Skeletal Demineralization
PTA 104 Orthopedic Dysfunctions
Skeletal Demineralization
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution for commercial purposes. It is not intended to serve as medical advice or treatment. Contact howardc@lanecc.edu for permissions.
For Your Info Only
Additional links are included in the 'sidebar' of your interactive lecture. These resources are for your information only and may help in the future with patient education in clinical practice
Reading and Study Tips
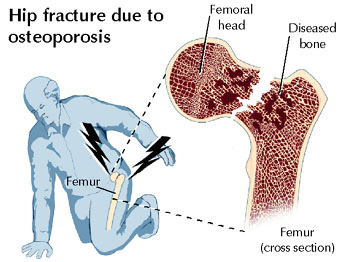
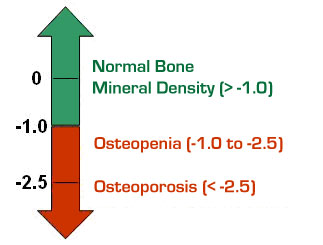
- Cameron discusses T-scores and bone density data. The take home message for this section is the standard deviations from normal bone density which determines diagnostic criteria. This information is reinforced in the interactive lecture
- Normal Bone Physiology should be review from your A&P. You will not be tested on your knowledge of normal bone physiology, but you will need to apply previous knowledge to understand the basis for interventions
