Spinal Disorders
PTA 104 Orthopedic Dysfunctions
Spinal Disorders - Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment. Contact howardc@lanecc.edu for permissions.
Introduction
Note: There are approximately 30 minutes of embedded screencasts as part of this interactive lecture. Additional supplemental materal is included as hyperlinks.
4 minute video
In this lesson, students will apply knowledge of anatomy and kinesiology of the spine to specific disorders encountered in physical therapy. The content and instruction assumes students have a working knowledge of the bones, ligaments, nerves, and muscles of the spine. Spinal pain is the number one reason people encounter and use physical therapy. PTAs must have an understanding of normal and abnormal spinal function and degenerative conditions in order to correctly select, apply, and compare results with the physical therapy evaluation and assessment.
Objectives
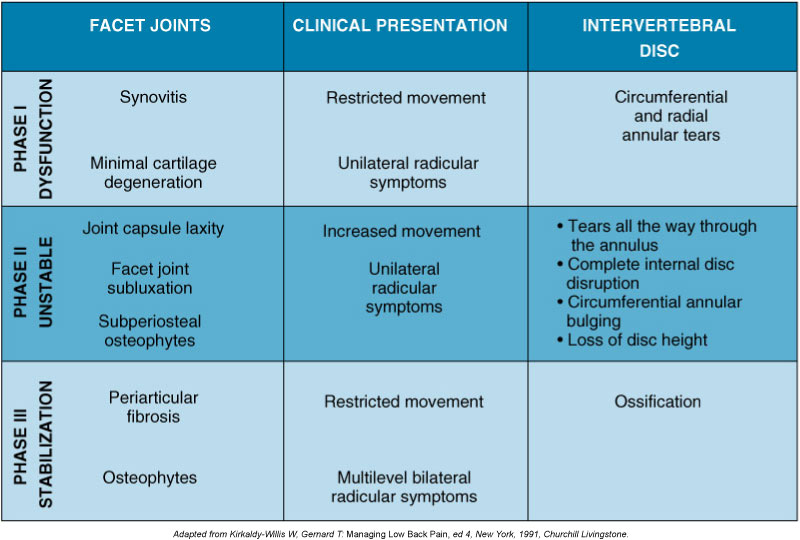
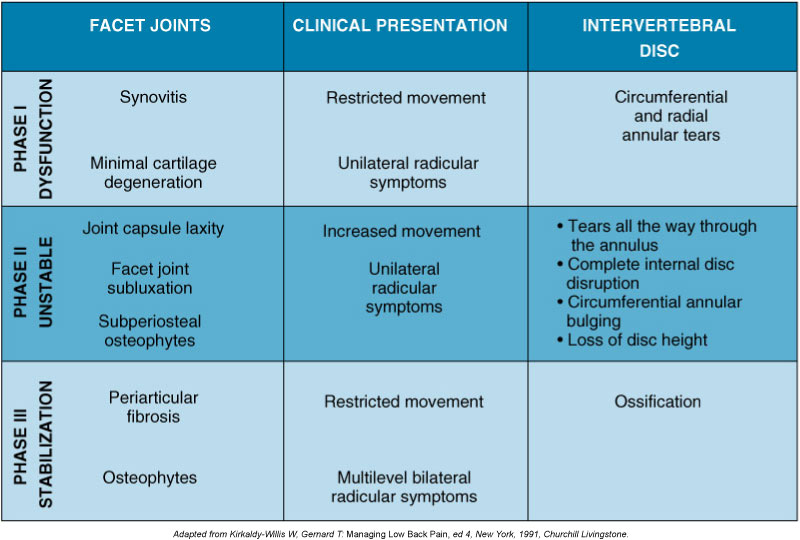
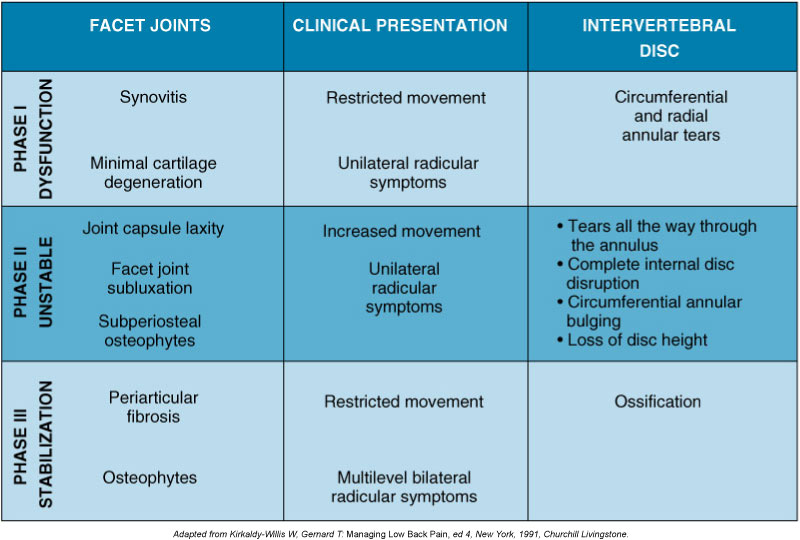
- Describe the phases of spinal joint and disc degeneration
- Describe mechanisms, signs and symptoms of common spinal disorders
- Differentiate between conditions of hypomobility versus instability
- Identify the most commonly involved spinal segments in degenerative disc disease
- Discriminate between clinical scenarios which indicate a surgical or other medical emergency/complication
- Compare and describe common surgical interventions for the spine
- Describe findings of musculoskeletal, neuromuscular, and special tests performed during PT examination of spinal disorders.
