Pregnancy and movement disorders
PTA 104 Orthopedic Dysfunctions
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Prior to clinical education, our priority is to direct you towards tools and resources to ensure your selected interventions and patient communications are safe. The purpose of this lesson is to introduce some of the more common considerations and conditions for pregnant patients you may work with clinically or in settings specific to prevention and wellness promotion. More practice of exercise, positioning, and exercise modifications, and post-pregnancy pathologies (pelvic floor dysfunctions) will be offered in PTA 205/205L. Remember, pregnancy is considered a state of wellness.
|
Weight Gain |
Averages up to 25-27 pounds; range associated with maternal BMI Increases stress to pelvic ligaments, which have higher elastic qualities |
|
Change to thorax |
Hormonally-induced: results in increased chest diameter, ribs flaring up and out |
|
Ventilation |
Work of breathing increases 15-20% due to increased demand, hyperventilation during pregnancy and dyspnea with mild exercise mid and late-term |
|
Blood volume |
Increases 35-50% |
|
Blood pressure |
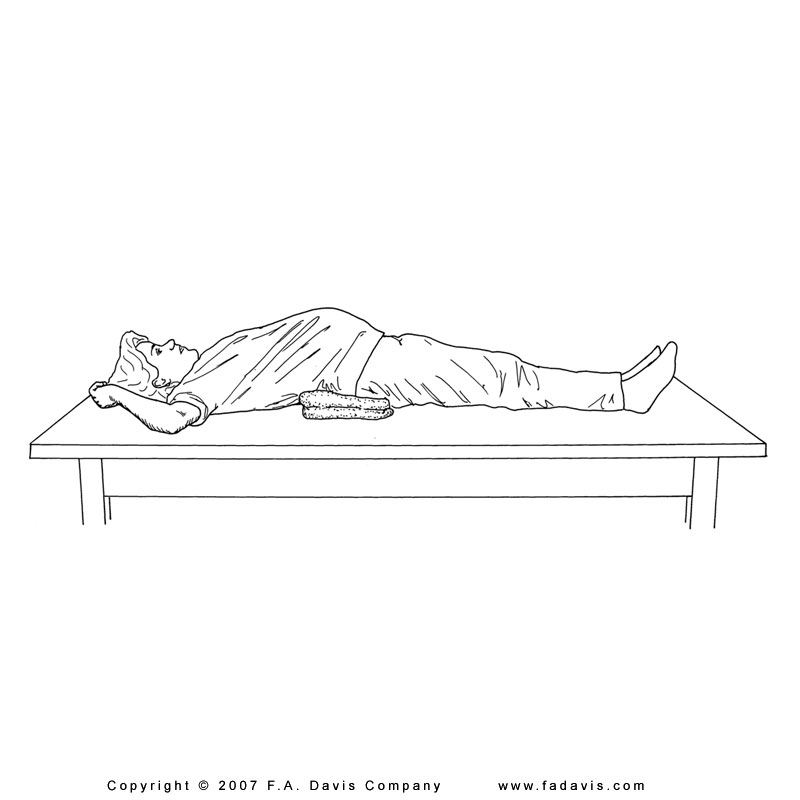
Decreases in early pregnancy; pressure of uterus on inferior vena cava (IVC) in supine may result in hypotension; venous distension increases in LEs. Signs and symptoms of hypertension may result in serious and/or critical health compromise in the pregnant woman and fetus |
|
Heart Rate |
Increases by ~ 10-20 bpm by full term; arrhythmias may develop during pregnancy |
|
Cardiac output |
Increases by 30-60%; L side lying position minimizes compression from uterus to aorta |
|
Musculoskeletal |
Abdominal muscles are maximally lengthened and functionally weaker Reduced ligamentous strength throughout results in hypermobility/instability of joints and fascia Increased demand on pelvic floor muscles Postural compensations with potential long-standing changes |
