Week 1 - Foundations for Effective Therex
PTA 104 Orthopedic Dysfunctions
Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions.
Introduction
Now you get to apply your knowledge of kinesiology and therapeutic exercise while expanding your understanding of pathologies, impairments, functional limitations and disabilities affecting the musculoskeletal system. Before we move directly into movement-based rehabilitation, we need to revisit normal muscle and skeletal anatomy and physiology, principles of motor learning, and postural alignment.
Lesson Objectives
- Review structure and function of the musculoskeletal system
- Recall principles of progressive:
- strengthening
- stretching
- ROM
- Review common pathologies associated with imbalances in strength and flexibility
- muscle strain
- abnormal posture
- Identify principles of motor learning and training
- Relate therapeutic exercise principles to the role of the PTA.
Introduction Video From Christina - Approximately 4.5 minutes
Musculoskeletal Anatomy Key Term Review
|
Key Term
|
Definition
|
|
myofiber
|
single muscle cell
|
|
myofibril
|
myofiber contractile units
|
|
sarcomere
|
a single contractile unit
|
|
motor unit
|
one neuron and the muscle fibers it innervates
|
|
Type I
|
Slow-twitch; dominant fiber type for endurance/posture;
|
|
Type II
|
Fast-twitch; dominant fiber type for agility, quick actions
|
|
neutralizers
|
muscles that function to maintain motion within a target plane of motion
|
|
stabilizers
|
muscles that function to provide support a region while another area moves
|
|
fascia
|
loose, ubiquitous connective tissue
|
|
tendon
|
thick connective tissue that attaches muscle to bone. Myotendinous junction (where muscle connects to tendon) is the most common site of muscle strain
|
|
ligaments
|
thick connective tissue that connects bones across joints; contributes to proprioception and pain perception
|
|
articular cartilage
|
avascular viscoelastic material that provide a smooth frictionless surface for joint motion
|
|
fibrocartilage
|
blend of fibrous and cartilaginous tissue that provides flexibility, toughness, and elasticity
|
- Major contractile proteins in myofibrils are actin and myosin
- Concentric muscle contraction (shortening) relies on ATP as its energy source to catalyze the myosin head bond to actin filaments.
- Eccentric contraction involves the physical "breaking" of cross links between actin and myosin due to an applied load.
- Hundreds of thousands of myofibrils use energy and interactions between actin and myosin to produce a shortening contraction resulting in isometric, single joint, or functional movement.
- Muscle function and training will determine the efficiency and effectiveness of Type I and Type II fibers.
Strengthening Benefits
- Increase speed, efficiency, and precision of movement
- Increase stability
- Increase endurance
- Increase size of muscle to meet demand
- Improve circulation
- Support and improve cardiovascular health
- Improve posture - increase bone density
- Reduce risk for overuse injury
Muscle Strengthening Methods
|
Neuromuscular electrical stimulation
|
Primarily used for muscle reeducation; timing of contraction
|
|
Isometric
|
Slow tension build with sustained hold, followed by a slow release. "Rule of tens" - 2 second ramp up, 6 second hold, 2 second release; used when joint motion is contraindicated to prevent atrophy or loss of tensile strength from disuse and promote circulation
Progression: single angle submaximal, multiple angle submaximal, and multiple angle maximal
|
|
Concentric/isotonic
|
Muscle shortening producing enough force to produce joint motion
|
|
Eccentric
|
Deceleration, controlled lowering against gravity; stimulates contractile and non-contractile elements
|
|
Isokinetic
|
Requires exercise equipment that maintains torque throughout the range of motion
|
|
Proprioceptive neuromuscular facilitation
|
Manual resistance applied to promote stability or motion depending on the target outcome
|
|
Stabilization
|
Goal is to focus maintaining a closed-chain position in varying levels of support
|
Muscle Tissue Pathology
Disuse Atrophy
- The number of sarcomeres decrease with disuse
- The size of muscle cells decrease with disuse
- Connective tissue (non-contractile) loses its tensile strength with disuse
- Muscle tissue becomes stiffer (i.e., loses elasticity) with disuse
- Disuse can be result from acute injury, immobilization, primary disease, a secondary effect from disease, and/or a lifestyle choice
- Fast twitch muscle fibers (Type II) atrophy faster than slow twitch (Type I)
Muscle Strain
- Classifications range from overstretch to tissue failure (tear)
- Most common site of strain is where the muscle and tendon connect ("musculotendinous")
- May result when there is
- repetitive overuse
- sudden excessive loading beyond a muscle's capacity to resist the force
- overstretching
- Graded on a three-point scale: higher grade = more severe injury
Review from PTA 101
Stretching versus ROM
Range of Motion (ROM)
- Range of motion describes specific (joint) or gross (limb and trunk) movement.
