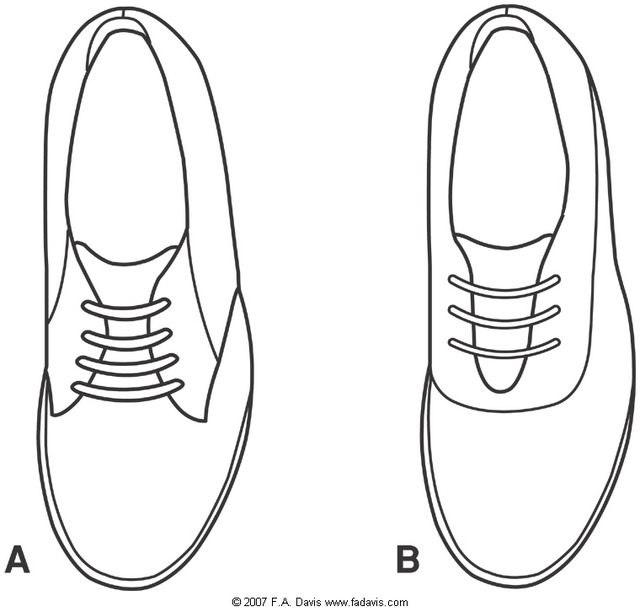 Blucher upper pattern which is most recommended for patients with foot edema, internal shoe modifications and LE orthoses
Blucher upper pattern which is most recommended for patients with foot edema, internal shoe modifications and LE orthoses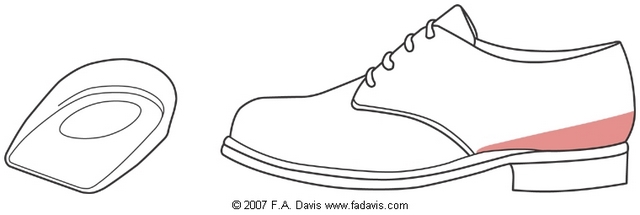 slightly increases plantar flexion and distributes force off of heel
slightly increases plantar flexion and distributes force off of heel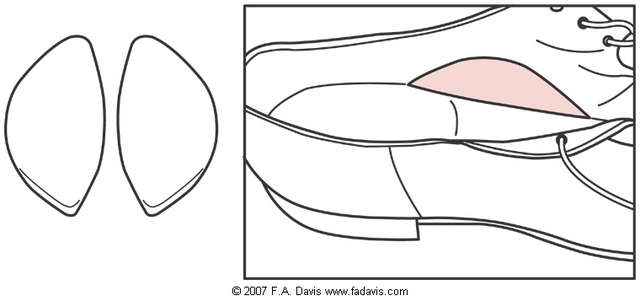 to decrease or control pronation in mid-stance