- Compare and contrast classification systems for low back and spinal pain
Definition of regional pain
- Low back pain extends inferior to 12th rib to the gluteal fold
- Neck pain is between the occiput and T3
Link to Screencast (About 4 minutes)
Incidence
|
% of adults in U.S. reporting LBP x 1 day / year
|
56%
|
|
% of adults in U.S. reporting LBP x 6+ days / year
|
34%
|
|
% of adults in U.S. reporting LBP >30 days/year
|
14%
|
|
% workforce receiving disability income due to LBP
|
2%
|
|
% pregnant women reporting LBP
|
48-90%
|
|
% of adults who experience recurrence of LBP following a single episode
|
up to 85%
|
According to the National Institute of Health, spine impairment is the most frequent musculoskeletal impairment and low back pain is the most frequent reason for referral to physical therapy.
Phases of Degeneration
Video about 4.5 minutes
Facet joint and intervertebral disc degeneration can be classified in three (3) phases of degeneration, resulting in pain and fluctuating levels of spinal stability
Complete this self-assessment of your ability to recall medical terminology related to the spine.
Spinal Disorders
Radiculopathy
- Spinal nerve / nerve root conduction is impeded due to "encroachment into peripheral nerve tissue spaces resulting in nerve compression or ischemia";
- encroachment can be classified as direct or indirect, mechanical or chemical
- direct - mechanical : direct compression pressures from structures or motions is place on spinal nerve(s)
- indirect - mechanical: blood flow decreases (ischemia) to the spinal nerve from direct pressure (compression or stretch) or from scar tissue formation around nerve tissue
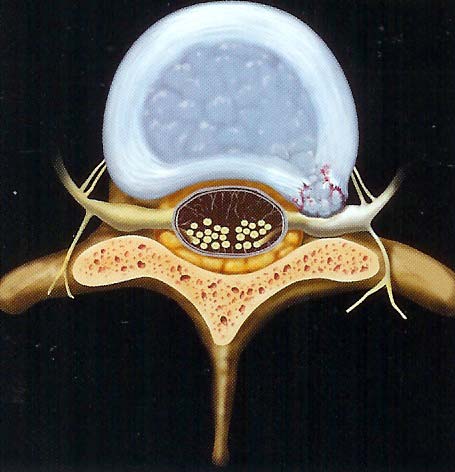
- direct - chemical: nuclear material from herniated intervertebral discs encroaches space
- indirect - chemical: ongoing cellular inflammatory responses with tissue edema
- Compression can be due to stenosis in the central canal or foramen by bony and/soft tissue changes, tumor, or disc bulge/herniation
- Associated Signs and Symptoms: Numbness (sensory n.), weakness (motor n.), muscle atrophy, impaired DTR, sensory changes in affected nerve root distribution
Sciatica
- sharp, radiating pain often associated with numbness and parasthesias
- weakness and loss of reflexes
- L4: patellar reflex, medial sensation
- L5: dorsiflexion, lateral sensation
- S1: Achilles reflex, plantar flexion, posterior sensation
- aggravated by coughing, sneezing, valsalva
- most-commonly caused by herniated disc
- Cauda Equina Syndrome: considered a surgical emergency