- you will not be asked to distinguish between type I and type II bone loss (Table 3.1)
- concepts are summarized well in Box 3.1 and represents the depth of knowledge expected for the exam
- risk factors are important and are also reinforced in the lecture
- Examination - skim this section for a general understanding of a PT evaluation (skim pp. 22-23)
- reinforce your understanding of the role of the interventions featured in the major headings for this section.
Objectives
- Describe risk factors for skeletal demineralization
- Identify clinical indicators for bone loss
- Describe the role of PT in bone loss prevention
- Select appropriate exercises for patients with osteoporosis
- Explore resources for patient education in fall-risk management associated with osteoporosis
What is bone demineralization?
Imbalance between bone formation and bone resorption
Homeostatic mechanisms such as mechanical forces, nutrition, hormonal function (e.g., parathyroid, gonads) work to progressively replace and restore bone tissue to an ideal density. Failure to maintain balance between osteoblastic (bone forming) and osteoclastic (bone resorbing) systems results in loss of bone tissue.
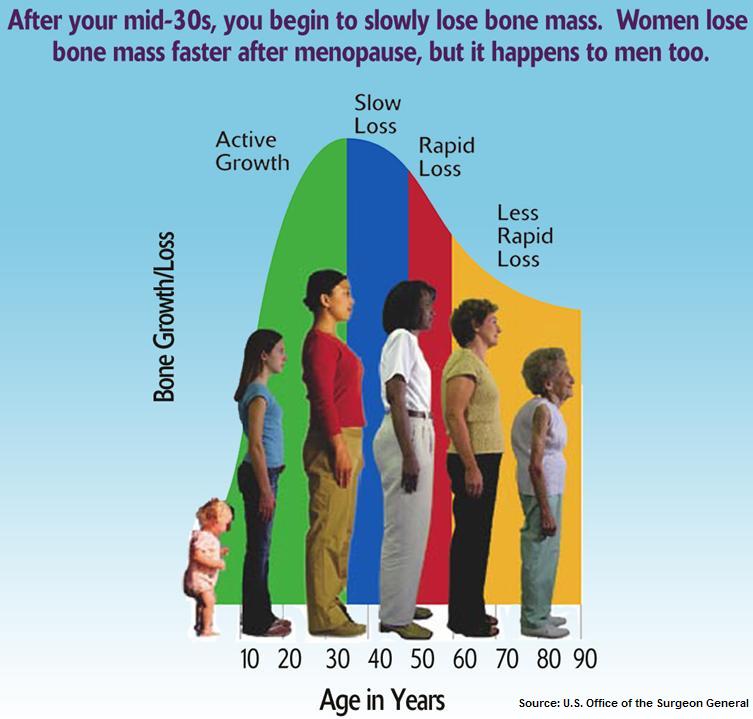
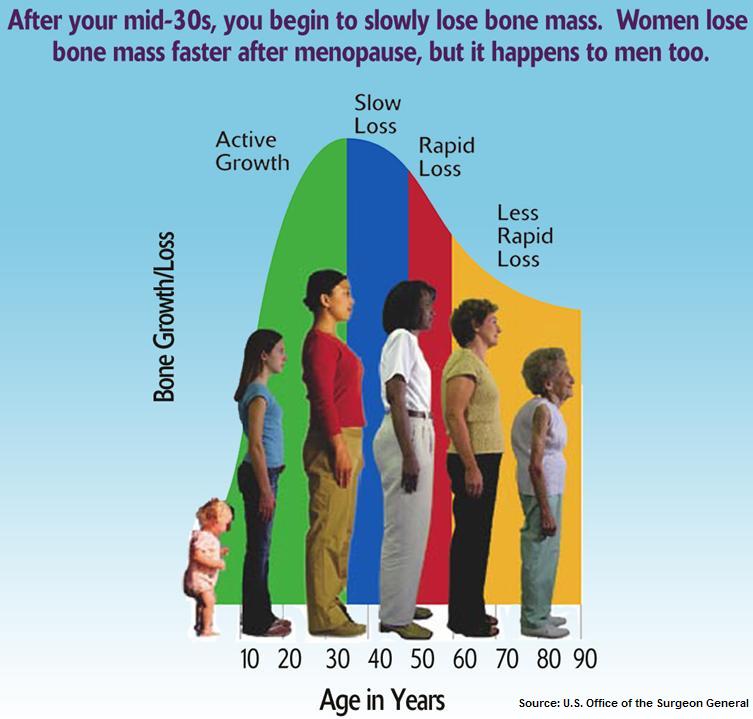
Peak bone mass is typically maintained between ages 25-40
Terms
- bone mineral density
- osteopenia - low bone mass (thinning)
- osteoporosis - significant loss of bone mineral density (porous)
- vertebroplasty - surgical procedure where cement-like substance is injected into affected vertebral bodies post-compression fracture to increase strength of axial bone tissue and decrease pain
- kyphoplasty - surgical procedure where collapsed area in vertebral body is inflated and then injected with bone cement post compression fracture
Incidence of Involutional Bone Loss
- most common in women
- women lose 35-50% of trabecular bone mass, 25-30% of cortical bone mass
- more common in low body weight, slight frame body type
