Spinal Orthoses
PTA 104 Orthopedic Dysfunctions Lab
Orthoses as an Intervention for Spine Conditions
Corsets and spinal orthosis can be an integral component of the physical therapy plan of care for spinal pain management. Spinal orthoses can be used during the acute (e.g., following surgery), subacute, and chronic stages of tissue healing and spinal rehabilitation.
Objectives
- Describe the major modes of action of rigid and soft spinal orthoses
- Identify the role of the PTA in patient care involving spinal orthoses
- Identify common braces used to treat scoliosis
- Recognize signs and symptoms of adverse fit of spinal orthoses
- Communicate signs and symptoms of misfit to the supervising PT and appropriate personnel
Primary Goals of Spinal Orthoses
- decrease pain
- by limiting motion
- by providing greater abdominal support
- correct deformities
- by applying pressure to the spine, abdomen, and torso
- prevent motion
- by using materials that are inherently stiff and/or rigid
PTs and PTAs recognize the effects of postural impairments on spinal pain. Optimal lumbar posture can be an important contributor to pain reduction, and orthoses may facilitate maintaining optimal posture.
Evidence-Based Support
A systematic review by Goodwin and colleagues (2016) found that there is relatively weak evidence to support the use of orthotics on WHO-ICF elements, such as impairment reduction and increased participation in patients with a history of vertebral compression fracture.
In a recent comparative study for treating non-specfic low back pain with physical therapy alone or physical therapy & rigid orthotic bracing, there was no signficant difference in pain or postural control between the groups, and some improvements in reported disability in the PT + bracing group (Azadinia et al., 2017a).
Lariviere et al., (2019) compared the effects of active muscle stabilization, LSO use and muscle stabilization + LSO use with controls and found that LSO use had some effect in increasing stiffness (e.g. stability), when compared with active muscle stabilization alone.
Li and colleagues (2015) compared rigid versus soft orthoses as a pain management intervention for older adults in the subacute phase of thoracic vertebral compression fracture and found no signficant difference in pain or function between the two orthotics after 4 weeks of consistent wear. Morrisette and colleagues (2014) compared outcomes in pain and disability between PT + inelastic bracing and PT + elastic bracing in patients with acute, subacute, and chronic low back pain. Their results indicated the inelastic bracing group showed greater improvement in reported disability after two weeks of use.
Patients, some providers, and members of the public may have questions or concerns about bracing and its effect on reducing muscle strength. In a recent review of the literature for lumbar bracing, there is inconclusive evidence that bracing leads to weaknened lumbar musculature (Azadinia, et al., 2017b). Continous monitoring of a need for bracing, measures, and goals should inform decisions to trial and/or continue bracing as an intervention for symptom management and improved function
Azadinia, F., Ebrahimi-Takamjani, I., Kamyab, M., Parnianpour, M., & Asgari, M. (2017a). Comparing lumbosacral orthosis to routine physical therapy on postural stability in patients with chronic low back pain: A randomized trial. Medical Journal of The Islamic Republic of Iran (MJIRI), 31(1), 150-157.
Azadinia, F., Ebrahimi, E., Kamyab, M., Parnianpour, M., Cholewicki, J., & Maroufi, N. (2017b). Can lumbosacral orthoses cause trunk muscle weakness? A systematic review of literature. The Spine Journal, 17(4), 589-602.
Goodwin, V. A., Hall, A. J., Rogers, E., & Bethel, A. (2016). Orthotics and taping in the management of vertebral fractures in people with osteoporosis: a systematic review. BMJ open, 6(5), e010657.
Larivier, C, Boucher, J-A., Mecheri, H., Ludvig, D. (2019). Maintaining lumbar spine stability: A study of the specific and combined effects of abdominal activation and lumbosacral orthosis on lumbar intrinsic stiffness. Journal of Orthopaedic & Sports Physical Therapy, 49(4) 262-271.
Li, M., Law, S. W., Cheng, J., Kee, H. M., & Wong, M. S. (2015). A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthetics and Orthotics International, 39(4), 270-276.