- ROM can load and stress soft tissues
- ROM may be selected as a therapeutic exercise in order to:
- decrease pain
- prevent contracture
- promote circulation
- maintain and promote elasticity
- Early healing ROM follows a predictable sequence: PROM, then AAROM, then AROM
- The type for ROM exercise (PROM, AAROM, AROM) is largely based on tissue healing stages and any subsequent post-operative precautions
Stretching
- Stretching includes applying a force over time in the end range of the tissue to create lasting changes in soft tissue length
- Stretching is most effective when the soft tissues are heated to promote extensibility
- Stretching may be selected as a therapeutic exercise in order to:
- increase ROM
- reduce posture impairment
- decrease pain
- increased strength
- reduce functional mobility impairment
- Techniques can be passive (i.e., static stretch) or active (i.e., hold-relax, contract-relax)
- General descriptions include static, cyclic, ballistic, and PNF stretch
- Stretch durations between 15 seconds and 2 minutes can produce changes in muscle length
- A minimum of frequency of 2 x week over 6 weeks is needed to produce lasting changes in muscle length
Stretching is not the same as applying PROM nor progressing to AAROM and AROM
- Muscle is comprised of contractile and noncontractile elements (i.e., soft tissue)
- Stretching - elongation of soft tissue
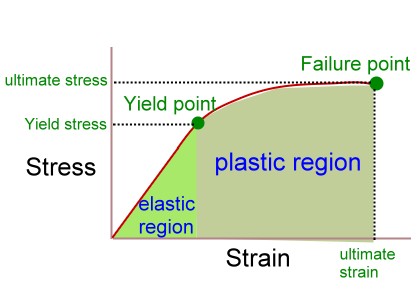
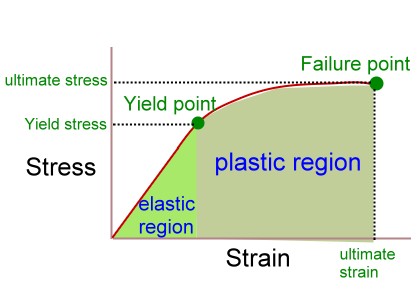
- Stress-Strain curve illustrates how the effect of a sustained load on soft tissue over time results in a lasting change in the length of the connective tissue
- Stress = load or force causing the strain; strain = elongation of the tissue as a % of its original length
- Creep describes how soft tissue will become increasingly stretched over time when the load on the soft tissue is constant
- Relaxation describes how the soft tissue length decreases when the load is removed.
- Yield point - when the soft tissue will no longer return to it's original resting length
- Viscoelasticity of soft tissue is represented by the strength-strain curve; repetitive stretching allows for the soft tissue to experience greater strain (length) under the same stress (load)
- movement in the elastic range will result in no change to muscle length - the tissue "bounces" back
- stretching occurs in the plastic range and will result in soft tissue lengthening by "breaking" collagen fibers; energy from breaking collagen is released as heat
- longer strain durations are indicated for older patients due to changes (e.g., decreased) plasticity of soft tissue
- overstretching can result in tissue failure, tearing, strain and/or rupture (failure point)
- http://www.pt.ntu.edu.tw/hmchai/bm02/bm02method/ForceMeasure.files/StressStrain.jpg
Static stretch is the safest form of stretching. A constant load applied over time will allow the soft tissue to safely yield, target collagen fibers which restrict motion, yet protect from strain and/or tear.
PNF stretching is the most effective method to increase muscle length over time.
What is Therapeutic Exercise?
Therapeutic exercise is the systematic, planned performance of bodily movements, postures, or physical activities intended to provide a patient/client with the means to
- Remediate or prevent impairments
- Improve, restore, or enhance physical function
- Prevent or reduce health-related risk factors
- Optimize overall health status, fitness, or sense of well-being
Therapeutic exercise is used in physical therapy to prevent disability, to minimize the progression of factors which result in disabilities, and to provide rehabilitation from pathological processes which result in loss of function and participation in the community. The PT/PTA team consider risk factors which may impact successful progression through a plan of care. Biological, lifestyle, environmental, and socioeconomic factors which impact treatment planning and progression are an integral part of PT/PTA -patient- centered approach to treatment.
