Arthritis
PTA 104 Orthopedic Dysfunctions
Arthritis
Refers to any inflammation of joint/joint structures. Most common forms are osteoarthritis and rheumatoid arthritis, respectively.
Signs and Symptoms
- pain
- impaired mobility (typically a capsular pattern)
- chronic - firm end-feel
- acute - guarded end-feel
- includes effusion
- loss of accessory joint motion
- impaired muscle performance
- muscle length-tension relationships
- inadequate activation or guarding of postural stabilizers
- impaired balance
- joint degeneration limits feedback from proprioceptors
- functional limitations
- may need adaptive equipment to complete a functional activity or to protect joint(s) from further injury
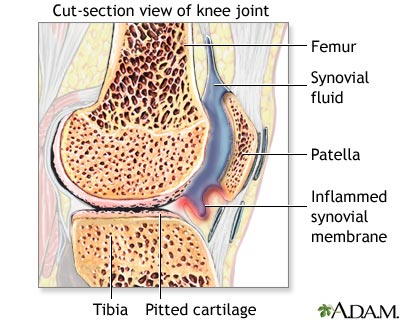
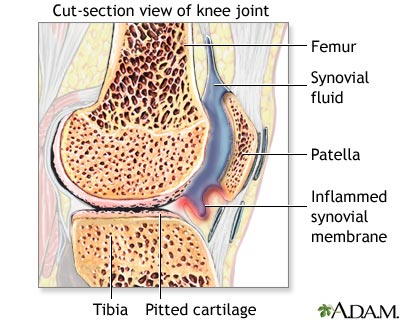
Osteoarthritis
A chronic, degenerative disorder primarily affecting the articular cartilage of synovial joints, with eventual bony remodeling and overgrowth at the margins of the joint
Background and Characteristics
- Refers to degeneration and inflammation of bone and cartilage in articulating (moving) areas
- Pain with weight bearing and joint motion can progress into partial to full loss of motion and pathological fusion (ankylosis)
- Osteophytes (bone spurring) may be identified on x-ray or diagnostic imaging

- http://www.medical-look.com/Joint_pain/Osteoarthritis.html
- Pathological bone remodeling can lead to ligamentous laxity and joint hypermobility/instability
- Can result in secondary nerve or postural dysfunction due to loss of joint height/space
- Symptoms are exacerbated with overuse, weather changes, or prolonged immobilization
- Associated with advanced age, lifestyle habits (sedentary, obesity, high-impact sports, repetitive loading/lifting), and family history
Principles of Management of Osteoarthritis
- Patient instruction
- Pain management—early stages
- emphasis is on reducing joint stiffness, balancing activity and rest, and reinforcing the role of movement in joint health
- Pain management—late stages
- consider modalities for home use, pacing and prioritizing, modifying activities
- Assistive and supportive devices and activity
- bracing, aquatics, assistive devices for ADLs, home and environmental modifications
- Resistance exercise
- emphasis is on strengthening within non-painful ranges, isometrics to minimize disuse atrophy
- open chain activities with resistance across long lever arms can increase joint loads and exacerbate arthritis symptoms
- Stretching and joint mobilization
- assisted and patient instruction in safe and effective technique
- involved joints typically have a firm end-feel due to bony changes in the articulating areas
- Balance activities
- Aerobic conditioning
- patient education on exercise parameters, including low impact-low joint stress activities
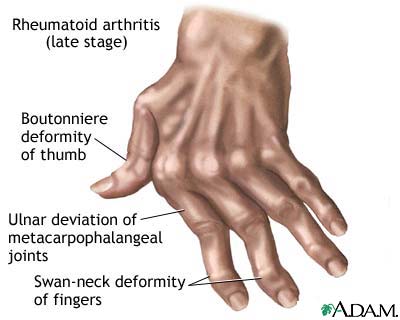
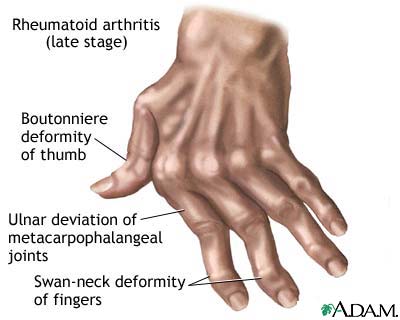
Rheumatoid Arthritis
An autoimmune, chronic, inflammatory, systemic disease primarily affecting the synovial lining of joints as well as other connective tissue. It is characterized by a fluctuating course with periods of active disease and remission.
Background and Characteristics
- Source of pain is inflammation of the synovium
- Typically presents bilaterally, with >=3 joints involved, redness and increased skin temperature
- Higher incidence in women and can be diagnosed in childhood (Juvenile Rheumatoid Arthritis (JRA)
- Autoimmune response is thought to be trigger by some bacterial or viral exposure
- Some association with family history and presence of rheumatoid factor (RF) in the blood
Principles of Management of Rheumatoid Arthritis
Acute Inflammatory Period
- Joint protection
- especially the smaller joints in the hands and feet
- spinting to protect from subluxation due to hypermobility from synovial degeneration
- includes patient instruction in correct exercise technique to prevent further joint stresses during activity
- Energy conservation
- Joint mobility
- stretching is NOT performed when joints are swollen (increased risk for subluxation)
http://arthritis.about.com/od/rheumatoidarthritis/ss/pictures_photos.htm
- Exercise
- PROM, AAROM, AROM depending on pain and swelling in affected joints
- Functional training
- similar to OA; instruction in methods to incorporate joint protection in everyday activities
Subacute and Chronic Stages
http://arthritis.about.com/od/rheumatoidarthritis/ss/pictures_photos.htm
- To improve function, exercise should be aimed at improving flexibility, muscle performance, and cardiopulmonary endurance
- Nonimpact or low-impact conditioning exercises such as swimming and bicycling
- Group activities such as water aerobics
Self-Assessments
Test your knowledge on characteristics of OA versus RA