- most common in caucasians and asians
- loss of BMD is associated with aging, menopause, estrogen deficiency throughout the lifespan
- secondary bone loss/osteoporosis is correlated with
- associated with corticosteroid use (i.e., treatment of RA or other autoimmune disorders/immunosuppressives)
- nutritional influences include: eating disorders, food insensitivities, alcohol use/abuse, low calcium intake, low Vitamin D
- environmental: decreased exposure to sunlight results in lower Vitamin D concentrations
- lifestyle influences: decreased WB activity, smoking, caffeine (studies vary)
APTA PodCast on Osteoporosis
Clinical Significance of Bone Loss
- low BMD is a valid predictor of fracture risk
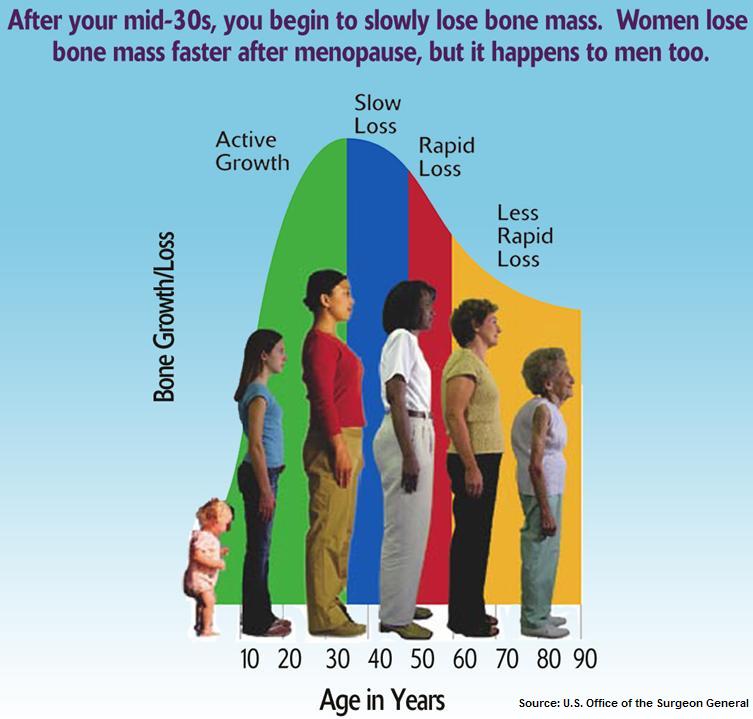
- common fractures: vertebral (compression), Colles's (distal radius with/without ulna) and hip
- fractures may precede trauma (spontaneous fracture causes the fall)
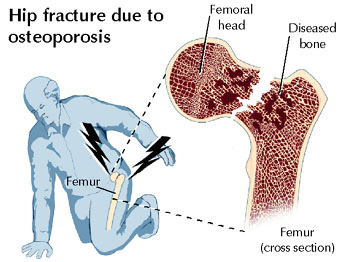
- disability and mortality rates associated with fracture are higher in population with lower bone densities