How does therapeutic exercise prescription support a need for skilled physical therapy services?
- Therapeutic exercise effects on body tissues and systems are monitored for safety and effectiveness through objective means
- Therapeutic exercise is selected based on a sound foundation in anatomy, physiology, kinesiology, pathology, and behavioral/social sciences
- Therapeutic exercise is individualized to positively impact impairments, functional limitations, and disability for the patient/client
- Therapeutic exercise includes principles of motor learning to optimize skill and performance of movement-based activities
- Therapeutic exercise is specific to the targeted functional outcome for the patient
What factors contribute to the safety of a therapeutic exercise program?
- Health history
- Current health status (includes CP, Integument, Musculoskeletal, Neuromuscular)
- Exercise environment (equipment and surroundings)
- Accuracy of performance; includes monitoring for substitutions
- Fatigue/Endurance
- Proper body mechanics and joint protection habits by the treating therapist
Key Terms in Therapeutic Exercise
|
Term
|
Definition
|
|
Flexibility
|
range of motion allowed at a joint
static - PROM at a joint
dynamic - ease of movement within the ROM
|
|
Strength
|
maximum force produced in a single contraction
|
|
Endurance
|
sustained contractions or effort over time
|
|
Power
|
a function of speed and strength within a muscle
|
|
Intensity
|
level of effort
|
|
Duration
|
length of time (session or over a rehabilitation/exercise program)
|
|
Frequency
|
Number of times exercise is performed (session, rehabilitation plan)
|
|
Position
|
Alignment of limb or body (e.g., related to gravity, end-range, etc.)
|
|
Progression
|
Increasing demand of exercise to effect a change in one or more outcomes (e.g., speed, accuracy, complexity, endurance, power, etc.)
|
|
SAID
|
"specific adaptation to imposed demand" - selected exercises should match intended effect
|
|
Overload
|
adaptation and training requires a demand greater than normal stress
|
Types of Resistance
|
Gravity
|
Moving against gravity (concentric); and slow lowering with gravity (eccentric); effective for weakened muscles
|
|
Body weight
|
Leverages body weight as resistance (e.g. push up, squat, side plank)
|
|
Small weights
|
Cuff weights or free weights allow for high repetition motions to build endurance and strengthen weaker muscles
|
|
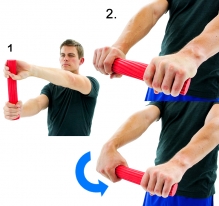
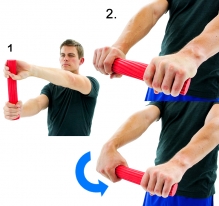
Surgical tubing/theraband
|
Variable resistance to motion dependent on the elastic qualities of the tubing
|
|
Machines
|
Typically used for larger muscle groups to build strength/power
|
|
Manual resistance
|
Clinician uses hand placement during motions or positions to resist through parts of an arc or throughout the arc of motion
|
Strengthening Programs
Therapeutic exercise selection dependent on the patient goals, tissue healing stage, general conditioning, and pain response. Typical resisted exercise progression gradually increases the load on contractile and non-contractile tissue to optimize function
- small arc submaximal contractions: concentric/eccentric

- full range of motion: concentric/eccentric (e.g., bicep curl with hand weight)
- functional activity specific plane submaximal concentric (e.g. sidestep with elastic band)

- functional ROM submaximal eccentric
Free Exercise Resource
Would you like to have access to modifiable home exercise pictures and instructions? Try HEP2Go.com! Create an account and design your own home exercise programs and reinforce your understanding of muscle action and function at the same time.
I use this in the clinic and its just great. Don't forget, you have access to home exercises through your APTA membership: Go to PTNow and the Rehab Reference Center to find the exercises that align wiith the PT plan of care.
Motor Learning Principles
In many of our case simulations, we have provided patient and family education in exercise techniques and safety considerations. How do we optimize our patient/client's chances for mastering the task? How do we evaluate if our instruction led to the intended result? With adequate preparation and applying concepts of motor learning, we can evaluate our effectiveness as patient and family educators.
