Arthritis Pathologies
PTA 104 Orthopedic Dysfunctions
Introduction
Arthritis is a general category which describes signs and symptoms of joint inflammation. In this lesson, our focus is on two major forms of arthritis: osteoarthritis and rheumatoid arthritis. Arthritic conditions are encountered across the life span, and the PT/PTA team play a significant role in applying knowledge of kinesiology and range of motion and strengthening principles into an effective exercise and physical wellness program
Lesson Objectives
- Describe and select an example of the clinical signs and symptoms of arthritis
- Compare and contrast characteristics of OA and RA
- Describe precautions and contraindications for exercise and activity for a patient with active RA
- Describe how principles of RA management depend on the stage of the disease
- Integrate principles of play into an intervention for joint protection in a pediatric client
- Describe the effects of steroidal medication on the musculoskeletal system
Osteoarthritis (OA)
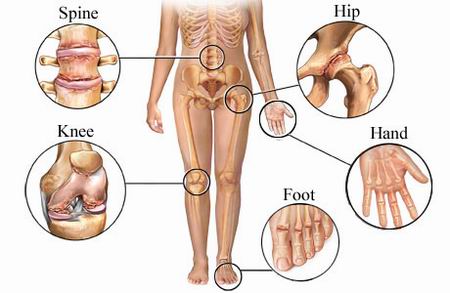
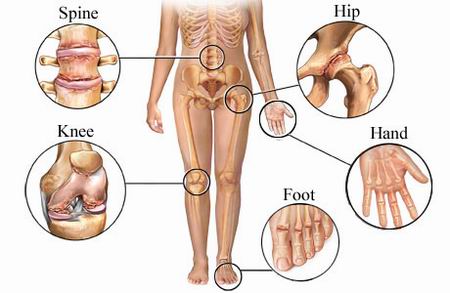
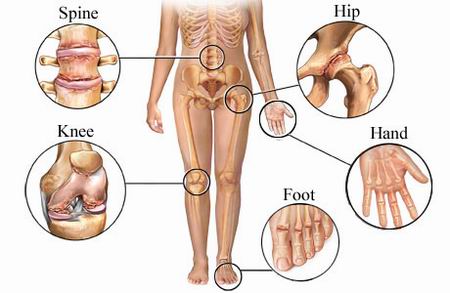
A chronic, degenerative disorder primarily affecting the articular cartilage of synovial joints, with eventual bony remodeling and overgrowth at the margins of the joint.
Background and Characteristics
- Refers to degeneration and inflammation of bone and cartilage in articulating (moving) areas
- Pain with weight bearing and joint motion can progress into partial to full loss of motion and pathological fusion (ankylosis)
- Osteophytes (bone spurring) may be identified on x-ray or diagnostic imaging. They can form in response to abnormal joint stresses
- http://www.medical-look.com/Joint_pain/Osteoarthritis.html
- Pathological bone remodeling can lead to ligamentous laxity and joint hypermobility/instability
- Can result in secondary nerve or postural dysfunction due to loss of joint height/space
- Symptoms are exacerbated with overuse, weather changes, or prolonged immobilization
- Associated with advancing age and family history (primary OA), lifestyle habits (sedentary, obesity, high-impact sports, repetitive loading/lifting), prior fracture or injury, and loss of bone density (secondary OA)
Signs and Symptoms
- pain - localized and referred
- impaired joint mobility (typically a capsular pattern)
- firm end-feel indicates chronic presentation
- guarded end-feel indicates acute presentation
- includes effusion and/or crepitus
- loss of accessory joint motion
- impaired muscle performance
- muscle length-tension relationships
- inadequate activation or guarding of postural stabilizers
- impaired balance
- joint degeneration limits feedback from proprioceptors
- functional limitations
- may need adaptive equipment to complete a functional activity or to protect joint(s) from further injury
Principles of Management of Osteoarthritis
- Patient instruction
- Pain management—early stages
- emphasis is on reducing joint stiffness, balancing activity and rest, and reinforcing the role of movement in joint health
- Pain management—late stages
- consider modalities for home use, pacing and prioritizing, modifying activities
- Assistive and supportive devices and activity
- bracing, aquatics, assistive devices for ADLs, home and environmental modifications
- Resistance exercise
- emphasis is on strengthening within non-painful ranges, isometrics to minimize disuse atrophy
- open chain activities with resistance across long lever arms can increase joint loads and exacerbate arthritis symptoms
- Stretching and joint mobilization
- assisted and patient instruction in safe and effective technique
- involved joints typically have a firm end-feel due to bony changes in the articulating areas
- Balance activities
- Aerobic conditioning
- patient education on exercise parameters, including low impact-low joint stress activities
Rheumatoid Arthritis
An autoimmune, chronic, inflammatory, systemic disease primarily affecting the synovial lining of joints as well as other connective tissue. It is characterized by a fluctuating course with periods of active disease and remission.
Background and Characteristics
- Source of pain is inflammation of the synovium
- Typically presents bilaterally, with >=3 joints involved, redness and increased skin temperature
- Higher incidence in women and can be diagnosed in childhood (Juvenile Rheumatoid Arthritis (JRA))
- Autoimmune response is thought to be triggered by some bacterial or viral exposure
- Some association with family history and presence of rheumatoid factor (RF) in the blood
- Morning stiffness in affected joints can last an hour or more
- May also lead to osteopenia (bone thinning) in wrist and hands
Pharmacology Management
Prednisone and other steroid-based medications are used to treat RA. There are numerous drug side effects, including an increased tendon rupture and muscle weakness, particularly proximal muscles, which can increase pain, limitation and disability.
Principles of Management of Rheumatoid Arthritis
Acute Inflammatory Period
- Joint protection
- especially the smaller joints in the hands and feet
- splinting to protect from subluxation due to hypermobility from synovial degeneration
- includes patient instruction in correct exercise technique to prevent further joint stresses during activity
- Energy conservation
- Joint mobility
- stretching is NOT performed when joints are swollen (increased risk for subluxation)
Consider the image above: think about how muscle and ligaments involved at the knee might be affected by this type of inflammation.
- Exercise
- PROM, AAROM, AROM depending on pain and swelling in affected joints
- Functional training
- similar to OA; instruction in methods to incorporate joint protection in everyday activities
Subacute and Chronic Stages
Common deformities at the wrist and hand in RA include
- Boutonniere deformity of thumb
- Ulnar deviation of metacarpophalangeal joints
- Swan-neck deformity of fingers
Exercise considerations
- To improve function, exercise should be aimed at
- improving flexibility, muscle performance, and cardiopulmonary endurance
- Nonimpact or low-impact conditioning exercises such as swimming and bicycling
- Group activities such as water aerobics
Juvenile RA
- classified as inflammatory, autoimmune arthritis lasting at least 6 weeks in a child younger than sixteen
- three major subcategories:
- systemic onset - includes spiking fevers and a short-duration rash in the trunk and extremities
- polyarticular - five or more joints; often affects the same joint bilaterally
- pauciarticlar - typically affects just one joint but as many as four; most common in the knee
- benefits from PT/home exercise program in
- avoiding high-impact activities
- splinting to rest joints
- engaging in fun, low impact endurance activities
- daily prone positioning to stretch hip and knee flexors
- exercise to encourage neutral and upright posture
- monitoring and correcting leg length discrepancies