Amputations and Gait Deviations
PTA 205L Complex Medical Dysfunctions Lab
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution or commercial purposes. It is not intended to serve as medical advice or treatment.
Contact howardc@lanecc.edu for permissions
Prior to an amputation, physical therapy provides education in cardiovascular conditioning, therapeutic exercises (upper and lower extremity) for gait, pivot and wheelchair transfers including the use of slideboards as needed, positioning for contracture prevention and management, and initiates instruction in skin/stump care to be carried forward post amputation. Close coordination with the certified Prosthetist will help plan for the definitive prosthesis and physical therapy should coordinate with social work and counseling as needed to help the patient with psychological impacts of preparing for limb loss. The treatment team works with the patient to develop rapport, reduce anxiety, and help set realistic goals
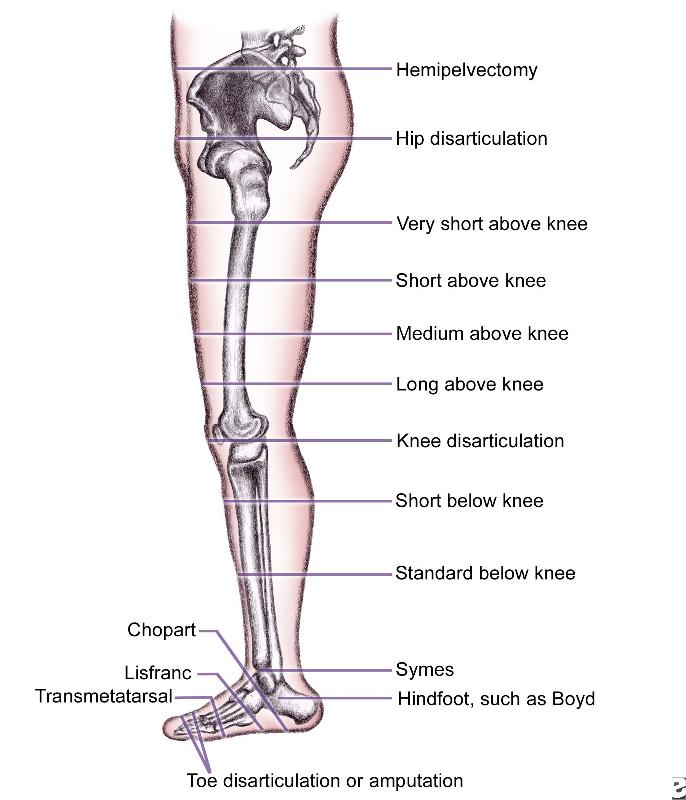
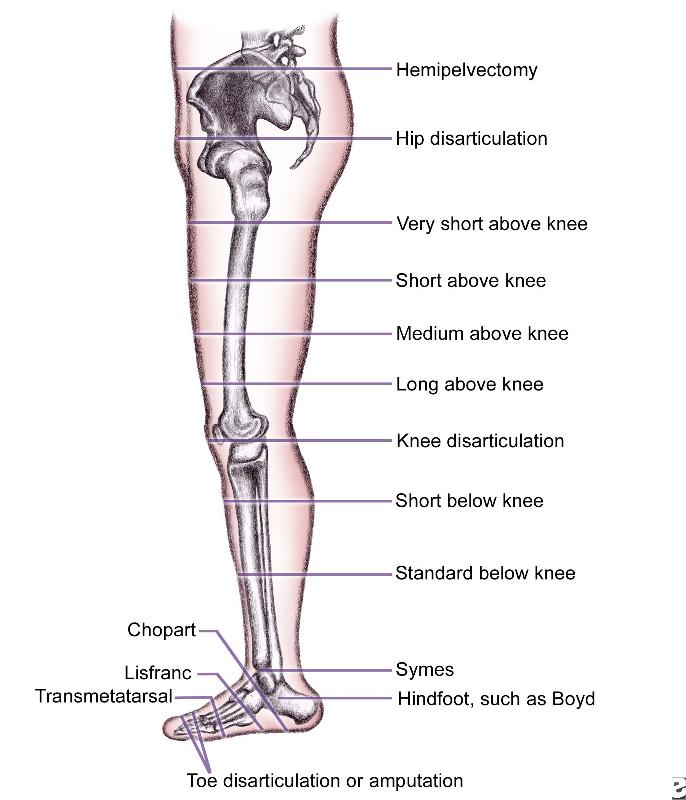
Terminology associated with lower extremity amputation will change depending on the source and audience. For example, transpelvic amputation is commonly known as a hemipelvectomy. A BKA (below knee amputation) is referred to in the literature as a transtibial amputation and an AKA (above knee amputation) is referred to as a transfemoral amputation. A PTA is likely to find references to AKA and BKA , as well as "trans-" in the patient's medical record.
Patients are initially fitted with a IPOP (immediate post-operative prosthesis) within 2-3 hours of amputation for edema management. Use of IPOPs can also promote wound/suture healing and minimize risk for falls when WB in the preparatory prosthesis.