to decrease or control pronation in mid-stance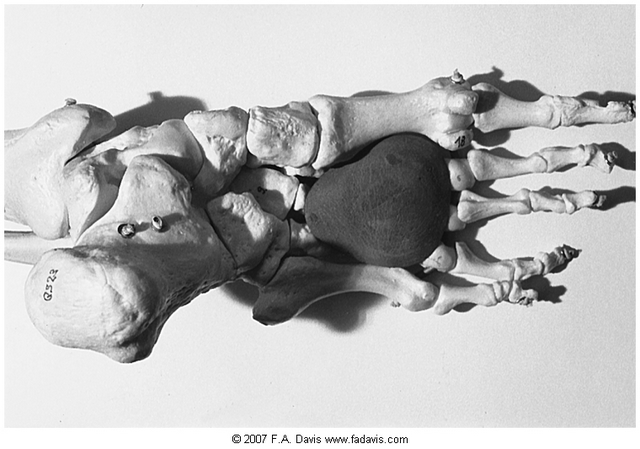 to relieve pressure off MT heads during late stance
to relieve pressure off MT heads during late stance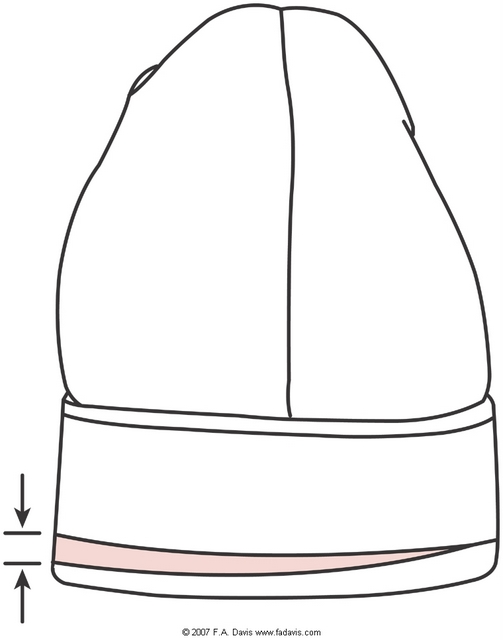
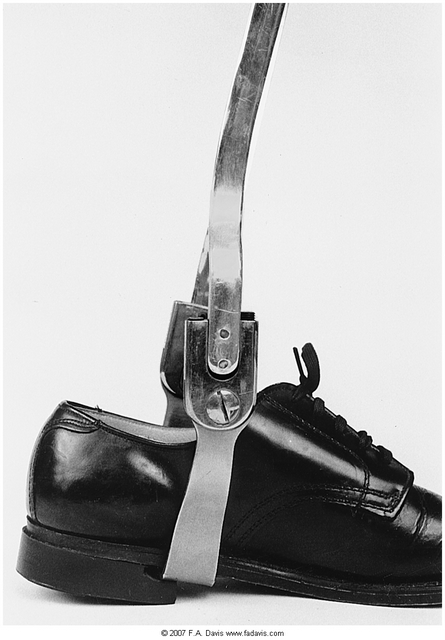 riveted to shoe
riveted to shoe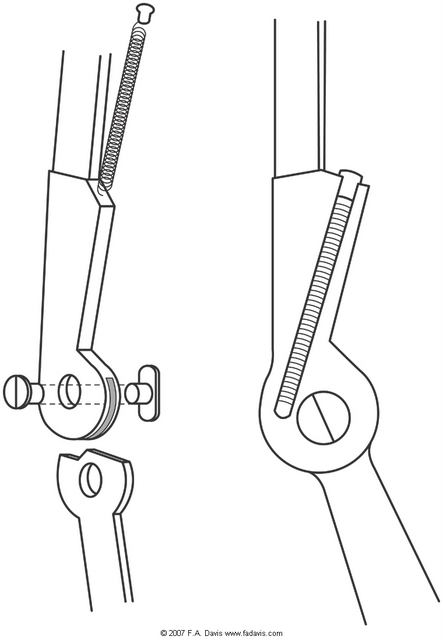
 assists dorsiflexors during pushoff
assists dorsiflexors during pushoff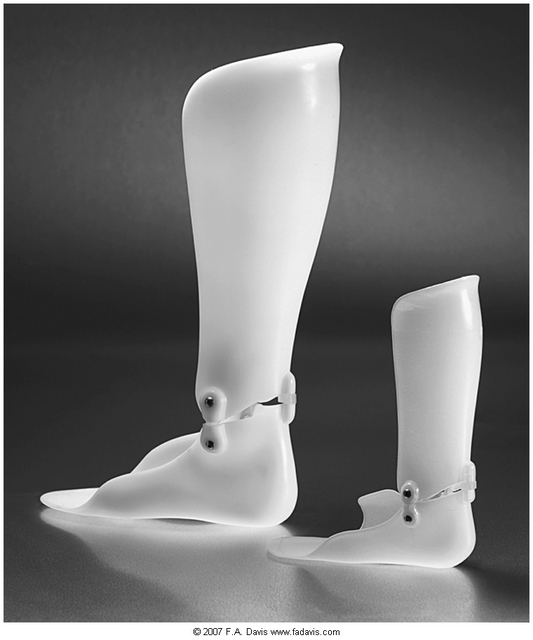
 may allow the user (typically a child) to move around using trunk motions
may allow the user (typically a child) to move around using trunk motions