Interventions for Neuromuscular Reeducation
PTA 204L Neurological Dysfunctions Lab
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions.
D.W. Fell introduced a clinical decision-making framework for selecting and progressing interventions in this population. All interventions typically applied in this population (e.g., gait and locomotion training, functional training, balance and coordination training, conditioning and reconditioning) can be selected and progressed based on clinical decisions that fall into one or more of these three categories:
In clinical practice, there are a variety of manual techniques used to facilitate functional recovery in patients with neuromuscular impairments. In laboratory practice, we will learn and practice the technical aspects of a few, selected rehabilitation techniques (e.g. manual contact, direction of force, cues, etc.).
During skill checks, you are graded on your ability to technically perform the selected techniques with some level of accuracy. In clinical practice (and practical examination), you will select appropriate interventions based on how you can best help the patient relearn movement patterns and restore postural control.
PTAs can provide opportunities for patients with sensory dysfunction to attend, discriminate, and functionally adapt to sensory information so that movement improves during functional activities. In PTA 132L, 133L, and 104L, we introduced orthopedic interventions, such as closed chain activities, that facilitate improvements in kinesthesia and proprioception. Additional examples of interventions to support sensory systems while working to improve movement and motor control include:
PTAs instruct patients and family members in strategies to increase attention to sensory stimulation and integration. As patients recall and reuse strategies to attend to stimuli, the neuromuscular system is set up to become as successful as possible. Sensory neglect and visual field cuts impact safety and recovery of the involved side. As the patient progresses, cueing should decrease and the situations and environments should be made progressively more complex to optimize functional recovery. The following are examples of using multi-modal feedback to promote attention to areas of sensory impairment and neglect during functional tasks:
Following CVA and TBI, patients experience varying degrees of deficits in central nervous system processes which are necessary for normal movement. The level of motor impairment and potential for functional recovery is evaluated by the physical therapist. A summary of examination processes are included in the Interactive Lecture: Neuromuscular Examination Elements.
|