|
Metabolic |
Average 300 Kcal/day needed during pregnancy due to increased metabolic rate |
|
Endocrine |
Enlarged adrenal, thyroid, parathyroid, and pituitary glands; relaxin and other hormones increases laxity |
|
Neurologic |
Nerve plexi and peripheral nerve compression due to fluid accumulation and structural changes |
|
Gastrointestinal |
"Morning sickness", nausea and vomiting; increased likelihood of reflux, constipation, heartburn, hemorrhoids, etc. |
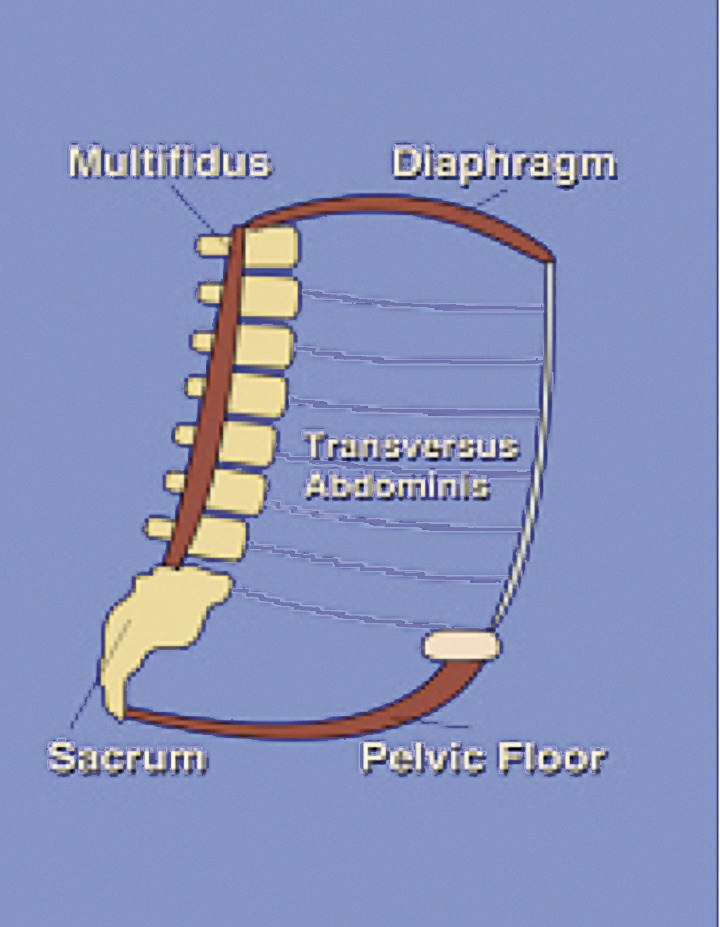
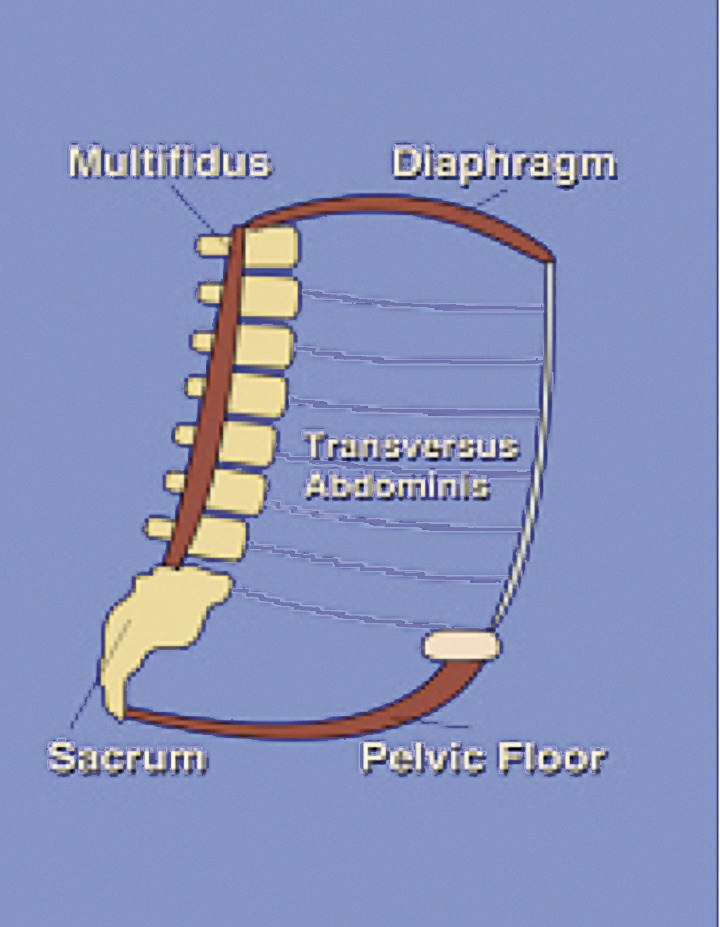
Abdominal lengthening, pelvic floor lowering, diaphragm elevation, and increase laxity all contribute to movement dysfunctions and neuromuscular and/or musculoskeletal pain and decreased movement function with pregnancy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987347/
![]() http://www.flickr.com/photos/mahalie/144905384/
http://www.flickr.com/photos/mahalie/144905384/
Hypertension
|
Monitor BP at rest and during activity and check for signs and symptoms of emerging hypertension, such as headache, altered vision, significant shortness of breath |
Diastasis Recti
|
Separation of rectus abdominus at linea alba; Diagonistic criteria is >=2cm; condition is not exclusive to pregnancy; may result in abdominal herniation requiring surgical intervention |
Postural Back Pain
|
Prevalence is 50-70%. Treatment plan is similar to treatment in patient population where instability, body mechanics, and postural compensations are primary impairments. Deep heating agents, electrical stimulation and traction are generally contraindicated. May also present as peripartum posterior pelvic (SI) pain |
Coccydynia |
Pain in coccyx (tailbone) region; painful sitting; may require manual adjustment for pain relief |
Symphysis Pubis Dysfunction and Diastasis Symphysis Pubis
|
