Fractures
PTA 104 Ortho Dysfunctions
Fracture of bone tissue significantly impacts function and participation in daily activities. Rehabilitation from fracture is a multi-disciplinary approach involving careful coordination with the health care team, patient, and involved family members. Patients often experience barriers within their home and work environments that were previously unnoticed. In this lesson, we will review the pathology and physiology of fractures, appreciate the science basis for post-operative precautions, and apply this knowledge to effective rehabilitation strategies.
The content of this lesson is derived from
Cameron, MH, Monroe LG: Physical Rehabilitation, St. Louis, 2007, Elsevier Mosby.
Kisner, C, ColbyLA: Therapeutic Exercise, Philadelphia, 2007, FA Davis.
Oregon Department of Human Services
After completing this lesson, students will:
Below is a video of my comments and perspectives on the lecture material as it relates to clinical practice.
Disclaimer: it was made in 2014 and I have since reformatted the lecture, so the formatting on the screen will not look the same as what you see in Moodle
Divisions of the Skeleton
Axial skeleton
–Skull
–Hyoid bone
–Vertebral column
–Thoracic (rib) cage
Appendicular skeleton
–Limbs
–Girdles
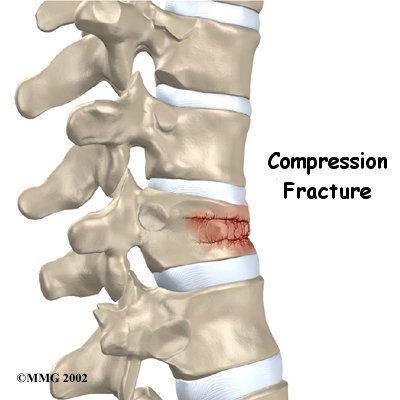
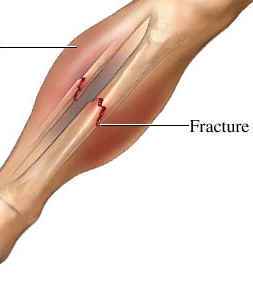
Any break in the continuity of bone tissue (hairline or multi-fragmented (comminuted))
Stress applied to the bone tissue exceeds its strength
Stress applied to the bone tisse is rapid and multi-directional
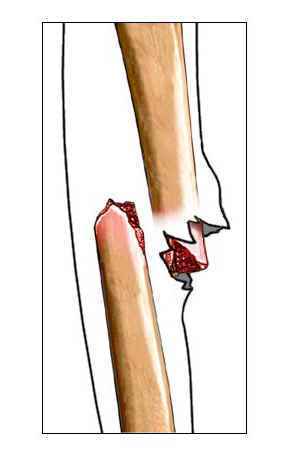
Direct: fracture occurs at point of force impact
Indirect: fracture occurs as a result of compression or rotational force applied at a distance
http://www.nytimes.com/imagepages/2007/08/01/health/adam/1096Fracturetypes1.html

 longitudinal fx
longitudinal fx
http://www.rush.edu/rumc/page-P07392.html
http://www.eorthopod.com/content/spinal-compression-fractures
http://radpod.org/wp-content/uploads/2007/05/calcaneal_avulsion.jpg
calcaneus -- jumping
tibia/fibula -- running
patella -- hurdling
pelvis, obturator ring -- gymnastics
ribs -- heavy lifting, coughing
vertebrae, pars interarticularis -- lifting
scapula, coracoid -- trap shooting
humerus. ulna -- throwing baseball, pitching
hamate -- golf, baseball

http://www.radsource.us/clinic/0803
Bone can be surgically fixed internally or externally with the use of instrumentation.
Fixation devices can be described as stress shielding (no motion to fracture site - primary healing) and stress sharing (distributes forces to minimize motion - secondary healing)
Normal stresses to bone are transmitted through the devices instead of bone tissue, therefore fixation devices are often removed following fracture union to reverse device-induced osteoporosis.
Types of fixation devices are well-described in your Cameron text. Study pages 201 and 202 and check your understanding.
PTAs monitor for signs and symptoms of pre-operative and post-operative complications associated with fracture and fracture repair. Box 12.6 in your Kisner and Colby text provides an excellent summary of complications which may emerge through the healing process. Any suspected signs and symptoms of medical post-operative complications are immediately reported to the supervising PT and/or medical staff (nursing/PCP).
DVTs are blood clots which typically present in the lower limb.
Risk for DVT increases with recent history of cancer, paresis, immobilization/bed rest more than 3 days
Signs and symptoms of DVT include: limb redness, warmth, and swelling (increased limb girth), increased tenderness to touch, increased pain.