Prerequisites for Motor Control |
Typical Motor Control Components |
Atypical Motor Control Components |
|
cognition - perception
|
able to:
|
apraxia memory impairments disorientation |
|
range of motion
|
normal alignment of body segments normal length-tension on muscle and connective tissue
|
contractures increased connective tissue formation (stiffening) disuse atrophy |
|
sensation
|
intact, two-way communication between sensory and motor systems
|
somatosensory and kinesthetic deficits slow velocity decreased accuracy |
|
strength |
appropriate effort and force production in a muscle |
reduction of motor units available for activation selective atrophy (decreased fast twitch) reduced firing rate of motor neurons |
|
tone
|
tension between origin and insertion of a muscle
|
hypotonic hypertonic spasticity |
|
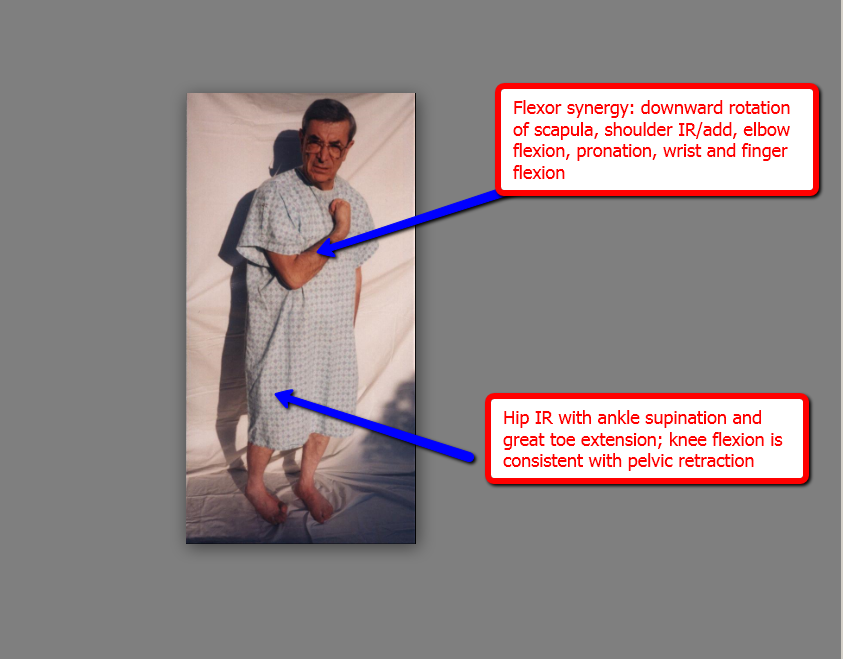
synergies |
patterns of contractions which are variable and flexible stabilize body segments during movement produce movement
|
Non-selective movement patterns Stereotypic and predictable movement patterns flexor synergies extensor synergies |
|
adaptability
|
ability to modify motor programs and make predictions/plan based on the environment; integration of
|
Rigid and inflexible responses to initiating/producing movement
|
prolonged pressure on long flexor tendons of hand low, oscillating movements, incorporating trunk/limb rotation
weight bearing positions: quadruped, kneeling, plantigrade standing
sustained stretching in upright postures
active contraction of antagonists to spastic muscles
electrical stimulation to antagonists
ice wraps/packs
splinting (positioning, pressurized)
![]()
NDT as a neuromuscular and functional reeducation technique now includes neuroplasticity as a basis how the brain can change and reorganize itself and its processes based on practice and experience
|
Individualized Functional Outcomes |
Patient: Life role, supports systems, home environment, patient's goals ICF: Pathologies, abilities, limitations |
|
Motor Control |
Optimize use of systems (sensory, musculoskeletal) and available movement patterns/synergies |
|
Target the Involved Side |
Progressive, increased demand and functional use |
|
Motor Learning |
Closed vs. open environment, simple vs. complex, part vs. whole, practice and feedback/knowledge of results
|
|
Team-Approach |
Coordination with rehab team, parents/caregivers, and support staff to allow for continual practice and consistent use of facilitation strategies |
Key elements to Applying NDT
http://www.stonecrestmedical.com/CPM/Neuro_Ball.jpg
|
Alignment
|
Cannot impose normal movement on malaligned joints
|
|
Handling
|
Inhibition, Facilitation, Key points
|
|
Placing