Morrisette, D. C., Cholewicki, J., Patenge, W. F., Logan, S., Seif, G., & McGowan, S. (2014). A randomized clinical trial comparing extensible and inextensible lumbosacral orthoses and standard care alone in the management of lower back pain. Spine, 39(21), 1733.
Orthoses Type and Action
Rigid orthoses may also be referred to as "inextensible"; soft orthoses may also be referred to as "extensible". For your exam, you will be expected to recall the primary action of selected orthoses and make clinical decisions about patient safety and signs and symptosm of orthosis misfit.
|
Acronym
|
Name
|
Primary Action
|
|
SIO
|
Sacroiliac orthosis
|
Limit motion at bilateral SI joints
|
|
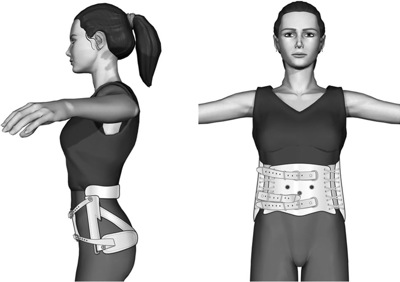
LSO
|
Lumbosacral orthosis
Knight LSO may be indicated for discogenic-mechanical pain

Williams LSO for may be indicated to reduce signs and symptoms of stenosis or spondylolisthesis
|
Limits flexion at lumbar and lumbosacral spine
Soft strap across abdomen allows flexion, rigid posterior and lateral stays limit extension, sidebending,
and rotation
|
|
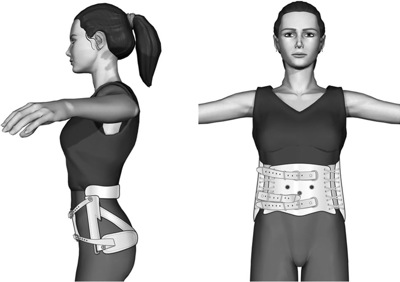
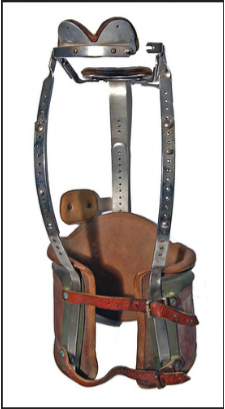
TLSO
|
Thoracolumbosacral orthosis
Milwaukie Brace

https://plus.google.com/photos/113387096966549877335/albums/5692059375073503729/5692059645093835778?banner=pwa&pid=5692059645093835778&oid=113387096966549877335
|
Corrective for scoliosis; limits thoracic and lumbar flexion and extension; lateral straps are adjusted to stabilize against sidebending according to type of scoliosis
|
|
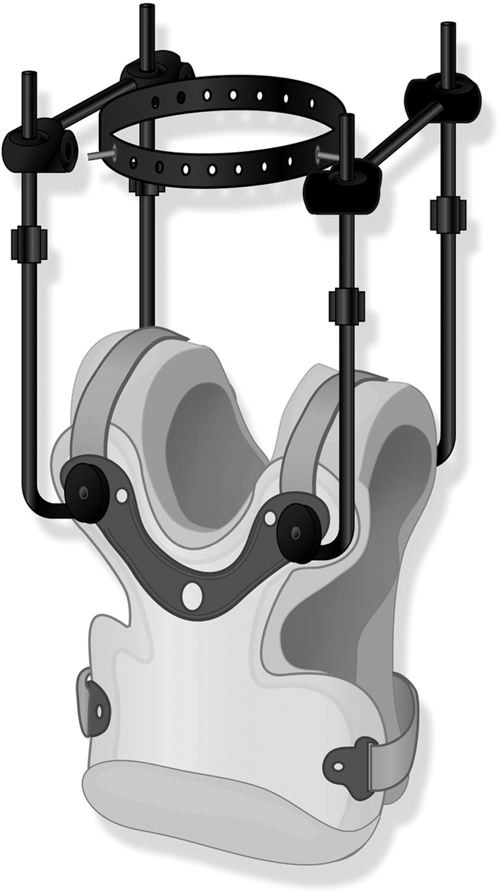
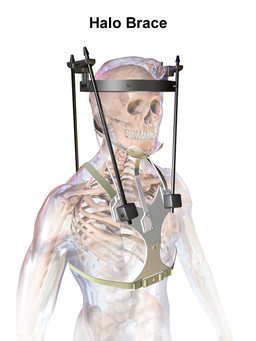
