Balance Testing and Interventions
204L Neurological Dysfunctions Lab
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
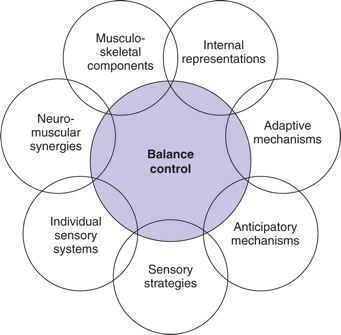
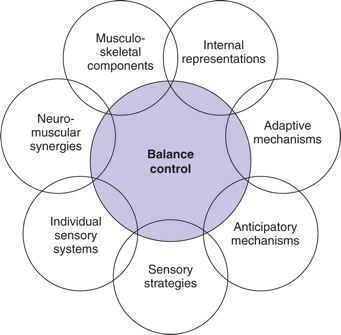
There are multiple models for looking at the role of systems in maintaining balance
Motor Control: Theory and Practical Applications,ed 2, Philadelphia, 2001, Lippincott Williams & Wilkins.
Balance is complex.
Balance control includes continuous coordination of sensory, motor, and cognitive systems. Selecting balance interventions, and measuring the effect of these interventions, is a fundamental skill for the PTA.
Balance impairments can result from pathologies and injuries that effect central nervous system processing. Altered sensation processing from the senses and periphery can influence motor planning, motor control, and motor responsiveness. Effective treatment of balance disorders is dependent on determining the cause of the impaired balance. Let's say this again, because this is IMPORTANT!
Effective treatment of balance disorders is dependent on determining the cause of the impaired balance
Contributors can be musculoskeletal, neuromuscular, sensory, or cognitive, or some combination. Unsteadiness, dizziness, and loss of balance is often attributed to disorganization or conflicting information from the sensorimotor system.
Fay Horak and colleagues at OHSU have studied balance extensively, and developed an alternative schema for looking at balance control. They have identified six categories that influence balance. These include:
There are three primary categories of balance control during functional activities: static, dynamic, and automatic postural reactions (Dutton, 249)
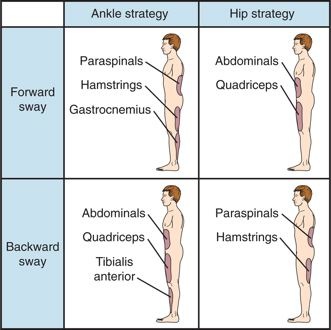
There are predictable balance strategies which are selected in response to a postural perturbations and/or loss of balance in order to prevent a fall.
Loss of balance and falls has a significant impact to older adults. An excellent resources for your future practice is the CDC progrram STEADI - Stopping Elderly Accidents, Deaths & Injuries
Statistics for related to falls in Oregon include:
Due to the high risk of injury when treating patients with impaired balance, best practices include setting up the treatment environment to challenge balance, but prevent injury from falls. This includes the use of a gait belt or harness, performing the exercises near a railing, and closely guarding the patient.
The Berg is a validated balance assessment which has been shown to be a reliable predictor of fall risk. It assesses static and dynamic components of sitting and standing activities in multiple planes. Standardized assessments are valid when they are administered consistently and systematically according to published guidelines.
The Berg is most applicable to older adults when assessing fall risk.
Berg Balance Scale Demonstration
CDP Demonstration
This assessment tool is a valid fall predictor and is sensitive to identifying vestibular dysfunction. Sensitivity, however, is contingent on correct administration of the test.
Dynamic Gait Index Demonstration
MiniBEST Test Instructions and Scoring Form
Fay Horak and colleagues at OHSU have researched balance and falls and have developed and tested (validity and reliability) this method to assess balance.
The MiniBEST has been shown to have less of a "ceiling effect" compared to the BERG. What does this mean? Can you think of a clinical reason about why you would select the BERG over the MiniBEST or vice versa?
Notice the "Subscore" areas on the MiniBEST form....see if you can develop your own ideas around why these subcategories are included as major factors for improving balance and preventing falls.
Selecting interventions is based on the PT plan of care. Activities to restore and improve balance function should be directly related to a documented impairment, functional limitation, or disability. Conversely, impairments observed and/or measured by the PTA which are not included in the evaluation findings should be communicated to the supervising therapist for consideration and review.