|
Assisting patients in achieving the appropriate
|
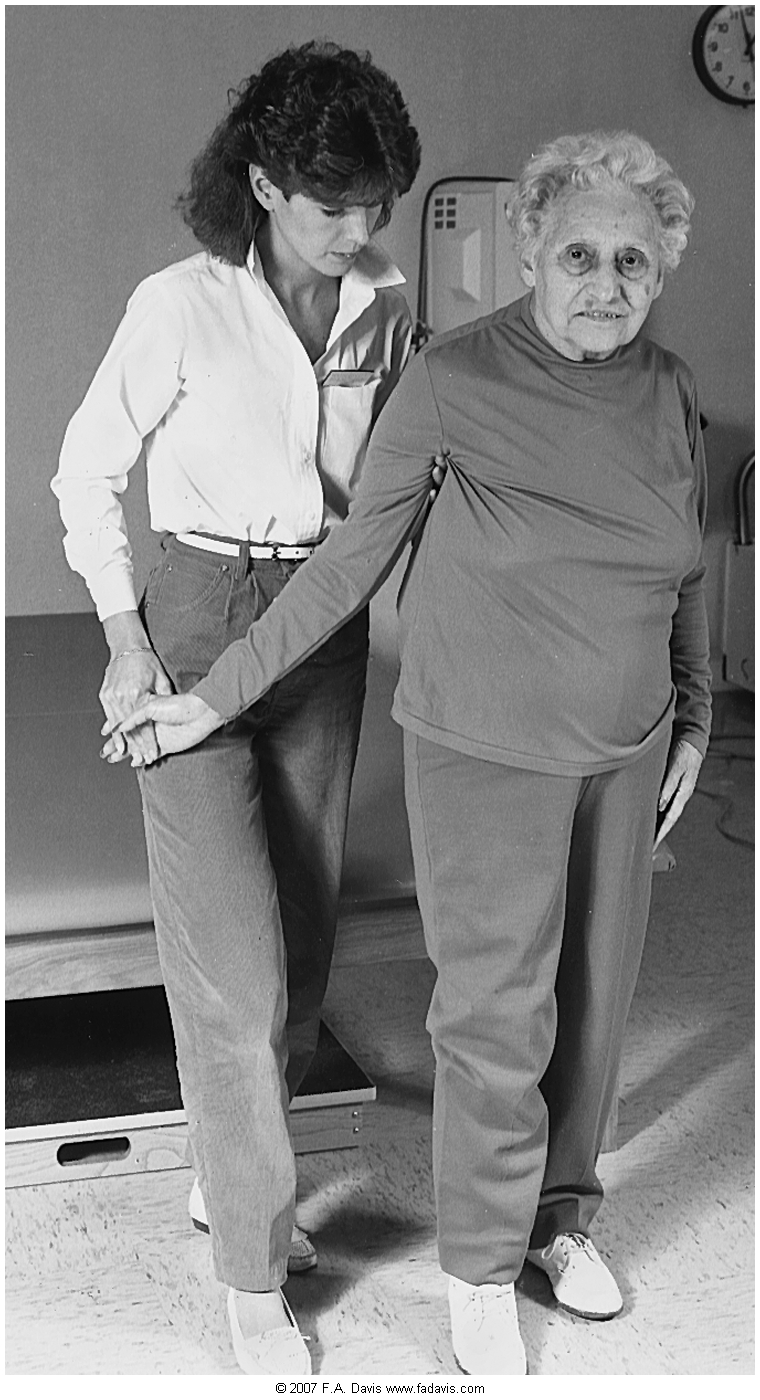
Alignment Check points - PTs and PTAs use manual contact to establish, align and assist the patient with these key elements

Functional Check points - PTs and PTAs will modify manual cues and feedback to the demands of the task and the ability of the patient. Examples of functional check points include:
http://www.mitaka-supply.com/02en_models/102m165/p2.gif
|
Starting Posture |
Missing Components |
Manual Cues |
|
Begin and assess the most efficient posture from which to move (typically upright) Reorient to midline (head/trunk) Neutral alignment of body segments
|
Observe starting posture and make comparisons to normal Review the evaluation and POC for PT assessment of primary impairments (e.g. decreased ROM, strength, sensation, control) Select a movement-based functional intervention which progresses patient toward mobility goals |
Use hands on key points of control to facilitate normal posture/movement and inhibit abnormal posture/movement May includes manual stretching if PT has determined ROM/muscle length interferes with function |

http://www.wingatehealthcare.com/images/location_photos/worcester/img11.jpg
Proprioceptive Neuromuscular Facilitation (PNF) is a stretching technique used to increase range of motion, flexibility, and improve muscle performance (Hindle, Whitcomb, Briggs & Hong, 2012).
Initially developed by Kabat, Knott, and Voss, PNF is applied to treat impairments associated with neuromuscular conditions and musculoskeletal conditions. There are multiple theoretical mechanisms proposed for the effects of PNF, largely based on antagonist inhibition with maximum voluntary contraction.
Manual contact enhances the muscular response and faciltates recruitment. This can occur through indirect (distal) and direct facilitation. Manual contact can also influence the direction of force produced; therefore manual contact should be in placed to inform the direction of motion.
Resistance is applied based on the desired action from the patient. For example, if the patient needs to stabilize in a position, the resistance is applied in a slow velocity and in a direction that requires the patient to and "match" the resistance. This is referred to maintained isotonic contraction. Unlike an isometric contraction where there is no movement ("hold"), isotonic contractions is a recruitment pattern where the muscles are trying to prevent external forces from producing movement ("don't let me move you").
Note the manual contact and the appropriopriate resistance demonstrated in the video clip and how hand placement, speed, and verbal cuing influences the motor response.