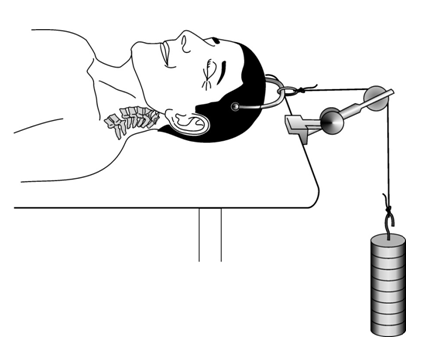
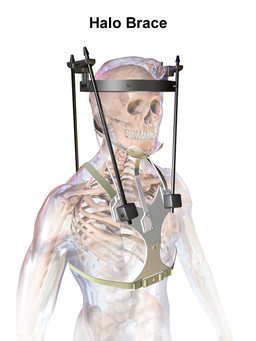
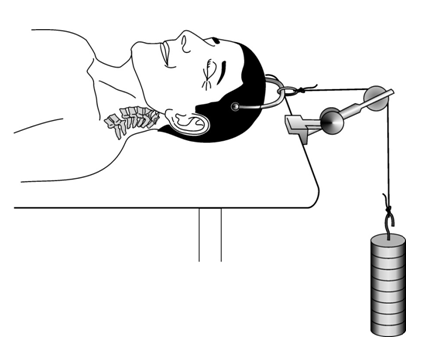
Halo Vest Orthosis
|
BruceBlaus / CC BY-SA (https://creativecommons.org/licenses/by-sa/4.0);
http://www0.sun.ac.za/ortho/webct-ortho/general/trac/trac-3.html
|
Protective post-cervical facture with instability; limits cranial and cervical motion in all planes
Allows a superior traction force to be placed on the cervical spine to facilitate bone healing and reduce facet dislocations
|
|
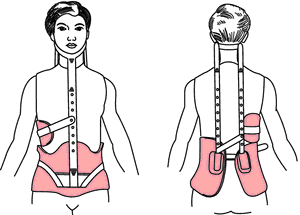
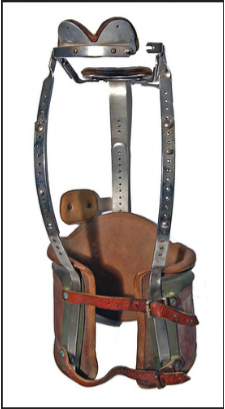
CTLSO
|
Cervico-thoracolumbosacral orthosis
http://img.tfd.com/mk/B/X2604-B-29.png
|
Corrective for scoliosis; limits cervical, thoracic and lumbar flexion and extension; lateral straps are adjusted to stabilize against sidebending according to type of scoliosis
|
|
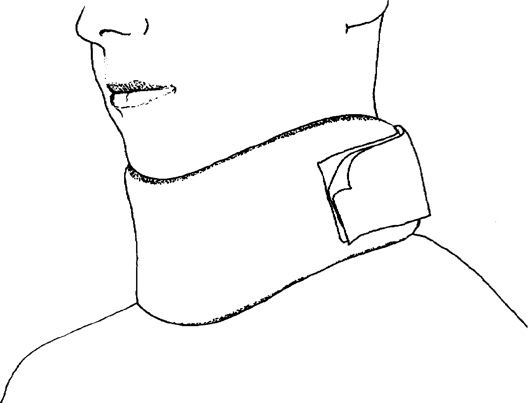
CTO
|
Cervical thoracic orthosis / Rigid Cervical Collar;
Trade names include: Philadelphia Collar; Aspen Collar
|
Limits all cervical motion; commonly applied post-trauma to protect spine and spinal cord; protective orthosis post-whiplash
|
Soft Garments and Supports
|
Acronym
|
Name
|
Primary function
|
Mode of Action
|
|
SI belt
|
Sacroiliac belt

http://activeortho.com/si_belt_for_sacroiliac_pain.html
|
Support SI joint
|
Mild lower abdominal compression
|
|
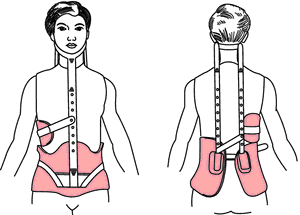
LS Corset
|
Lumbosacral corset

|
Reduce overall gross trunk motion
|
Compresses abdominal tissue; decreasing axial vertebral load; reduce spinal muscle activity
|
|
DL corset
|
DL corset (also known as thoracolumbar