- increased rate of transition to skilled and assisted living settings post-fracture with osteoporosis
- prolonged immobilization due to illness or injury results in bone tissue loss
- activities requiring sustained or repeated trunk flexion may increase risk for compression fracture in the spine
Clinical Indicators of Bone Loss
- bone density studies (BMD)
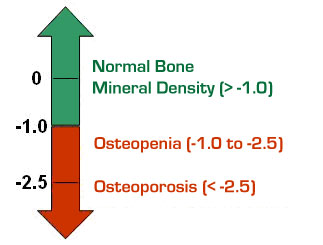
- outpatient procedure which measure bone density at the wrist, spine, hip, or calcaneus
- increased thoracic kyphosis
- loss of vertical height greater than one (1) inch
- stiffening of anterior trunk structure
- decreased shoulder flexion, ankle dorsiflexion, and hip extension
- decreased strength (hip extension, knee extension, abdominals, trunk extensors)
- trunk and/or visceral pain, radiating rib pain; point tenderness on spine
- fall risk on balance assessments
- Tinetti Assessment Tool
- Berg Balance Scale
- Supine Sign
- See Table 3-2 in Cameron and Monroe for a summary of clinical findings and prognoses
Interventions
increase bone mass, slow bone loss, and/or reduce the risk of fractures.
Weight bearing aerobic exercise
depending on the severity of osteoporosis, patients may exercise in a weighted vest to stimulate osteoblastic activity
Resistance exercise
consistent effects are generally noted in spine bone density
flexion activities (sit ups, abdominal machines) can increase pressure on compromised vertebral bodies and increase risk for fracture
no combined flexion with rotation exercises in trunk
limit closed chain hip internal/external rotation activities to decrease torsion through femoral neck
avoid high velocity, high impact activities
begin weight training at low intensities with low repetitions (6-8) to minimize fracture risk; progress to 1-3 sets of 8-12 repetitions of resisted exercise
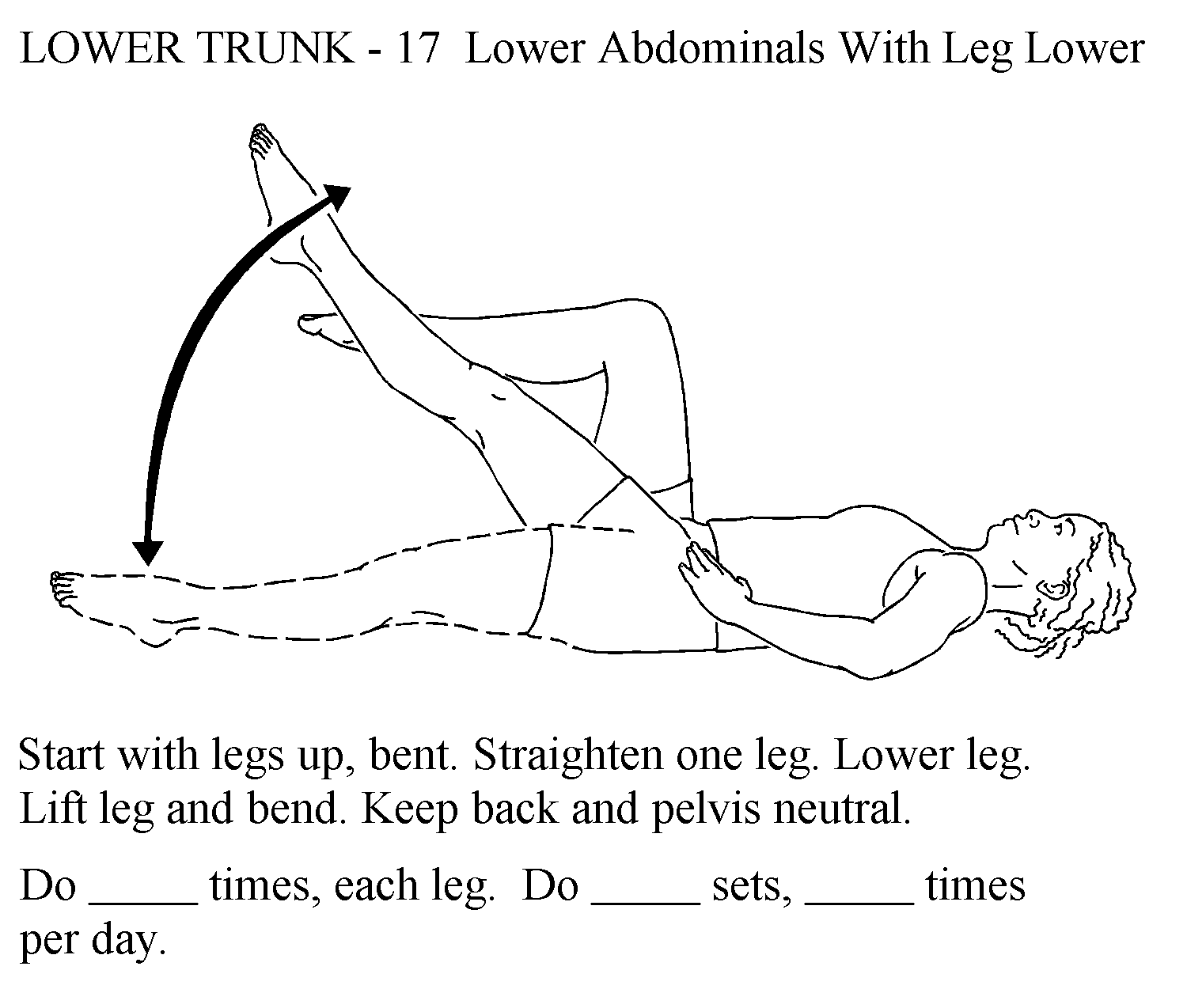
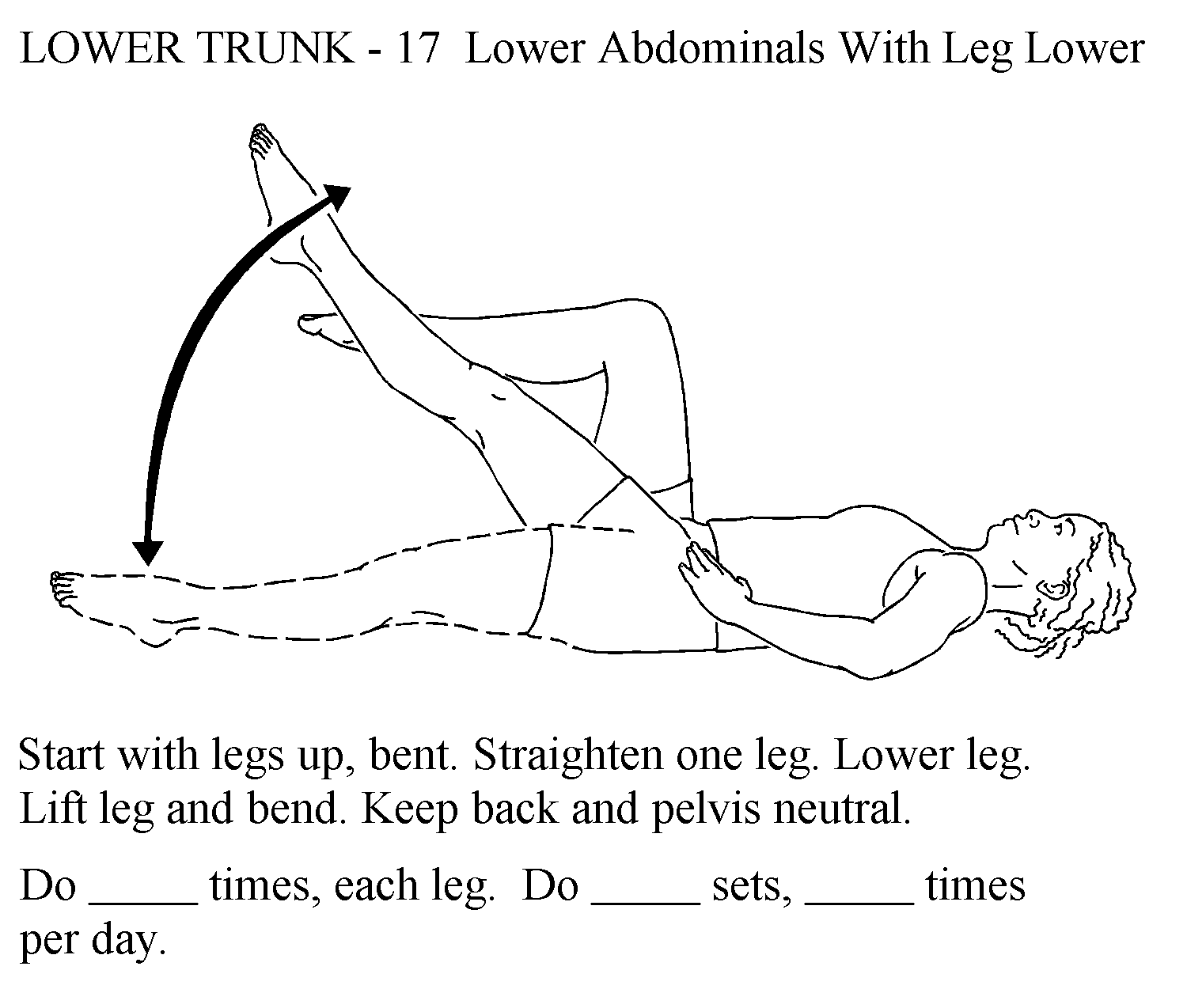
an alternative to a curl up for abdominal strengthening is a straight leg raise with a stable lumbar and pelvic spine