On a neuromuscular level, motor responses are heavily influenced by pressure receptors. Therefore, appropriate pressure is a necessary component for influencing the direction of motion and facilitating a maximal response. Manual contact should impart a feeling of security and should not be painful. Proper body positioning and mechanics are preliminaries for appropriate application of pressure.
NDT and PNF are specific for an open hand approach to facilitating movement: there is no grasping the patient to facilitate optimal alignment or movement.
With NDT, contact is very light initially and allows for a graded increase in pressure depending on the stimulus needs of the patient.
Appropriate resistance is that amount of manual resistance which facilitates a maximal response while still allowing a smooth and coordinated contraction. Maximal resistance facilitates irradiation and overflow from stronger components to those that are weaker. Emphasis should be placed on avoiding the valsalva maneuver.
Resistance during PNF is dependent on the desired outcome of the intervention. For example resistance applied to build stability will differ in speed and force than resistance applied to produce a stretch
Gross motor skills are task-specific: physical therapy providers need to be able to work in and at the bedside, on hi-low mats, in parallel bars (sitting/standing) and in functional environments (bathroom, kitchen, car). Principles of good body mechanics (center of gravity, base of support, flexibility) must be observed during skill check and clinical activities.
Safety for you and your patient is the key to a successful treatment and career. Follow your clinical site's policy on use of a gait belt. In some cases, you will not be covered under Workmen's Compensation if you are injured during patient care and DID NOT follow safety policies and procedures, including correct use of a gait belt. When in doubt, put on the belt!