|
Reduce overall gross trunk motion
|
Compresses abdominal tissue; decreasing axial vertebral load; reduce spinal muscle activity
|
|
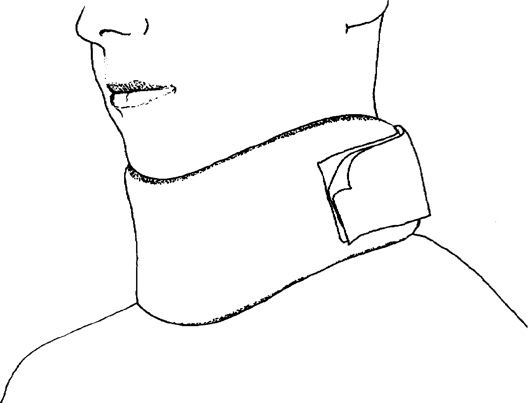
Soft collar
|
Nonreinforced cervical collars made from foam
or any low modulus material
|
Reduce overall gross cervical motion
|
Compresses cervical soft tissue; decreasing axial vertebral load; reduce spinal muscle activity
|
Impairment-Based Classification Considerations
Spine classification may guide recommendations for bracing. A wide variety of orthotic designs, ranging from lumbosacral corsets to rigid thermoplastic thoracolumbosacral orthoses (TLSOs), may be prescribed to appropriate position the spine for protection and pain relief. For example:
Orthoses by Impairment Classification
|
Condition
|
Orthoses type
|
Orthosis position
|
|
Non-specific mechanical low back pain
|
LSO
|
typically positions lumbar spine in extension
promotes lordosis
|
|
Discogenic
Extension-bias
|
TLSO
LSO
Knight LSO
|
typically oriented toward lumbar spine in extension
promotes lordosis
|
|
Stenosis
Spondylolisthesis
Flexion-bias
Non-weightbearing bias
|
LSO
Williams LSO
|
typically oriented toward lumbar spine in flexion
|
|
Fracture
Instability (traumatic and non-traumatic)
|
Halo
CTLSO
Rigid external collar
|
immobilizes specific levels and specific planes of movement.
|
Note: Although the trade name type (e.g., Williams) is typically associated with a position, the role of the PTA is to understand that the position of bias is a position of ease, and to coordinate brace selection and use based on the desired outcome and within the plan of care.