Suggestions for exercise instruction
- inquire about patients goals and general understanding of therapeutic exercise in rehabilitation
- Assess for patient fears and/or concerns regarding exercise and exercise programming
- choose an environment which is free of distractions
- demonstrate correct and variant forms of movement to create a context for correct technique and common errors
- use multiple modalities (verbal, visual, demonstration/kinesthetic) to optimize skill acquisition for all learners
- evaluate patient performance by repeat demonstration under supervision
- provide specific feedback to optimize the patient/client's ability to self-assess future performance
- design instruction which allows for mastery of simple to more complex tasks.
Taxonomy of Motor Learning
Taxonomies are classification systems to categorize items, animal, activities, etc., using progressively specific terminology. In motor learning, taxonomies are used to help distinguish levels of complexity between movement-based activities.
Environmental factors
Closed environments are less complex than open environments. Closed environments are static: objects, people and surfaces do not move. Open environments are dynamic: objects, people and surfaces can move and change between episodes.
Intertrial Variability: is absent when there is no change to the environmental conditions; is present when environmental demands change with each attempt
Desired Outcome of the Action
Body stable actions are less complex than body transport actions. Body stable includes maintaining a stationary/stable position while executing a motor task. Body transport includes activities where the patient/client is moving and changing positions through space
Tasks which do not include object manipulation are less complex than tasks where the person is required to move/manipulate an object
Practice and feedback strategies are selected by the PT/PTA based on the instructional readiness of the patient/client and the complexity of the task demands (person/environment). Your text distinguishes between:
- part vs. whole practice
- blocked practice
- random practice
- random-blocked practice
- physical practice
- mental practice
Consider the intended outcome of the instruction. Performance is enhance by repeated blocked practice, however, skill retention and transferability of skills to multiple conditions and environments benefits most from task variations. The key is to assess each patient/client and select the most appropriate level of practice to allow for incremental, progressive success in motor performance and skill development.
Feedback is categorized by timing, outcome focus (knowledge of performance vs. knowledge of result), and source.
Test your knowledge of effective instructional strategies for therapeutic exercise by matching the strategy with the most likely stage of motor learning
Active learning exercise
Consider a patient who has right ankle stiffness and weakness since an ankle sprain 8 weeks ago due to volleyball injury. The patient walks with a minimal limp, with decreased stride length on the left.The patient is athletic and is eager to return to sport, however, this is the third time the patient has had this injury.
Can you think of a series of progressions, with a focus on motor learning principles as a guiding factor? How will you change practice, feedback, environment and stability versus mobility to demonstrate you are making the task progressively more complex and automatic? Is it something you would be willing to do on your own if you had this injury?