Pubis separates; Pain when lifting one leg at a time, in/out of bed and car, walking up stairs, and transitional movements. Symptoms may not be relieved with rest or decreased WB. Emphasis is on exercise and activity modification and stabilization to decrease torsion. May benefit from a stabilization belt or Mother-to-Be corset
|
Varicose Veins
|
Increased leg discomfort or "heaviness". Increased risk for DVT due to stasis in LEs. May need compression stockings to facilitate venous return. Can also affect pelvic floor vessels (hemorrhoids)
|
Joint Laxity
|
Decreased tensile strength during pregnancy and up to 5+ months post-partum; Emphasis is on activity modification and aerobic exercise which minimized WB stresses |
Nerve Compression
|
Attributable to postural changes, fluid retention, hormonal changes, circulatory changes. Carpal tunnel incidence is higher during pregnancy. May benefit from splinting as well as activity modification to decrease stress/strain to nerve pathways |
Cesarean Birth |
Gentle mobilization of soft tissue and postural/body mechanics education; instruction in anterior lumbopelvic splinting techniques during acute healing phase to protect incision from strain |
Urinary Incontinence |
Although predominantly related to pregnancy, diastasis recti, a separation or stretch of the linea alba can occur in men
![]()
![]()
If any of these are observed during supervised exercise, communicate with your supervising PT and their physician. PTAs educate patients in signs and symptoms of overexertion for self-monitoring during unsupervised exercise
Recall your knowledge of general medical conditions: when there are signs and symptoms of infection, inflammation, or metabolic disorders, exercises may require modification or physician clearance may be needed to insure exercise can be applied safely.
Patients in high risk pregnancy categories may not be able to safely participate in any form or mild to moderate exercise. Absolute contraindications include:
![]()
![]()