Cueing should be simple, concise, audible. Depending on the condition and patient status, the patient should be given ample time to respond volitionally to the motor command. PNF cueing emphasizes the desired response (e.g. "hold" vs. "don't let me move you")
Alternate isometric resistance to various manual contact points to enhance balance. Direction of pressure and hand positions are altered smoothly, increasing and decreasing resistance slowly, so that the patient continues to maintain a stabilizing contraction
|
Lumbar Spine Anteriorly/Anterior pelvic tilt |
|
|
Thoracic Extension (facilitation points will vary depending on patient/therapist) |
|
|
Scapula Depression Scapula Elevation Scapula Adduction Scapula Abduction |
|
|
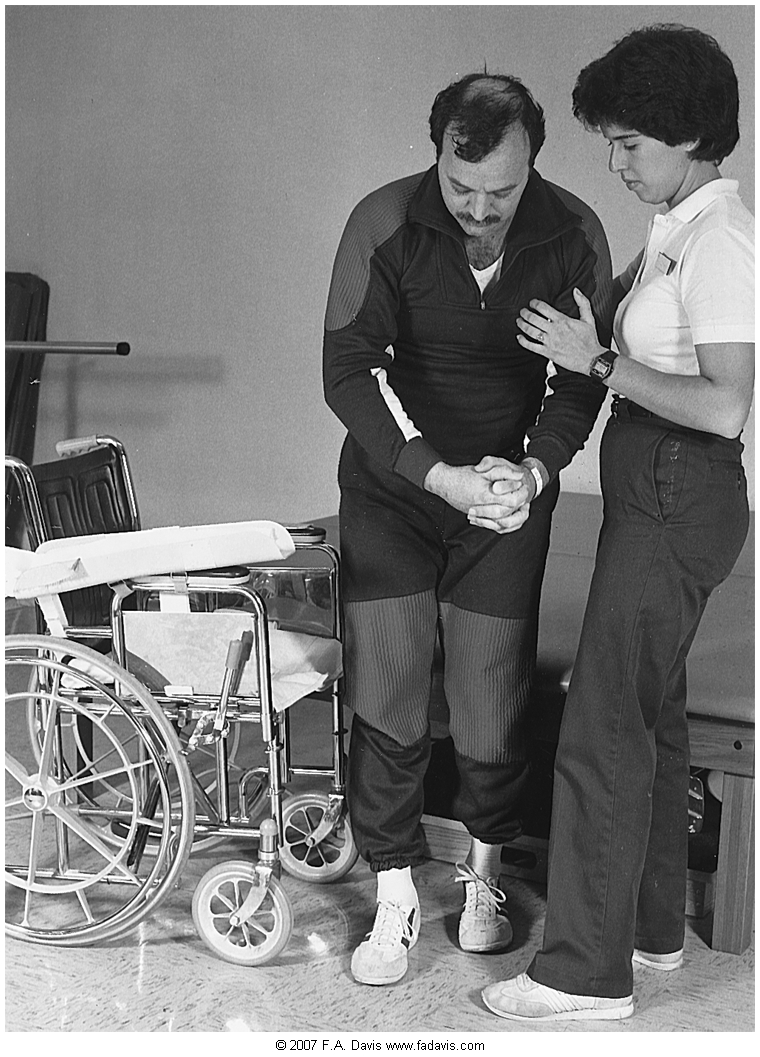
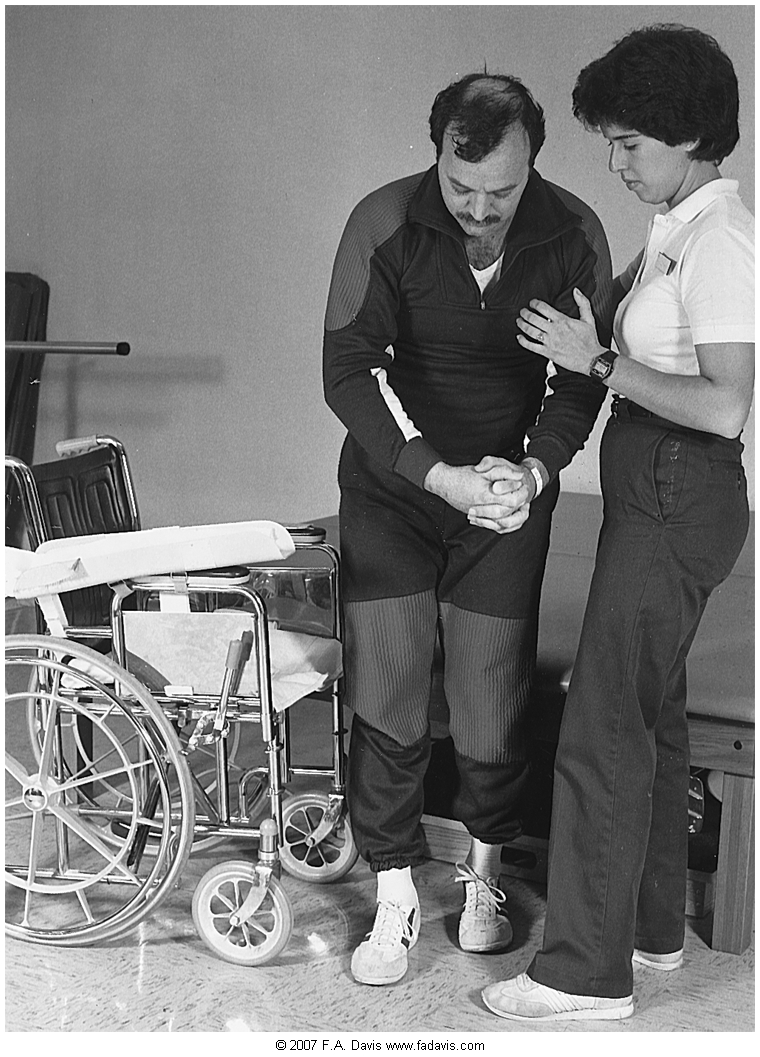
Facilitation of Sit to Stand |
|
|
Scooting in sitting |
|
|
Pre-gait and facilitated gait |
|
Supine to sit with head and neck |
|
|
Log rolling with integration of PNF |
|
|
PDF Copies of Mat Activities |
Download Here, pages 1-2 Download Here, page 3 |
How could this therapist use Fell's framework and manual facilitation interventions to progress this patient's
http://assets.bizjournals.com/story_image/112502-0-0-2.jpg
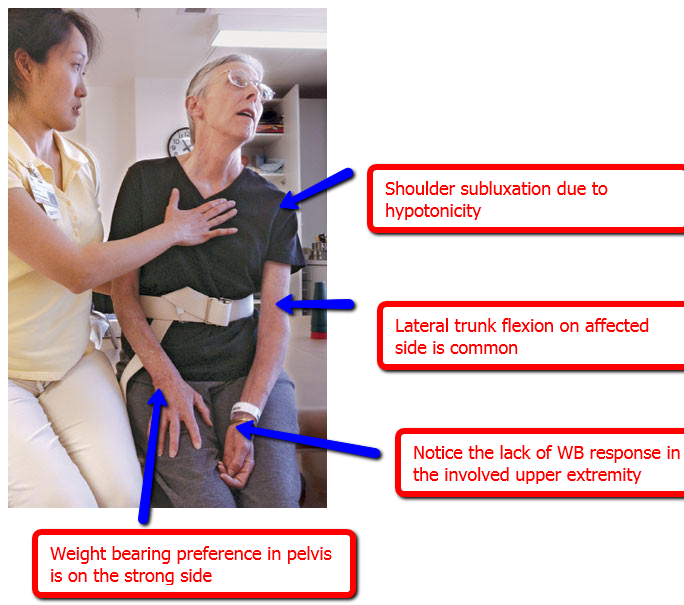
A significant percentage of patients develop some form of shoulder pain following stroke.
Downward scapular rotation and rotator cuff weakness due to loss of motor control on the affected side leads to subluxation of the glenohumeral joint. Pain can result from prolonged stretch, shoulder impingement from malalignment, adhesive capsulitis from loss of active or regular range of motion.
Over time, repeated microtrauma can result in severe pain throughout the limb: Complex Regional Pain Syndrome.