DVTs can mobilize (emboli) and result in a life-threatening pulmonary embolus
Exercise and soft tissue mobilization to the affected limb is contraindicated until medically cleared.
The formation and progression of a DVT into a pulmonary embolus is well-described by the National Heart Lung and Blood Institute
Immobilization and CNS suppresive drugs (anesthesia, pain medications, etc), can decrease the efficiency of breathing and airway clearance. Secondary complications of hospitalization due to fracture includes pneumonia and atelectasis (lung tissue collapse).
Premature weight bearing, excessive forces through healing soft tissue, and inappropriate use of orthoses can result in fracture of fixation devices and disruption of internal sutures and surgical anchors. Any sudden increases in pain or losses of function, or inability to progress to WB activities due to pain should be referred back to the supervising PT for further assessment.
Disruption of skin and bone tissue may result in local or systemic infection. Cardinal signs of inflammation, fever, shortness of breath (SOB), decreased cognition (change in arousal, A&O status) must be communicated to medical staff prior to engaging in physical activity. Vital sign monitoring before and during active-assisted and active exercises assure patient safety during activities which increase physiological stress to the cardiovascular and pulmonary systems.
Steps PTAs can take to empower the patient/family member to minimize risk for post-operative complications include:
Phases of post-operative rehabilitation are identified by the stages of healing of soft tissue and bone
|
Maximum Protection |
Inflammatory stage/acute Vigilant protection of tissues May include immobilization May include low-level stresses (e.g., partial, assisted or passive ROM) Isometric exercise to prevent excessive atrophy Physical agents for pain management and tissue healing Ranges from 3-7 days to 4-6 weeks |
|
Moderate Protection |
Subacute/proliferative phase Pain and tenderness is minimal Increased stresses to bone and soft tissue are indicated to restore function Exercises to restore normal kinematics, strength, function Neuromuscular exercises to increase efficiency, coordination and control of movement Physical agents for pain management and muscle re-education Ranges from 4-6 weeks to 8-12 weeks |
|
Minimal Protection/Return to Function |
Begins when full to almost full, pain-free ROM is available Joint mobility is restored and stable Focus is on task-specific, functional activities for the individual patient and prevention of secondary complications ( e.g., fall prevention, endurance) Ranges from 6-12 weeks to 6 months |

Etiology of fracture does not typically allow for pre-operative education and instruction by a PT or PTA. PT evaluations and treatment planning usually begin once the patient is medically stable to progressively increase activity. In order to minimize complications and promote a successful recovery, PTs and PTAs use knowledge of physiological processes to incrementally restore integrity and function of healing tissue while instructing patients in adaptive strategies for altered weight bearing. PTs establish a plan of care based on Impairments (I), Functional Limitations (FL), and Disability (D) and PTAs select interventions in the plan of care to progress patients toward short and long term goals.
The following table provides an example of treatment planning during rehabilitation from fracture based on impairments and post-operative complications:
|
I, FL, D |
Intervention |
PTA role/pt and family education |
Outcome/Method of Assessment |
|
Impaired WB status |
Gait Training |
Use of ambulation aid Use of orthosis Pt/family/staff education on precautions Instruction in gait pattern for condition |
Level of assistance with use/care for ambulation aid Demonstration of most-appropriate gait pattern for stage of healing/function Visual, Verbal and kinesthetic practice and feedback in static and dynamic environments |
|
Impaired endurance |
Therapeutic Exercise |
Progressive increase in functional mobility Progressive increase in muscle strengthening Instruction in energy conservation (pacing, planning, prioritizing, etc.) |
Level of assitance with bed mobility, transfers, balance, gait, locomotion, etc. HR/RR/%O2 sats with activity Upright tolerance in sitting, standing (PLE, BP) Demonstration of motor and activity planning for energy conservation
|
|
Need for prevention of secondary complications |
Therapeutic Exercise |
Instruction in frequent ankle pumps (dorsiflexion, plantar flexion, circles) Use and application of sequential pumps/compressive stockings during early rehab stages Instruction in incentive spirometry Instruction in diaphragmatic breathing Instruction in proper use/wear of orthoses
|
Demonstration and practice of correct technique (bed exs, breathing, brace application, etc) with and without cues Lung volume measurements consistent with expected values
|
|
Impaired skin integrity |
Wound Care |
Inspection of pin sites/surgical incisions Dressing changes Scar mobilization |
Size/characteristics of wound Range of motion Proficiency of patient/family member(s) in skin/wound care |
|
Pain |
Therapeutic Exercise Soft Tissue Mobilization Physical Agents |