Stretching
Upright posture and postural adaptations plays a significant role in fall recovery and balance strategy selection. Flexibility in the spine, hip, and ankle play a direct role in sensorimotor function.
Strengthening
Similarly, strengthening exercises for the postural and lower body muscles can improve balance and decrease risk for falls. Task-oriented approaches to strengthening enhance motor learning and functional recovery specific to the patient's functional short and long term goals. Therapists may integrate multidirectional resistance or perturbations to increase strength in muscles recruited during hip and ankle strategies. Balance and/or frequency of falls are impacted by the increased endurance which results from a strengthening and conditioning (cardiovascular) program.
Sensory Training
Activities which specifically challenge the visual, vestibular, and proprioceptive systems are included as interventions for sensory retraining. Interventions are targeted to effect a change in underutilized sensory inputs in order to integrate these multiple systems into an effective fall prevention strategy. Pain after joint injury alters proprioception, so interventions for recovering normal joint function typically include proprioceptive activities.
Interventions may also include providing adaptive strategies to compensate for compromised sensory systems. Large print, ergonomic modifications to prevent end-range activities (forward bending, overhead reaching), enhanced lighting/visual contrasts are examples of strategies to use in the home and community environments to prevent falls due to impaired sensation.
Perception training
Examples of activities which integrate sensorimotor training principles include eyes open/closed, variable surface consistencies, balance boards, performing a functional activity while on stable/unstable surfaces, enhanced feedback (e.g., knowledge of results using visual or auditory feedback).
Postural Awareness Training
Examples of interventions include progressive weight shifting and standing activities in double-limb and single-limb support. The intended outcome is that the patient can anticipate, assume, and maintain weight shifts in multiple planes without loss of balance. Strengthening of postural muscles and lower body stabilizers are requisites for postural awareness training.
Dynamic Gait
Interventions for dynamic gait should include environmental constraints for which walking is functional. For example, curb training, visual scanning/trunk rotation with walking (e.g., safely crossing streets), and maneuvering around obstacles are activities which may influence decisions about level of independence in community.
Vestibular Exercises
Vestibular exercises are specifically selected to enhance coordination and agreement between the visual and vestibular systems. When input from vision conflicts with vestibular input, then symptoms of vertigo (dizziness, nausea, altered gaze, disorientation) may result.
Examples of vestibular exercises include eyes fixed-head moving, and eyes moving-head fixed while tracking an object through multiple and variable directions of motion. These can be performed in sitting and standing, statically and dynamically.
STOP Here!
Do you want to learn a little deeper? Do you want to develop some clinical reasoning skills?
There are no wrong answers here and there are no points or extra credit for this exercise (but I promise it will help grow your thinking). So, simply focus on your learning and less on trying to "nail it". Experiment. Observe. Notice. Reflect.
*******Stop right now and jot down two exercises or activities that you think might help improve your balance (static and/or dynamic) in sitting.
Good.
Now - How many possible systems or combination of systems are being challenged by these selected activities? WRITE THESE DOWN WITHOUT looking at your notes or in the book or going back in this lesson. Take no more than five minutes to complete your brainstorming. Don't worry if you cannot recall the correct medical terminology - just write down what you think is happening from a neuromotor and neurosensory perspective.
Next, TRY the activities YOURSELF. Quietly reflect on what you perceive as you perform the activities. Do this NOW.
Open "DidYouKnow" link AFTER you have completed the above.
 http://www.mountpleasantgranary.net/blog/images/Sitting-on-the-bench.jpg
http://www.mountpleasantgranary.net/blog/images/Sitting-on-the-bench.jpg
Challenging and Progressing static balance control into functional activities include:
 http://upload.wikimedia.org/wikipedia/commons/1/13/Elderly_exercise.jpg
http://upload.wikimedia.org/wikipedia/commons/1/13/Elderly_exercise.jpg
Note how this concept of stabilizing under dynamic conditions translates to musculoskeletal practice.
http://upload.wikimedia.org/wikipedia/commons/e/e3/Balance_with_one_leg.JPG
Apply your understanding of functional movement and balance strategies by watching this demonstration. How is the PT using physical and verbal cues to facilitate function and provide an appropriate challenge.
In lab, you are going to continue to work on generating ideas to improve balance, and connecting your ideas to evidence and movement science. Looking forward to it!