Practical Applications
Active Learning Exercise
For your exam, you will be asked to identify how the structural components in selected orthotics reduce risk for reinjury and affect spine motion. Careful observation of orthoses components can often indicate which structures are receiving the greatest amount of stabilization. For example, by looking at this image, you should be able to classify it (rigid vs. soft, general level(s) of spine affected by bracing): 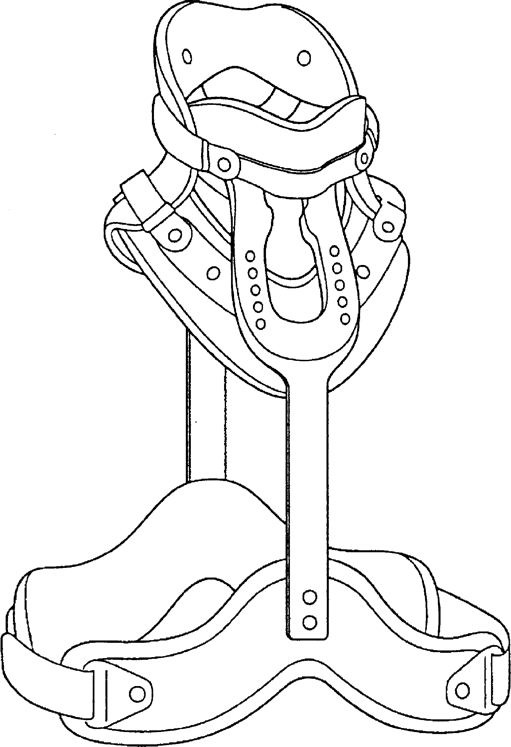
Take a look at this CTO and write down the points of contact for the rigid structures: 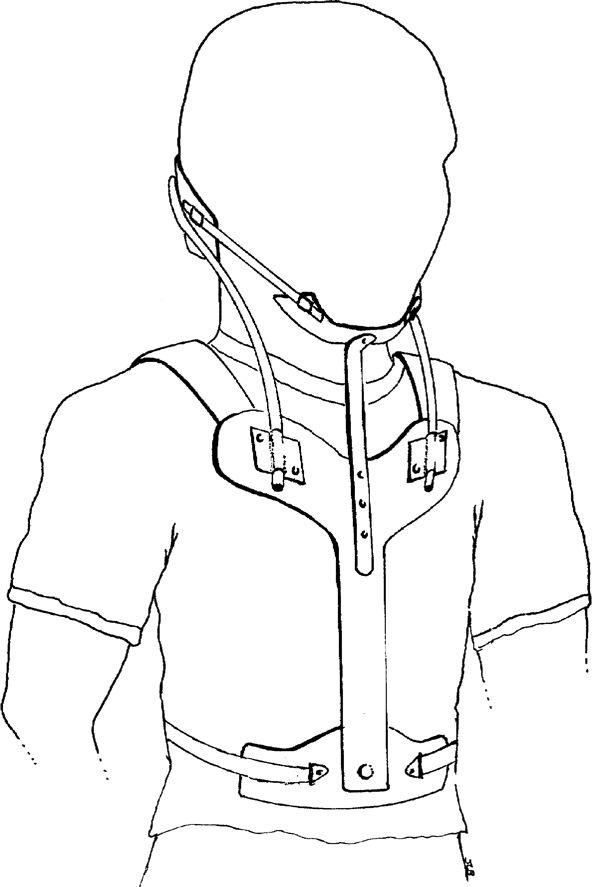 Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?
Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?
Halo Jackets
A halo vest/jacket is the only orthosis which completely limits cervical motion in all three planes. It can be used conservatively or post-operatively to insure adequate healing time for cervical stabilization.
Wear time for a halo jacket is typically 12 weeks, depending on bone healing. Driving while wearing a halo is illegal.
The head is stabilized by pressure pins inserted 1/8" into the skull above the lateral 1/3rd of the eyebrow and just posterior to the ear. Halo jackets typically weigh 5-8 poiunds.
Pins may also loosen over time, shifting out of the skull or into dural tissue, so close monitoring for fit and excessive motion is important.
PT/PTAs are involved in inspecting pin sites for signs and symptoms of infection and reporting findings to appropriate medical personnel and teaching log roll technique for transfers out of bed. . 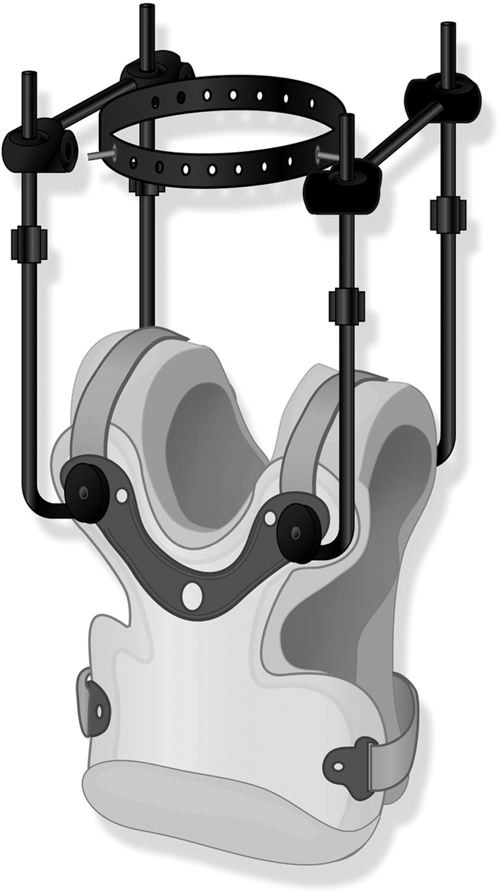
NEVER PULL ON THE HALO JACKET OR USE IT AS A POINT OF MANUAL CONTACT DURING FUNCTIONAL MOBILITY TRAINING. The anterior component of the jacket can be removed in supine for hygiene and for emergency medical procedures.