- sudden change in bowel/bladder function (urinary retention, loss of sphincter control) or
- sudden loss of sensation in the perineum ("saddle anesthesia")
- bilateral sciatica symptoms
- treatments is typically PT x 6 weeks with follow-up MRI/CT if there is no improvement in symptoms

Intervertebral Disc Disease
- Disc structure allows for distribution of force during weight bearing through the spine
- Reinforce your understanding of spine kinesiology by
- reviewing the animation on the Vertebra and Discs
- you will be taken to a Web page on the Normal Spine and from there you need to click on the Vertebra and Discs link to view the animation
- Disc structure allows for complex spinal motions in multiple planes
- Degenerative changes increase with repetitive compression (e.g. heavy lifting in flexion) or trauma (e.g. fall); degenerative changes may be asymptomatic
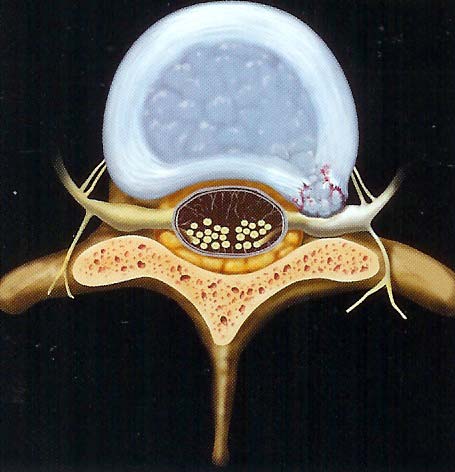
- Annulus fibrosis can tear, resulting in decreased resistance to torque and increased risk of extrusion of disc contents; risk of herniation of nucleus pulposus increases with annular tears
- tears usually occur posteriorly where the annulus is weakest
- Discs may bulge without evidence of annular tearing or herniation
- Most common site of disc herniation is
- foraminal disc herniations are the most symptomatic
Watch this video on lumbar disc herniation to reinforce concepts from your Cameron text
- Nucleus pulposus desiccates, decreasing its ability to absorb and distribute weight bearing and rotational forces; age-related change
- Increased calcification, fracture risk, and decreased density at vertebral end-plates
- The affected nerve root is between spinal levels (e.g. C5-6 involves C5 nerve root)
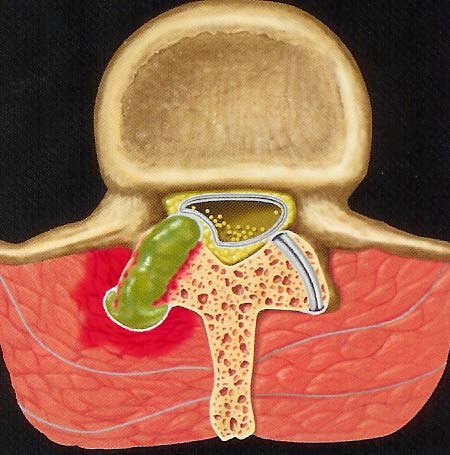
Spinal Stenosis
- Narrowing of the spinal canal or associated spinal foramen due to degeneration such as
- thickening of ligamentum flavum
- facet synovial cysts
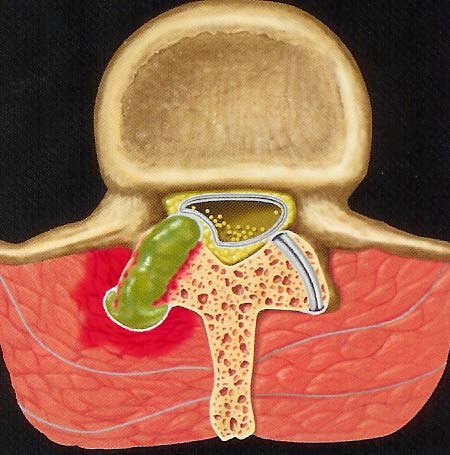
- Stenosis progression can lead to specific motor and sensory deficit patterns:
- central cord syndrome: motor and sensory changes are primarily in the upper extremities
- Brown-Sequard syndrome: ipsilateral weakness, contralateral sensory deficits
Watch this video on spinal stenosis to reinforce concepts from your Cameron text
- Space within the canal/foramen changes with spinal motions:
- flexion --> central canal widens
- extension --> central canal narrows
- What therapeutic exercises will decrease compression to nerves affected by central canal stenosis?