Instruction in ROM/stretching Massage techniques for secondary muscle guarding Electrical stimulation, heat, ice, US Instruction in proper use/wear of orthoses Instruction in joint/limb protection techniques
|
Pain levels at rest/with activity ROM measures Proficiency with use/application of physical agent, orthosis, etc. Proficiency with adaptive strategies during recovery phases |
|
Impaired Muscle Performance |
Therapeutic Exercise Physical Agents |
Progressive strengthening appropriate for healing stage NMES |
MMT Limb girth measurements (decreased atrophy) Ability to peform functional activities with least resistrictive/no assistive device Time/endurance measures for sustained cardiovascular activity |
|
Impaired Balance/Coordination |
Therapeutic Exercise |
Progressive activities to maintain center of gravity (COG) within base of support (BOS) in predictable and unpredictable environments |
Formal balance assessment (e.g. Berg) Time in standing Functional reach testing Balance strategy appropriate to activity |
|
Impaired joint mobility |
Therapeutic Exercise |
PNF Manual stretching Instruction in self-stretching |
ROM Demonstration of correct stretching with/without cues (patient and/or family)
|
PTAs can be the "eyes and ears" of the PT during direct patient care, family training, and interdisciplinary care meetings. PTs rely on PTAs to gather data and make comparisons so that patients are treated within the scope of PT practice safely and effectively. In some cases, a supervising PT may not be immediately available, therefore, PTAs understand signs and symptoms which require immediate medical attention. Significant adverse findings which would require immediate communication to the supervising PT/medical staff include:
Complications specific to fracture and fracture repair include delayed or non-union of bone tissue. PTAs often see patients successively over a period of time, and can assess if patient progress is consistent with fracture healing as measured by decreased impairments and functional limitations. PTAs develop relationships and rapport with family members and caregivers and can advise the PT on discharge readiness and planning based on safety, family training outcomes, equipment needs, and home assessments.
The level of functional limitation and disability is influenced by general health status and psychosocial factors. PTAs play an important role in integrating effective communication, respect for individual and cultural differences, and motivation techniques into the rehabilitation process. The PT/PTA team should coordinate with family, interdisciplinary staff, and community resources to promote optimal safety, health and wellness following a fracture.
Key factors which influence outcomes include
Fractures are the second most common injury in child physical abuse. Certain fractures are more specific indicators of abuse. Common but low specificity indicates typical presentation in childhood without consistent or significant evidence of child abuse.
Every state has laws in place to define and protect children from abuse and neglect. Oregon's definitions and resources can be referenced through the Department of Human Services
By Oregon law, PTAs are Mandatory Reporters of child and elder abuse and neglect. If a licensed PTA suspects abuse/neglect, there is a legal obligation to report the alleged abuse to law enforcement or the Department of Human Services.
The following statistics are from the 2009 Child Welfare Data Book published by DHS
67,885 reports of abuse and neglect were received.
28,584 reports were referred for investigation.
7,240 referrals were founded for abuse or neglect—involving 11,090 victims.
48.1 percent of victims were younger than 6 years old.
Threat of harm was the largest type of maltreatment incident experienced by victims (49.8 percent of incidents), followed by neglect incidents (31.1 percent of incidents).
At 42.1 percent, alcohol and drug issues represented the largest single family stress factor when child abuse/neglect was present.
The next most common stressors were domestic violence (31.7 percent) and parental involvement with law enforcement (27.0 percent).
During 2015 Oregon DHS received 69,972 reports of suspected child abuse or neglect. Of those, 32,682 reports were referred for investigation.
Of the reports referred for investigation, 6,708 were founded for abuse or neglect involving 10,402 victims; 46.6% were younger than 6 years old.
Public and private officials required by law to report suspected child abuse and neglect made 76 percent of the reports of abuse and neglect received by DHS.
Of all reports, 38.0 percent came from schools and law enforcement agencies.
10.6% of all reports of child abuse in Oregon were filed by medical personnel
There were 676 founded child abuse cases in Lane County; 606 founded cased in Jackson County, and 215 founded cases in Josephine County
Oregon Department of Human Services. 2015 Child Welfare Data Book. State of Oregon. Web 1 April 2016.
Guidelines to responding and reporting to accounts of abuse are found on the Oregon Department of Human Services website.
PTAs can access the "Report Child Abuse and Neglect" link to identify local child welfare offices by county in order to expedite the reporting process.