Scoliosis
Custom molded or 4 point rigid orthoses may be used to prevent progression of scoliosis. Research supports regular checking of fit and tension in the orthotic straps in order to prevent and/or reduce scoliosis progression (Wong, et al., 2000)
In a five year longitudinal study of 158 adults diagnosed with scoliosis, 80% saw increased spinal stability and improvements in curve measurements as a result of bracing (de Mauroy et al., 2016). In a systematic review of the literature, there is stronger evidence that bracing minimizes and slows scoliosis progression (Dunn et al., 2018).
Effective wear time ranges from 18-23 hours/day. In some cases where compliance is an issue, effects can be acheived through a night time wear schedule.
Your text provides examples of orthoses used in scoliosis management.
This six-minute video provides a patient perspective on using a brace for scoliosis management
de Mauroy, J. C., Lecante, C., Barral, F., & Pourret, S. (2016). Prospective study of 158 adult scoliosis treated by a bivalve polyethylene overlapping brace and reviewed at least 5 years after brace fitting. Scoliosis and spinal disorders, 11(2), 28.
Dunn, J., Henrikson, N. B., Morrison, C. C., Blasi, P. R., Nguyen, M., & Lin, J. S. (2018). Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US Preventive Services Task Force. JAMA, 319(2), 173-187.
Wong, M. S., Mak, A. F. T., Luk, K. D. K., Evans, J. H., & Brown, B. (2000). Effectiveness and biomechanics of spinal orthoses in the treatment of adolescent idiopathic scoliosis (AIS). Prosthetics and orthotics international, 24(2), 148-162.
More Clinical Considerations
For your exam, you will be asked to make clinical-decisions based on case simulations with a patient who is prescribed a spine orthoses as part of their rehabilitation.
Coordinate care with the interprofessional team. Work closely with the PT and the CPO (Certified Prosthetist Orthotist) for the latest products which are supported by research. There are many off-the-shelf brands and claims for support. Be sure that you use resources in your community and facility to help coordinate care when it comes to appropriate bracing and bracing modification.
Check fit and reinforce patient education on brace purpose and proper fit. Collars and orthoses are hot, awkward, and limit peripheral vision. Patients, family members and health care personnel are often compelled to loosen collars to increase comfort. If a collar or orthoses is loosened more than when the patient was originally fitted for the device, the effect of the collar is eliminated. The spine will move. PTAs are an integral member of the health care team who educate the patient on importance of proper, snug fit of spinal orthoses when upright. Tissue shifts with weight bearing. Retightening of the orthosis is necessary before the person wearing the orthosis changes from a supine position into sitting or standing postures.
Observe and inspect for signs and symptoms of skin or pressure injury. Pressure from weight bearing or from lying on the orthosis can lead to skin breakdown. Check for capillary refill or excessive blanching when the orthosis is removed. Stage 1 pressure areas should be reported to medical personnel and the PT in order to schedule brace and positioning modifications as needed. Check to be sure the patient is wearing an approved stockinette or undershirt when using a CTO or CTLO. Stockinettes absorb moisture and provide a modest friction barrier between skin and rigid components/straps
Apply principles of therapeutic positioning to optimize movement and prevent injury. Optimally, only a single pillow placed under the upper back (scapula), neck, and head is used for sleeping. When several pillows are placed under the person's head and neck, a large flexion moment is created, which, in turn, creates areas of high-pressure contact with the skin, increasing discomfort and the risk of skin breakdown.