- Signs and symptoms of spinal stenosis
- Cervical ->decreased strength and dexterity in hand, decreased grip function, pain, numbness in hands, potentially impaired balance/gait
- Lumbar -> pain (affected side or bilateral), numbness and LE weakness
- neurogenic claudication = pain in B LEs increasing with prolonged standing/extension and is relieved with lying down or sitting (flexion); increased pain with walking down inclines (due to increased lumbar extension)
- What postural adaptations can you expect from a patient with severe lumbar spinal stenosis?
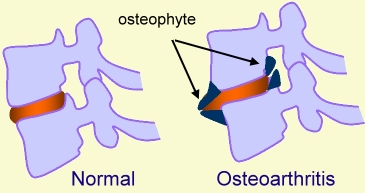
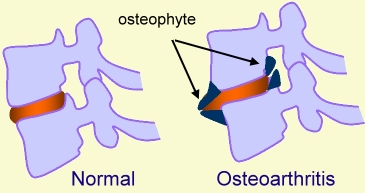
Osteoarthosis
- usually appear at the uncovertebral and/or facet joints
- osteophytes are one of the space-occupying lesions which may lead to radiculopathy
Spondylolysis and Spondylolisthesis
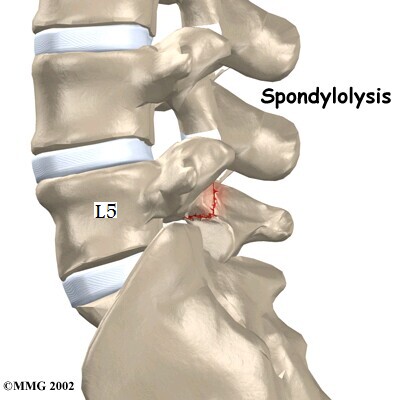
Spondylolysis
Fracture of the pars interarticularis (segment of bone between the superior and inferior articulating facets)
Can occur with some forceful impact in extension (hopping/landing on one foot)
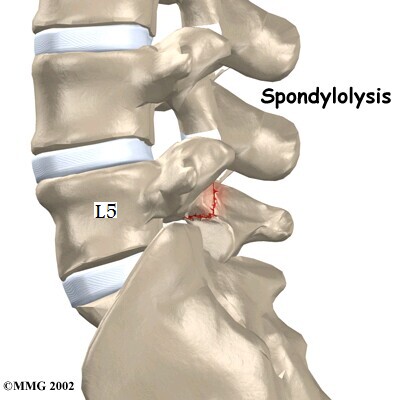
Result is instability at the affected segment and abnormal weight-bearing forces in adjacent spinal segments
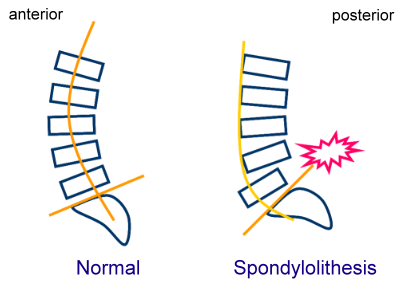
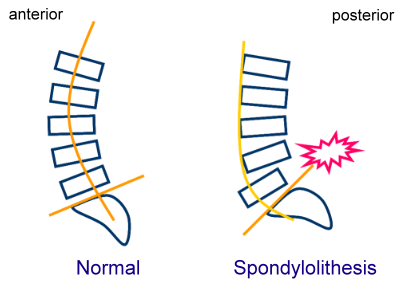
Vertebra translates forward in the sagittal plane with respect to adjacent vertebra
Spondylolisthesis
Mostly a condition of the lumbar spine which is associated with chronic, repetitive trauma
Mostly involves and anterolisthesis of the affected segment
May require surgical intervention/posterior fusion to prevent further instability or loss of nerve function
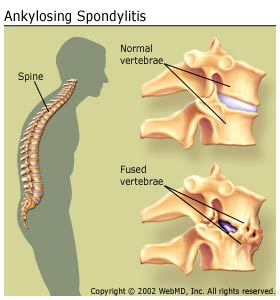
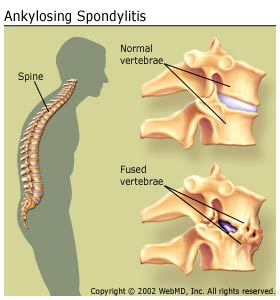
Ankylosing Spondylitis
An inflammatory condition of unknown etiology which initiates as inflammation in the sacral region. It results in progressive loss of spinal motion due to progressive inflammation and vertebral fusion.