Signs and symptoms of CRPS include: red and swollen hand, cool hand/limb or change in temperature, shiny skin and increased sweating, thenar and hypothenar atrophy
Support a flaccid arm at all times: pillows in bed, wheelchair lap tray, UE sling/hemi sling
Maintain glenohumeral external rotation
Maintain scapular mobility on the thorax
manual scapular ROM
PNF techniques in multiple directions with scapular facilitation
Avoid
passive or active shoulder movements beyond 90 degrees unless the scapula is gliding toward upward rotation and sufficient external rotation is available.
pulleys: they may cause impingement
Educate family members and nursing staff in use of positioning and protective strategies; proper transfer techniques to prevent pulling or lifting on affected limb
|
Supine and sitting |
scapula protraction & slight abduction with neutral GH rotation; humerus is supported |
Fell DW. (2004) "Progressing therapeutic intervention in patients with neuromuscular disorders: a framework to assist clinical decision making. J Neurol Phys Ther. 2004;28(1):34-46
Fisher, BE, Sullivan, KJ. "Activity-Dependent Factors Affecting Post Stroke Functional Outcomes" Topics in Stroke Rehabilitation. 2001;8(3):31-44.
Institute of Physical Art. (2018). PNF [Video file]. Retrieved from https://www.youtube.com/playlist?list=PLN-IyZZvkkxTFISSJbqvuCN1lpgFENPks
Nudo, RJ. "Role of Cortical Plasticity in Motor Recovery After Stroke" Neurology Report, Neurology Section, APTA. 1998;22(2).
Runyan, C. (2008) NDT/Bobath Certificate Course in Treatment and Management of Adults with Hemiplegia: NDTA Inc. Approved Course. Recovering Function.
Shaab, Kathryn R. "Neurodevelopmental Treatment of Adults with Hemiplegia". Sheltering Arms. May 2008. Web 9 Sept 2010.
Velickovic, TD, Perat, MV. "Basic Principles of the Neurodevelopmental Treatment" Medicina. 2005;42(41):112 - 120.
Voss, DE, Ionat, MK, Myers, BJ. Proprioceptive Neuromuscular Facilitation. Philadelphia. 1985. Print