Acknowledge the contextual factors that interfere with adherence and take time to educate. The aesthetics of bracing can often lead to non-compliance with wear time. Patients can perceive donning a brace to get to the restroom a nuisance-level task. Adolescents and teens are more likely to avoid wearing spinal orthoses. Frequent patient education on the risks of increasing instability and further injury/disability is often necessary in order to solidify understanding reasons for non-use.
Allow for questions about personal matters, such as hygiene and sexual activity. Sexual activity is often signficantly inhibited in patients who need spinal bracing. Patients may consult PTs and PTAs about how to assume sexual positions while minimizing risks for further injury. Rolled towels under the lumbar spine, kneeling positions and supported sidelying positions are several options to minimize spinal motion and sustained spinal position. Sex and Back Pain by Lauren Hebert, PT, OCS is an excellent resource for patients and PT/PTAs, complete with illustrations and positioning recommendations. There is an ebook version available for a very low cost.
End of Lesson





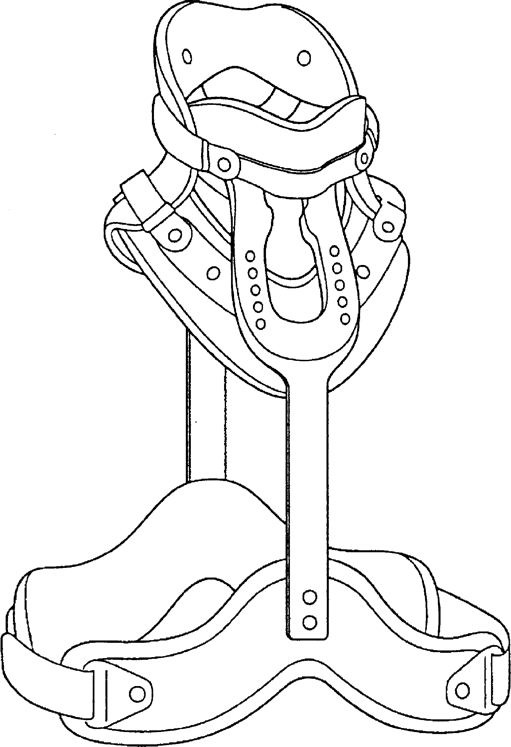
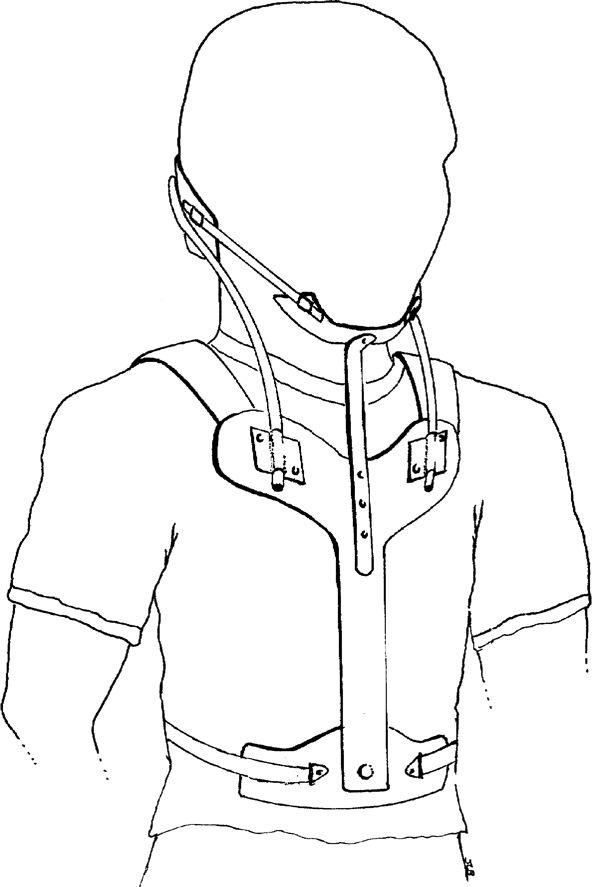 Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?
Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?