Whiplash-Associated Disorders (WAD)
Refers to bony and/or soft tissue injury in the cervical spine and upper quarter due to acceleration-deceleration forces
Injury is to ligaments and muscles; stretch forces to neuromuscular structures may account for increase sensitization
Symptoms of WAD include:
- pain
- headache
- decreased spinal mobility
- stiffness
- low back pain
- shoulder pain
- visual disturbances
- dizziness
Classification of WAD
- Grade I: No physical signs of musculoskeletal dysfunction; subjective reports of pain, stiffness, and tenderness
- Grade II: Some physical signs of cervical movement dysfunction; subjective symptoms reported
- Grade III: Physical and neurological signs of cervical dysfunction; subjective symptoms reported
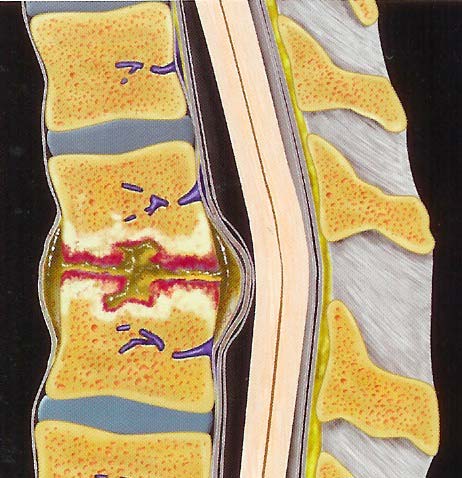
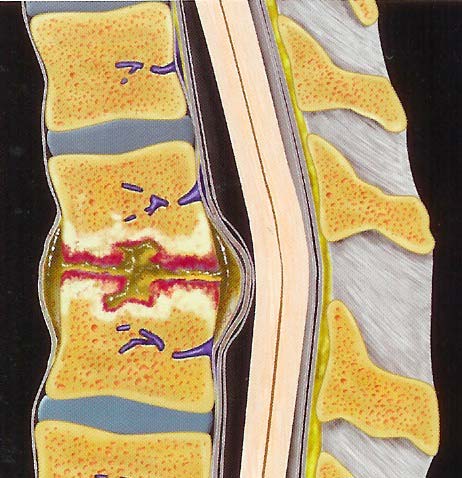
Discitis / Osteomyelitis
- Infection of the vertebral bodies and intervening discs
- Typically not observable in a x-ray during the early stages
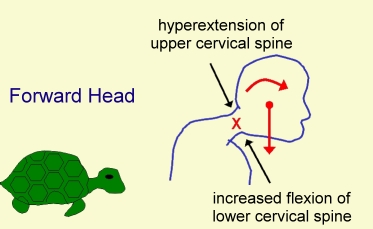
Malalignment
- forward head (turtle neck)
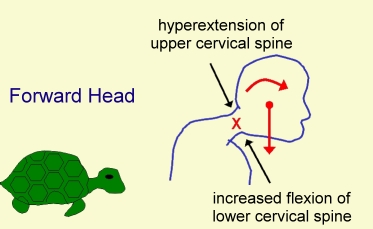
- hyperflexion of lower cervical spine
- hyperextension of upper cervical spine
Self-Assessment
Prepare for the test by checking your understanding of spinal disorders
Common Spine Surgery
- Foraminotomy: Bone and/or other fibrous tissue is removed in and around the foramen to decompress the affected nerve root
- Laminectomy: The vertebral lamina is removed to decompress the central canal or to relieve pressure secondary to spondylosis and spondylolisthesis
- Discectomy: A portion of the herniated disc is removed to decompress nervous tissue; involves a laminectomy to access disc contents
- Fusion: Use of hardware, bone grafts, screws and metal cages to eliminate segmental motion due to instability and/or pain
- Disc replacement: replacement of IVD with prosthesis
- Vertebroplasty: bone is injected with cement-like compound to increase strength of bone tissue following compression fracture
Post-operative Complications
- thrombophlebitis
- pulmonary infection
- hardware failure
- persistent pain
- sexual dysfunction
- spinal cord injury
- pseudoarthosis
PT Examination and Evaluation
History: Includes positions and movements which increase and/or relieve pain, duration of symptoms, level of irritability, pattern during the day/night, pain quality and location, onset and history of previous episodes.