Post your response in the CAN YOU HELP ME forum
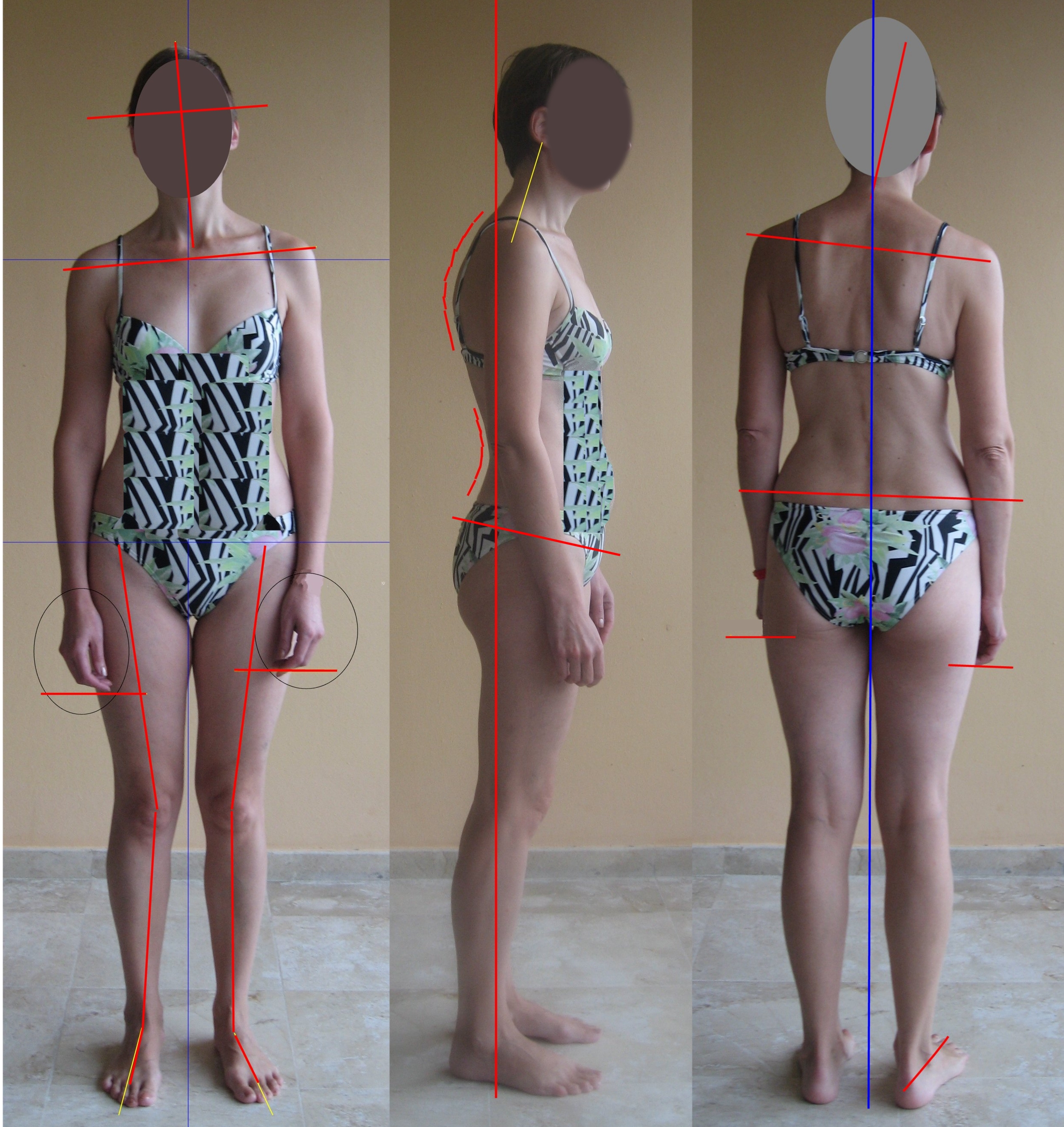
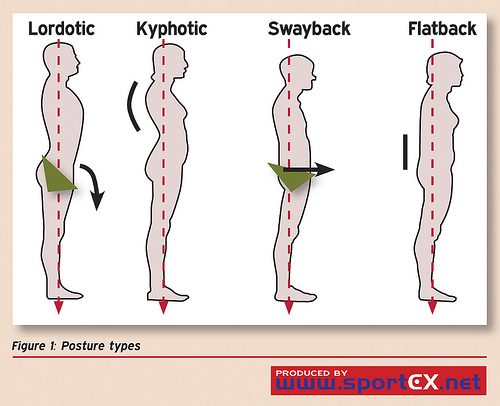
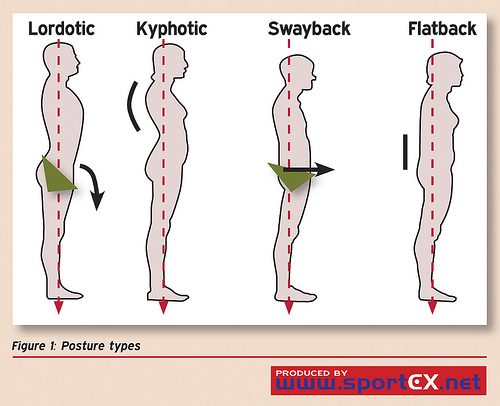
Faulty Posture Review
Common Faulty Postures
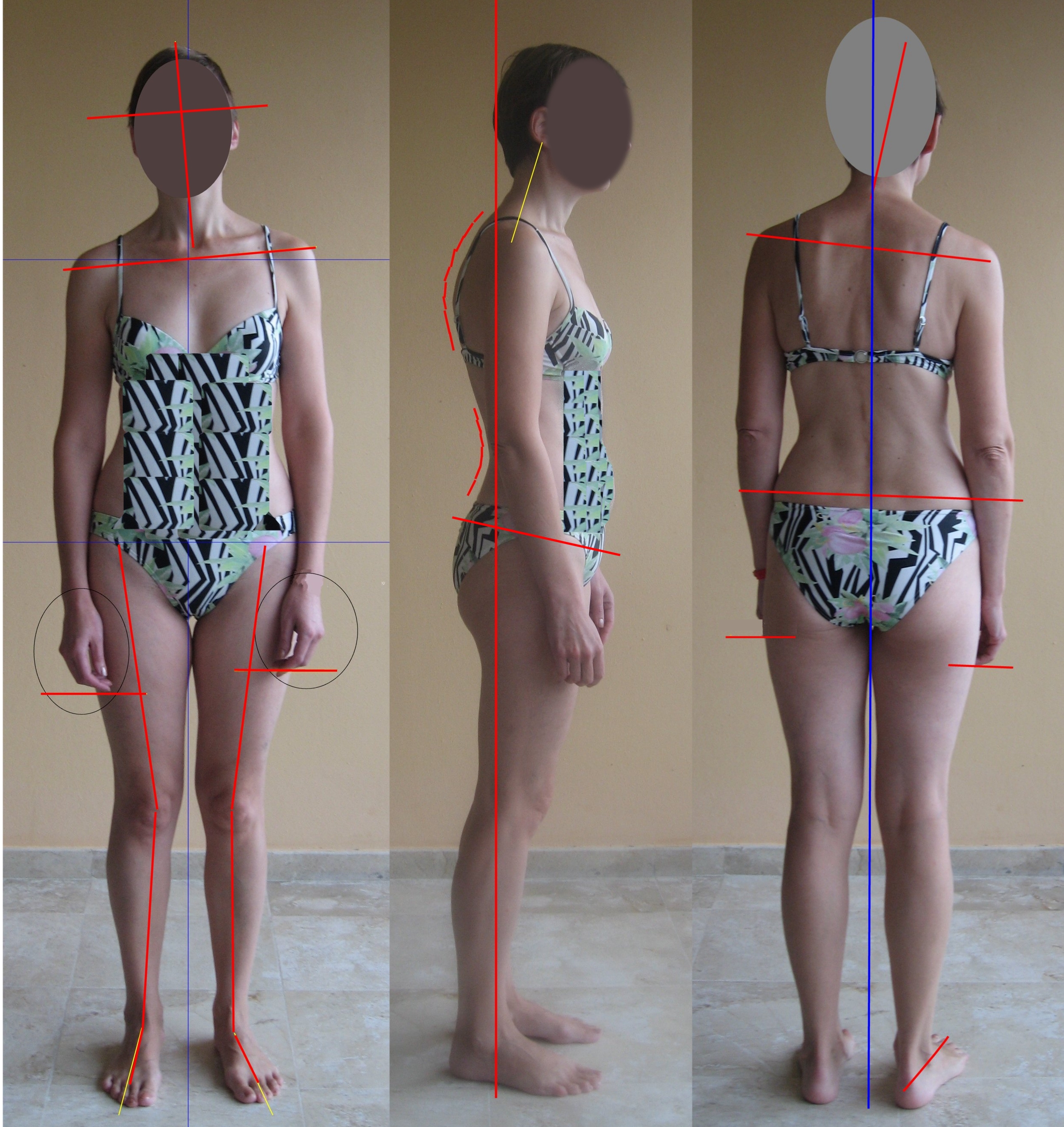
- Lordotic
- Flat back
- Slouched (sway back)
- Forward head
- Kyphotic
- Flat Upper Back
http://www.flickr.com/photos/sportex/5862747046/in/photostream/
Postural impairments are influenced by disease, endurance, strength and flexibility, age, pregnancy, habit, and pain
Muscle length (i.e. too long and too short) influences postural alignment
Role of the PTA
- PTAs use clinical reasoning and critical thinking to select the most appropriate therapeutic exercise. Effective decision-making is based on:
- the plan of care (selected interventions and goals)
- integrating specific direction from the supervising PT
- applying knowledge of precautions and contraindications
- applying knowledge of health status, body systems, related structures and tissue healing properties
- applying knowledge of motor learning principles
- consideration of personal factors (e.g., patient's age, ability to participate, motivation, cognitive status, etc.)
- evaluating the patient response (physiological, observation, behavior)
- consideration of environmental factors (e.g., discharge plan and setting, resources, work/home demands, etc.
- communicating barriers and outcomes to the supervising PT
- PTAs educate patients and clients in the frequency, duration, and methods of therapeutic exercise for injury management and prevention
End of Lecture