Spine exercises
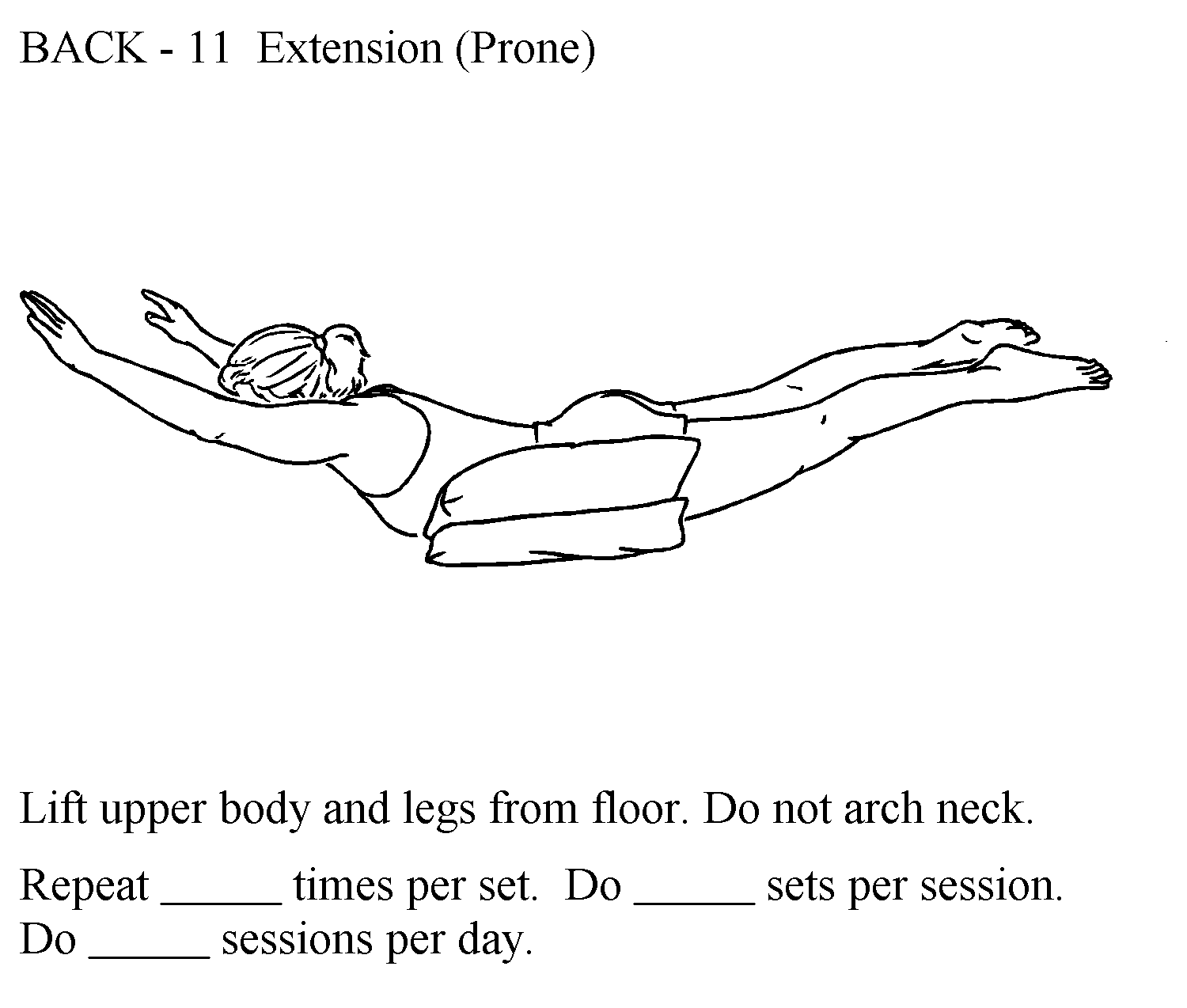
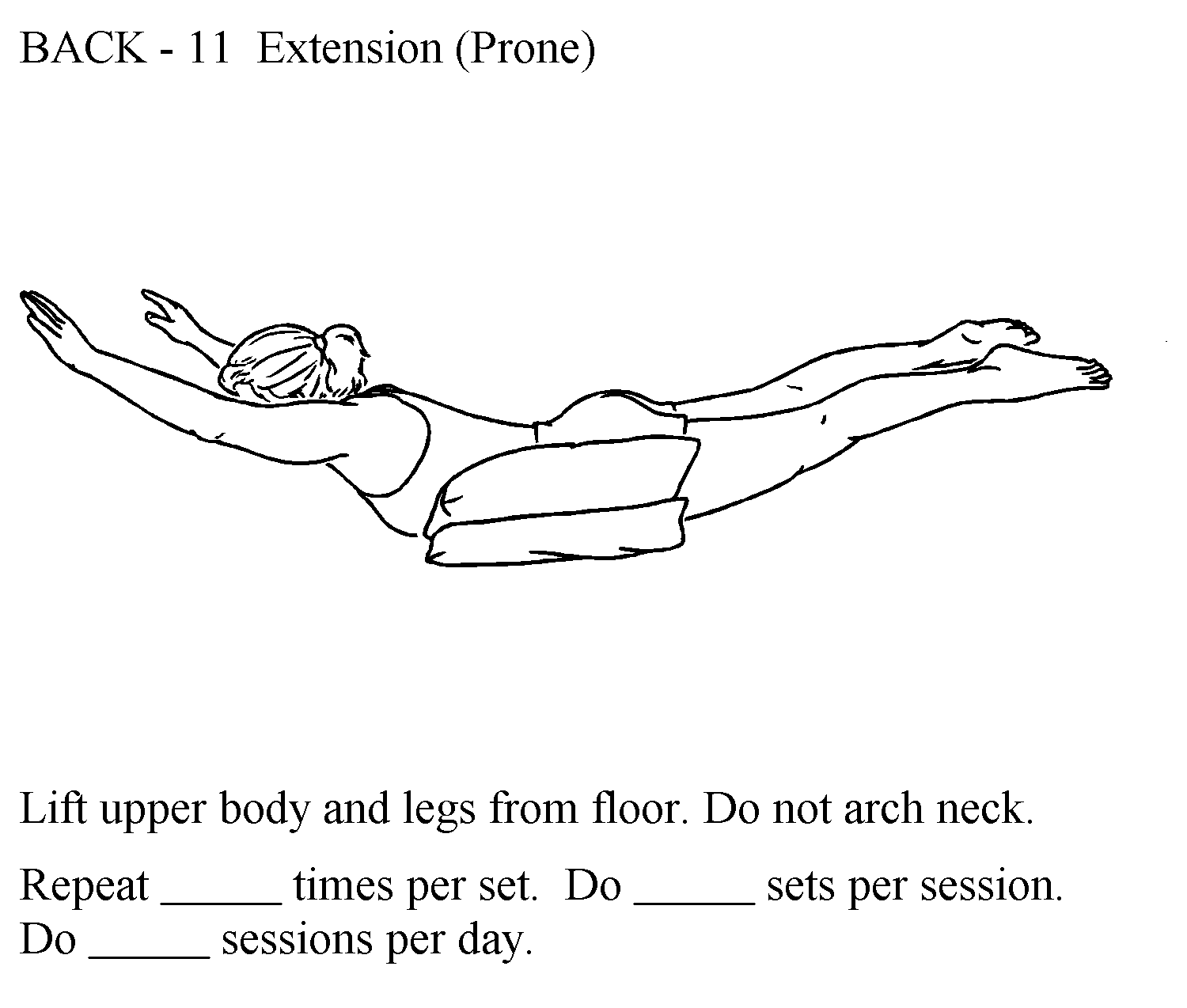
strong evidence that back extension exercise can markedly reduce compression fracture risk
Body Mechanics Training
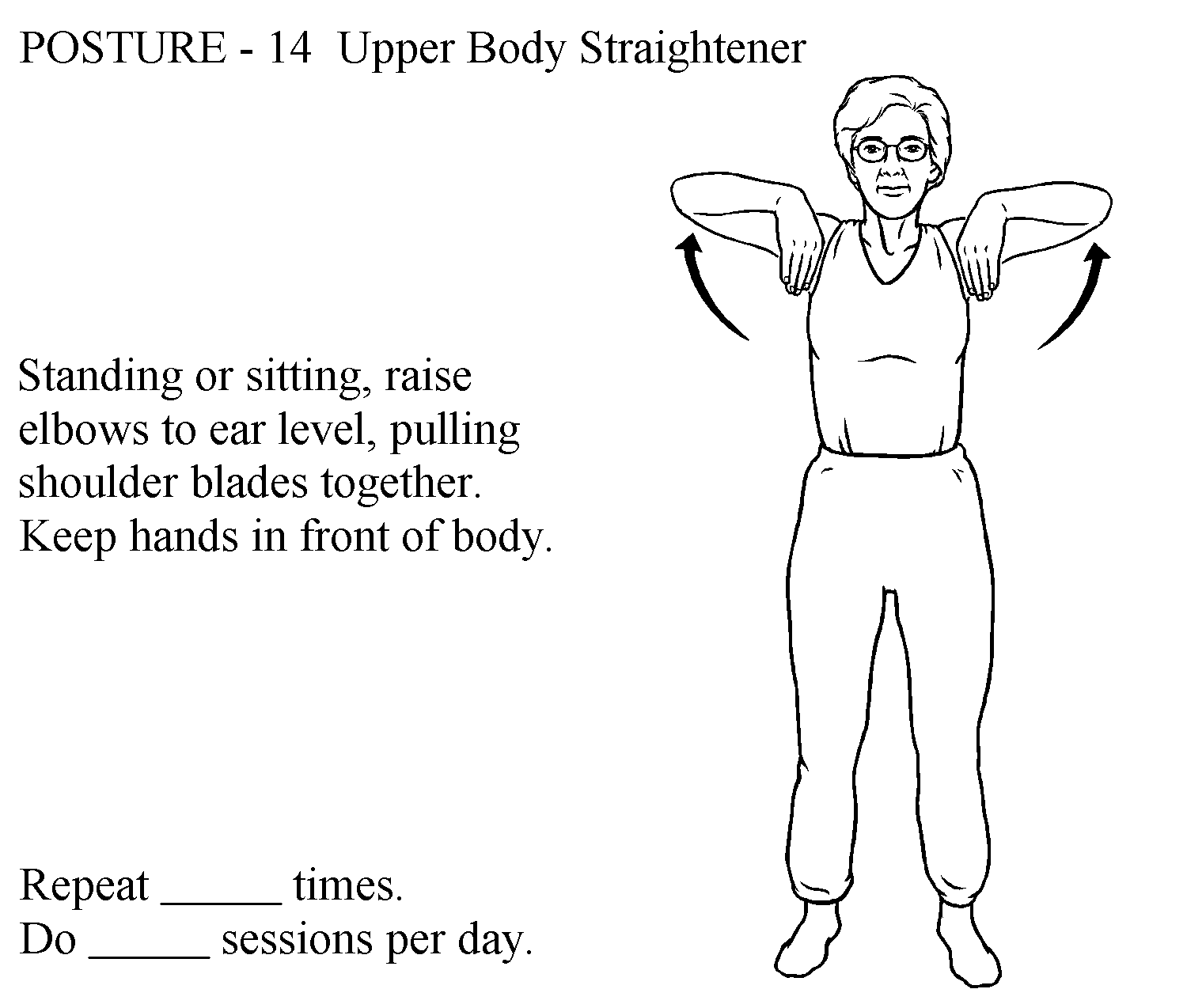
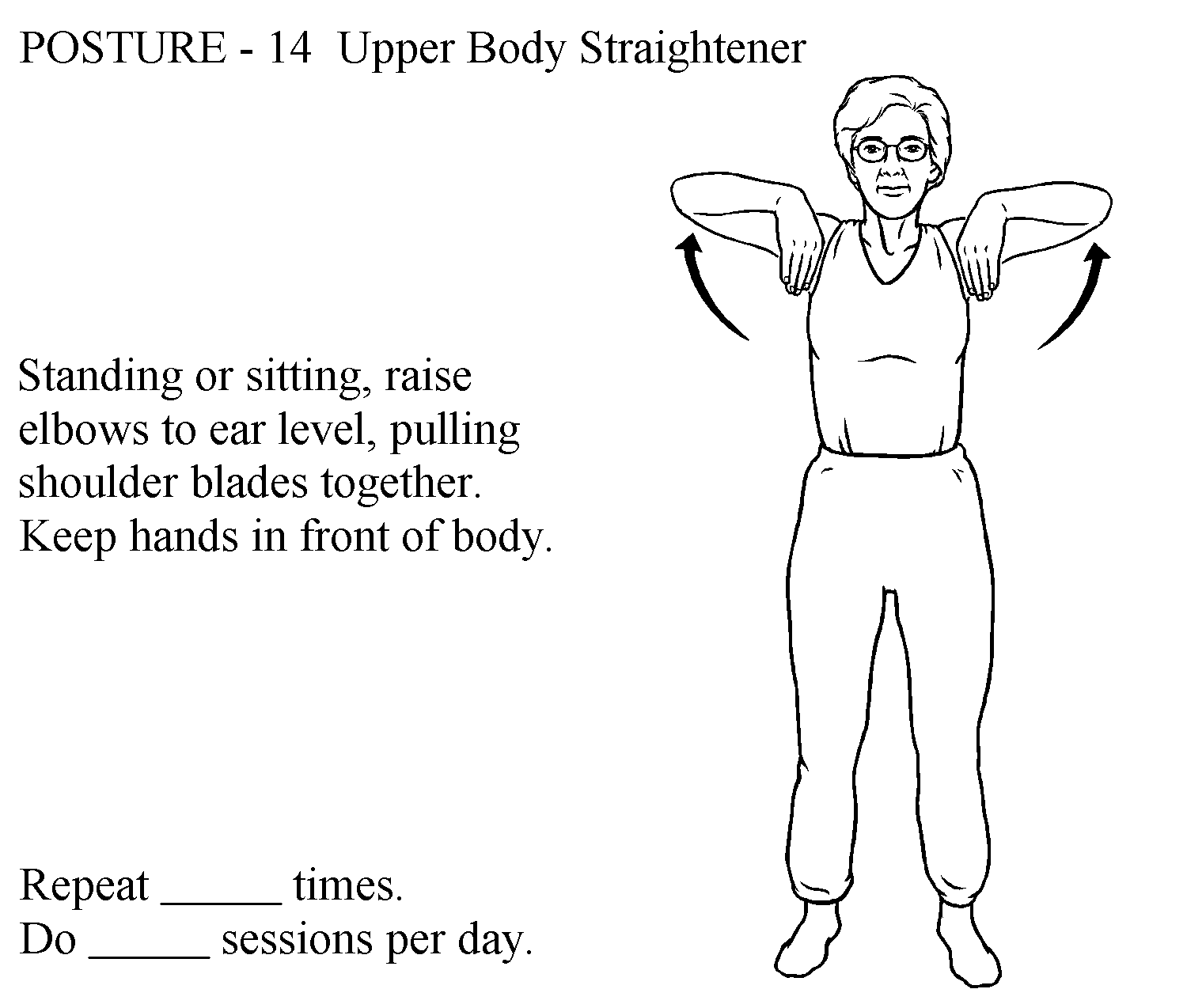
- posture awareness: emphasis on increasing control and activation of trunk extensors during postural activities, ADLs, and iADLs
- hip hinging
- hip and back extensor strengthening
- log rolling for bed mobility
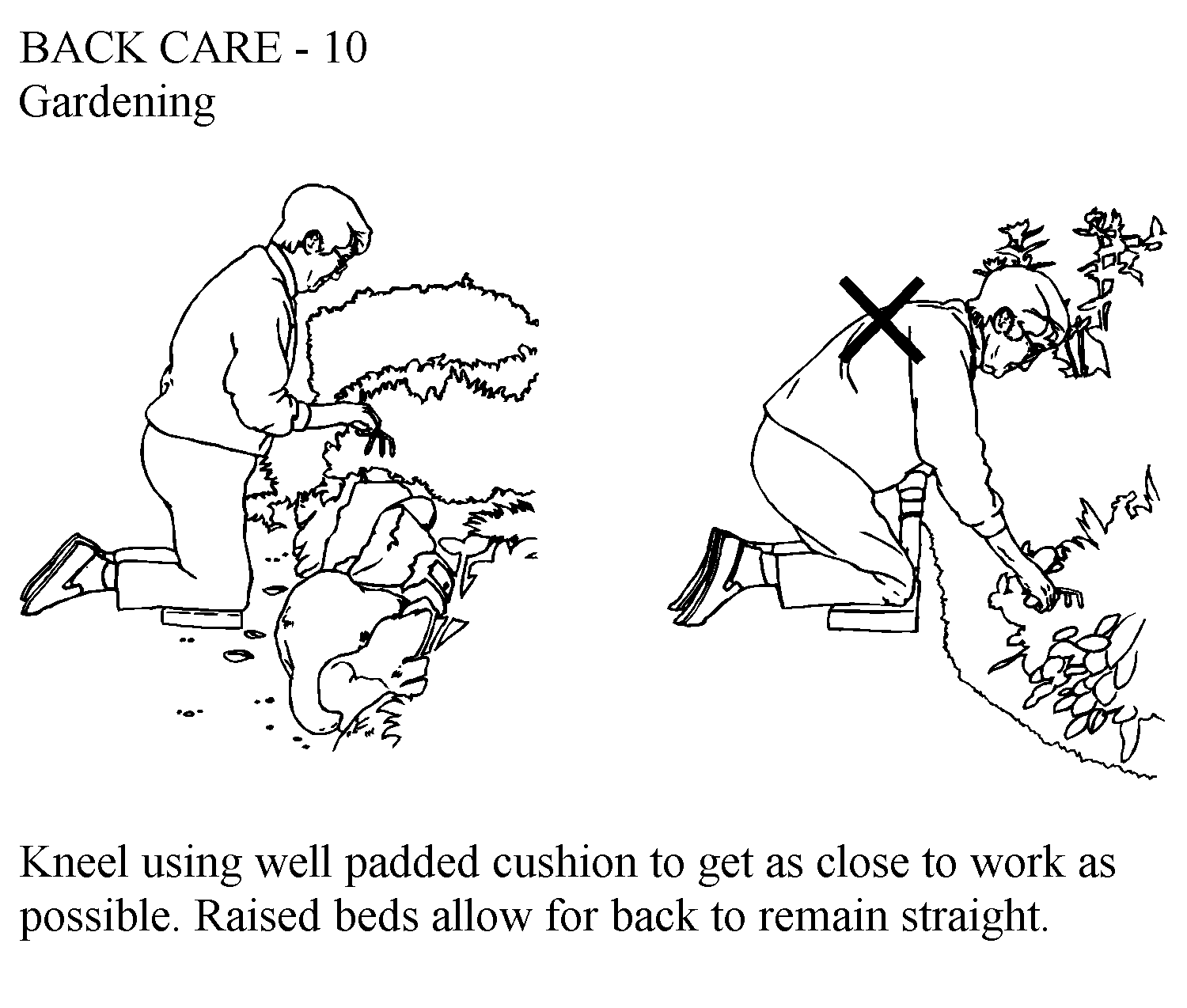
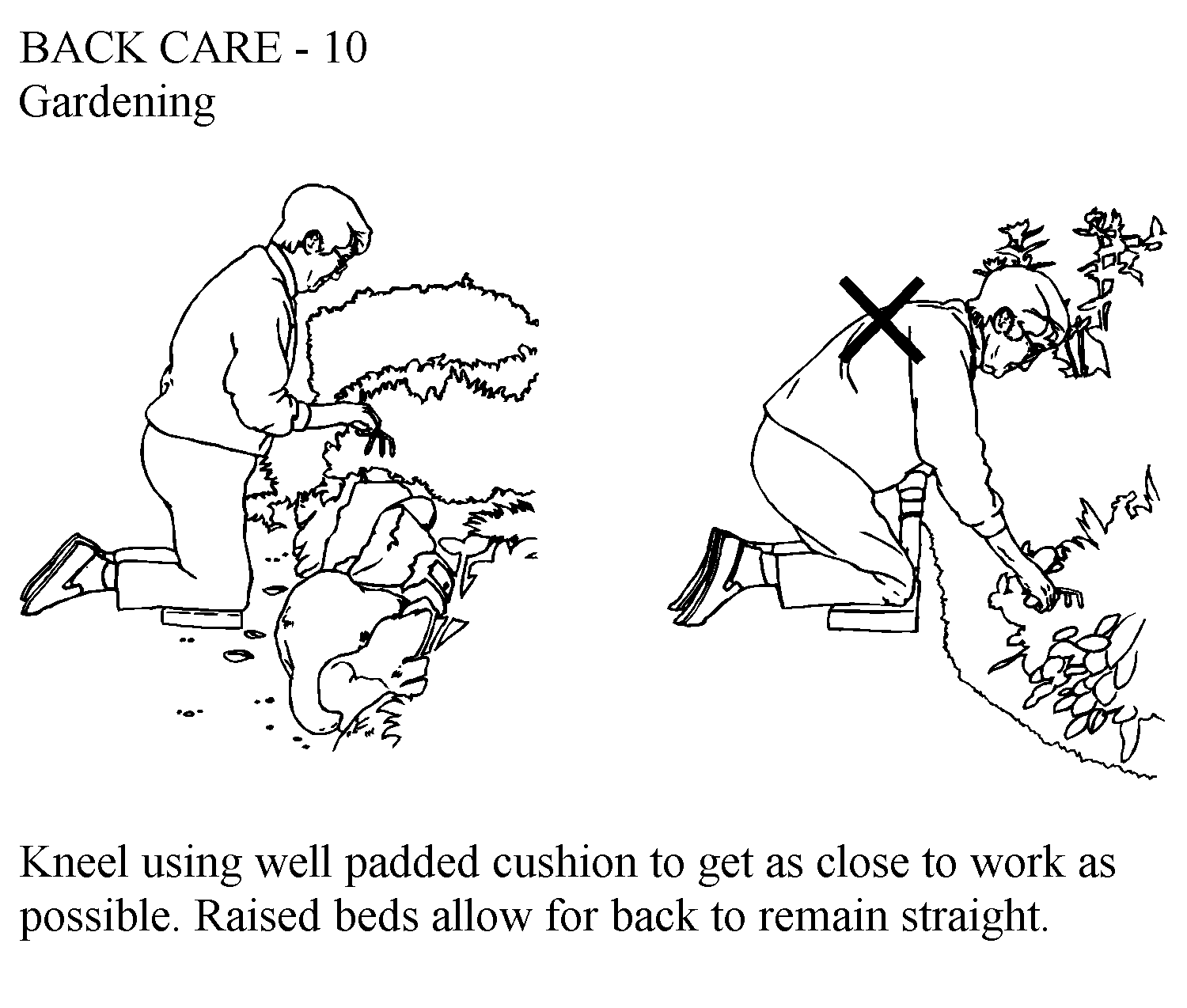
- correct body mechanics for push/pull, lift, carry, etc.
Visit this recent New York Times Article about patient-centered interventions for fall prevention:
Orthoses
spinal orthoses can be customized or prefabricated for pain management and joint protection
Fall prevention
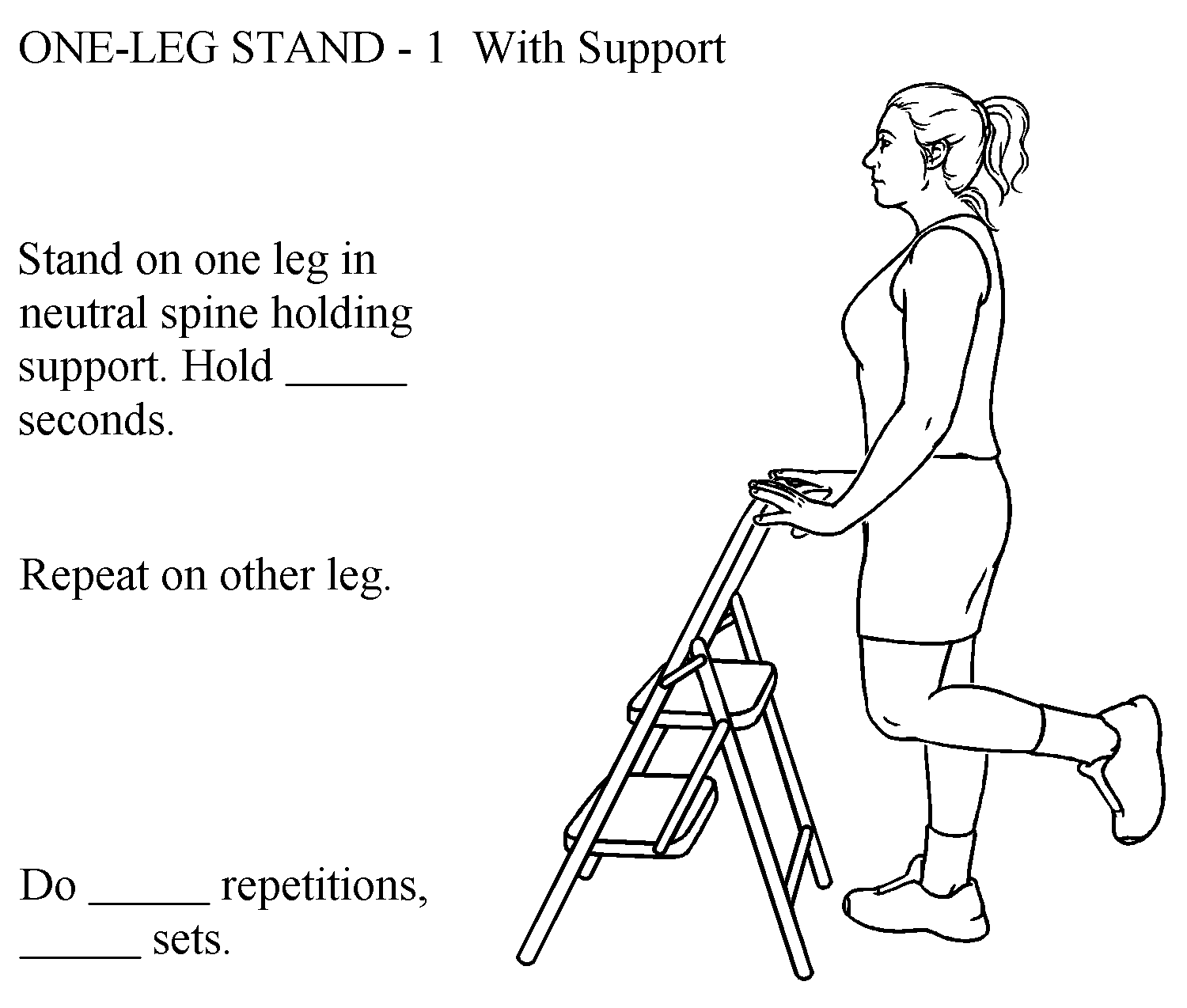
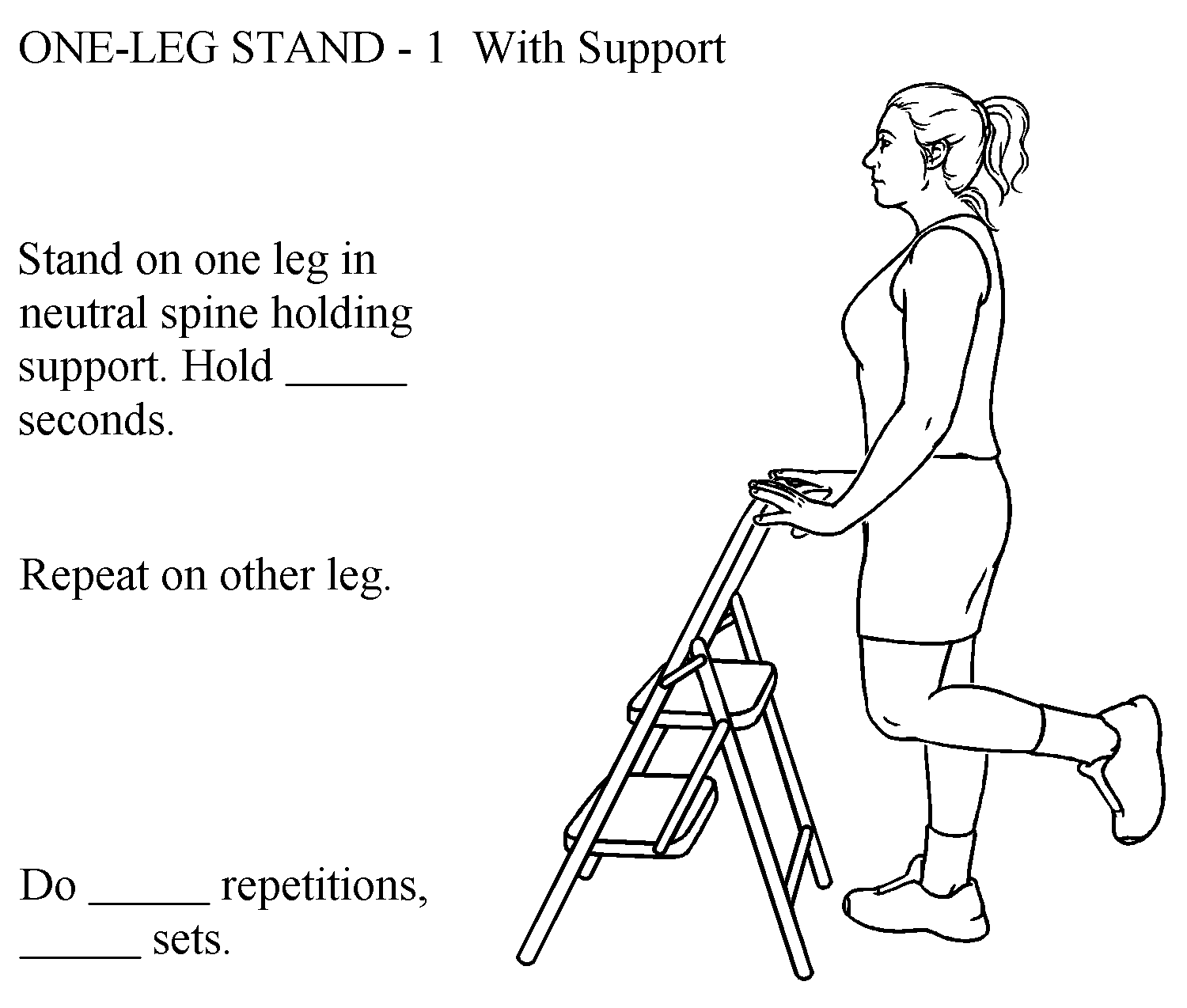
exercises to target stiff and weak muscles should include some firm UE support to minimize risk for falls during unsupervised exercise
balance exercises: standing in a corner for safety or using a chair for support; narrow base of support and progressing to one leg
home assessment: identify areas and objects within the home that may increase risk for falls or repeated trunk flexion motions
Health and Wellness Education
- nutrition and lifestyle education: including dietary sources of calcium, magnesium and Vitamin D
- patients can self-assess fracture risk by using an online tool. Link to 'calculation tool' to select calculations normed by country of residence and race
Exercise Self-Test
Select the images which are most appropriate for strengthening in a patient with osteoporosis
Exam Prep and End of Lesson
- Can you educate a patient on factors which influence bone density?
- Can you recognize clinical indicators for bone loss during a patient screen?
- Can you prioritize exercises based on predictable impairments and risks associated with osteoporosis?