May include self-report questionnaires to quantify level of pain and/or disability due to lumbar symptoms; can be used to differentiate between physical findings and psychosocial contributors to pain presentation.
Red Flags
During the examination, the PT will review the patient's history to rule out evidence of serious medical pathology. PTs use a systems review process to confirm the condition is within the scope of practice of physical therapy:
- Violent trauma
- Constant, progressive pain that does not change with movement or position
- Thoracic pain
- history of carcinoma, steroid use, drug abuse
- HIV
- Unexplained weight loss
- Persistent severe restriction of lumbar flexion
- Widespread neurological symptoms
- Structural deformity
Musculoskeletal
- postural deviations may indicate mobility restrictions (joint, muscle, etc)
- PTs may assess a patient's ability to self-correct postural deviations with verbal and/or tactile cues
- Range of motion is the primary impairment in LBP and is used to evaluate response to treatment. PTs may use a visual scale to document AROM as it relates to normal values. PTAs consult the evaluation for visual or quantitative assessment of spinal ROM
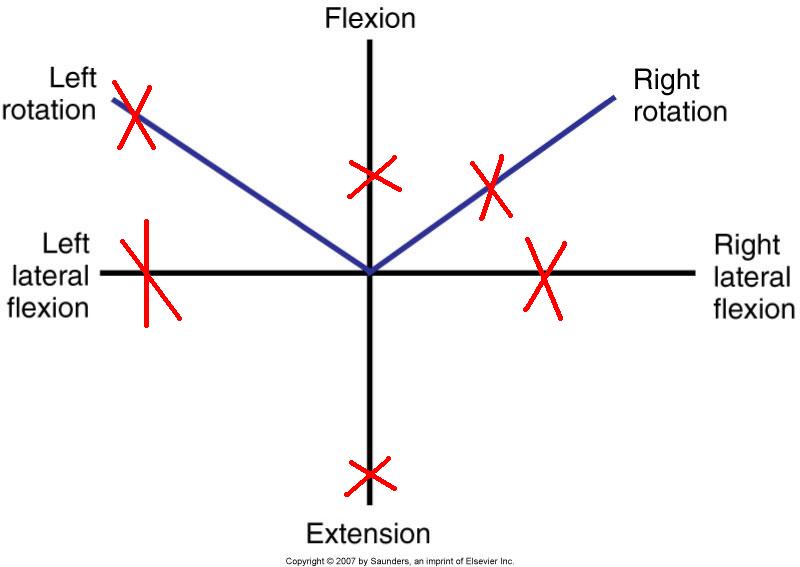
- ROM includes assessing response to overpressures when AROM and repeated AROM are pain-free or minimally symptomatic. The PT will apply gradual manual force to the spine in its end-range to provoke or clear symptoms with each spinal motion or with combined spinal motions (e.g., flexion + rotation R)
- Accessory segmental spinal motion is assessed and is classified as normal, hypomobile, or hypermobile
- abbreviated as PPIVM (passive physiological intervertebral mobility)
- hypomobile: benefits from mobilization, manipulation, stretching and stretching of related muscles
- hypermobile: benefits from stabilization
- Muscle length: often coincides with ROM testing; includes length of muscles which originate or insert on the spine/pelvis
- Muscle strength: MMT and functional tests are used to determine nerve root involvement and may provide information on secondary muscle guarding influences due to pain/perception of pain
- Mechanical Provocation Tests
- used by the PT to determine motions and involved structures which reproduce patient's primary complaint
- Quadrant/Foraminal closure test
- Spurlings is a combination of cervical SB + extension + axial compression + overpressure
- Positive (+) Spurlings is an indicator of cervical intervertebral disc or foramen dysfunction (radiculopathy)
- Cervical Compression
- Pressure is applied through the top of the head (axial loading)
- Positive (+) cervical compression is an indicator of nerve root impingement
- Cervical Distraction
- Cephalad manual traction is applied through the occiput
- Positive (+) cervical distraction test is reported when patient's symptoms decrease during traction and indicates cervical radiculopathy
Neuromuscular
- Pain: PT palpates painful and related structures, noting for warmth and tissue reactivity
- Peripheral nerve integrity: assessed through sensation testing and MMT for spinal dermatomes and myotomes respectively
- Reflex integrity: DTRs which are exaggerated, diminished or absent indicate spinal or other nervous system pathology
- Neurodynamic tests: Involves applying mechanical stress (stretch) to nervous tissue to distinguish nerve root compression and peripheral neuropathy contributors to patient's complaint
- Straight leg raise (SLR): Positive (+) indicates involvement of lumbosacral nerve roots. The PT should note the degrees of hip flexion when symptoms are elicited. Symptoms can present unilaterally, contralaterally or bilaterally. The PT may include medial hip rotation, hip adduction, ankle dorsiflexion, and/or cervical flexion to increase tension on nerve tissue.
- Prone knee flexion: Positive (+) indicates L2 and/or L3 involvement; may also produce SI pain due to restrictions in the rectus femoris
- Slump test: Positive (+) indicates lumbosacral nerve root compression or lumbosacral nerve involvement
- Upper Limb Tension Test (ULTT): Positive (+) indicates involvement of nerves in the brachial plexus. Movement tests are specific to radial, ulnar and median nerves
Special Tests
- Vertebral artery test: Positive (+) indicates evidence of vertebral artery compromise with end-range cervical motions, especially rotation and extension. High velocity joint manipulation or end-range motions are contraindicated
- SI Joint tests
- Abnormal SI mobility is classified as sacroiliac (abnormal positioning of sacrum on a normally positioned ilium) or iliosacral (abnormal positioning of the ilium on a normally positioned sacrum)
- Standing flexion test: Positive (+) if the PSIS moves upward (cephalad) and forward during lumbar flexion with respect to the contralateral side. Indicates restricted mobility of ilium on sacrum (iliosacral problem)

Sacral fixation test/Gillet's Test: Positive (+) if there is no PSIS movement as one hip flexes toward the trunk (iliosacral problem) (Approximately 1 minute)
Sitting flexion test: Positive (+) if PSIS moves cranially as trunk flexes forward (iliosacral hypomobility) (Approximately 30 seconds)
- Long sitting test: Used to determine abnormal rotation of the innominate on the sacrum
- moving from supine to long sit --> limb appears to lengthen in long sitting--> indicates posterior innominate rotation
- moving from supine to long sit --> limb appears to shorten in long sitting --> indicates anterior innominate rotation
- Compression tests: Positive (+) if manual compressive forces applied in supine to the SI joint(s) reproduce pain complaint
- Limb length inequality: Positive (+) if observed asymmetries with bony landmarks can be minimized or eliminated with placing blocks or shims under the shorter limb
- Prone instability test: Positive (+) if low back pain is reproduced with joint mobilization during active recruitment of lumbar extensors
- Thomas test: Positive (+) if hip flexion is greater than 0 degrees when controlled for lumbar extension. Indicates decreased mobility of hip flexors

Classification Systems for Spinal Disorders
McKenzie Method
Most common classification system for low back pain used in physical therapy
Patients are classified as having mechanical pain (reproduced with movement) or non-mechanical (associated with inflammation or other pathology)
Results of PT examination leads toward categorization of mechanical low back pain. Patients with neuromuscular findings are generally not included in a McKenzie classification system
Specific elements of the PT examination include:
- history
- posture
- movement testing (standing, sitting, prone, prone, etc.); repeated and sustained movements/positions
- pain with movement
- palpation and joint mobility
- range of motion
Movement testing
Lumbar motion tests are performed in straight planes and with combined motions
The PT monitors symptom location and intensity with sustained and repeated motions
centralization: pain presents proximally and in the spine
peripheralization: pain presents proximally and radiates laterally and distally with movement
Following the examination, patients are can be placed in one of three (3) syndromes:
- Postural
- Dysfunction
- Derangement
Delitto Treatment-Based
Determines if the patient can be managed by PT alone or requires MD or other health care provider involvement
Factors level of disability due to LBP into treatment classification
Key examination findings result in classification as needing immobilization, mobilization, specific exercises, traction
Movement-Based Impairment (Sahrmann)
Based on postural and kinesiological assessment which includes postural and spinal changes in static positions and with limb motion.
Patients are classified based on the direction of motion which reproduces the pain complaint.
Treatment emphasis is on restoring normal muscle length/balance and eliminating compensatory strategies.
End of Lesson
In lab we will apply some of these concepts to exercise selection and traction applications.
I recommend you work through the practice activities more than once to confirm your understanding of the material as it relates to the objectives
![]()

![]()
![]()
![]()
![]()
![]()


![]()
![]()