The IPOP is fitted under anesthesia. Patients with fragile diabetes and advanced vascular disease may not be candidates for a IPOP, and will use soft dressings to help manage edema and promote healing.
Shrinkers are pull-on type socks which can offer swelling management when rigid dressing is removed (needs to be worn 24 hours/day
The type of preparatory prothesis is determined by the MD. This test prosthesis is fit as soon as suture is healed. The function of the prosthesis is to continue to reduce edema and allow for adjustability at the final fit and prosthesis type is determined. A patient may need multiple sockets as the side of the limb is reduced and it lacks complete cosmetic finish. Patients are often altering their gait as they learn to ambulate, so adjustability of the prosthesis is key.
Common pressure areas include condyles, fibula, tibial tuberosity, and posterior aspect of the knee
Interventions post-amputation are directed at maximizing function and minimizing complications that result in poor prosthetic fit. The rehab team works closely with the patient to monitor skin, manage swelling, prevent falls, and recondition for the energy cost associated with donning/doffing and ambulating with a prosthetic limb.
Inadequate Knee Flexion - some loss of knee flexion is expected. Physical therapy and the prosthetic team use observational gait analysis to assess what can be adjusted to minimize the loss of knee flexion. Weak quadriceps, hip instability, pain and arthritis may be non-prosthetic sources of the deviation
Toe Out - physical therapy should rule out hip external rotation contracture, hip abductor weakness, and poor trunk stability as contributors to this compensatory pattern
Drop Off - a prosthetist should be consulted when drop off is observed and there is little to no evidence of a knee flexion contracture or substantial quadriceps weakness
Vaulting - this it the most energy consumptive compensatory habit: long prosthesis, excessive pflex of foot, excessive knee resistance or stability. Anatomical contributors include gait habit, fear of catching toe, weak hip flexors, or poor timing of hip flexors.
Quiz Prep: Can you think of balance and gait interventions you might select to help a patient overcome the fear of catching a toe? Or functional activities to improve hip flexor function?
Whips (medial and lateral) - these can result when the prosthesis was not donned in correct alignment and may indicate a need for further patient training in correct donning and doffing techniques
Quiz Prep: Can you think of what your first intervention may be if you observe a medial or lateral whip?
Circumducted - this is the most common transfemoral gait deviation; presents when there is a lack of confidence in flexing knee, long prosthesis, excessive knee friction, excessive knee stability; weak hip flexors, or due to habit (using entire hip and pelvis to advance limb)
Lateral Bending - Reverse Trendelenberg - This is often observed when there is hypersensitivity and/or pain at the residual limb.
Quiz Prep: If you are working with a patient who has a transfemoral amputation and a prosthesis with a locked knee unit, what gait deviations can you expect to see during ambulation?
Quiz Prep: Can you describe why lateral bending is the observed compensatory response if the residual limb is painful?
Fitting a prosthesis is individualized and takes time and feedback to optimize. Patients also change over time (size, bulk, skin, strength, etc.) so prosthesis monitoring for fit and function is ongoing.
Common sources of gait deviations driven by the prosthesis include:
The rehab team should monitor for excessive and prolonged redness on the residual limb following weight bearing and gait in the prosthesis. In general, if redness persists > 10 minutes after prosthesis removal, and the patient has donned the prosthesis correctly, the patient may benefit from a referral to the CPO for component and fit assessment
Demonstration of donning a transtibial prosthesis
Demonstration of donning and doffing a transfemoral prosthesis
Demonstration of basic exercises for residual limb
And a bit about the importance of patient centered practice from some of your future patients
I found some additional online videos to provide examples of gait deviations for your reference. Remember: work with your supervising PT to distinguish what deviations are expected and unexpected. Unexpected gait deviations can be due to the prosthesis, muscle function, coordination deficits, endurance, and pain.
https://www.youtube.com/user/dcraig35/videos
As the patient is progressing toward a determined (i.e., final) prosthesis, there must be documentation of a patient's functional status and ability to benefit from progressively more complex (and expensive) components. "K- Modifiers" are descriptions referenced by Medicare to determine if a patient is eligible for a recommended prosthesis
KO: This patient does not have the ability or potential to ambulate or transfer safely with or without assistance and a prosthesis does not enhance their quality of life or mobility.
Eligible components: SACH or single-axis foot, manually locked, single-axis, polycentric, or weight-activated knee, any suspension or liner, all socket designs
K1: This patient has the ability or potential to use a prosthesis for transfers or ambulation on level surfaces at fixed cadence - a typical limited or unlimited household ambulator.
Eligible components: All of Level 1, also flexible keel or multiaxial feet, rotator and torque absorber
K2: This patient has the ability or potential for ambulation with the ability to traverse low-level environmental barriers such as curbs, stairs, or uneven surfaces - a typical community ambulator.
Eligible components: All of Level 1, also flexible keel or multiaxial feet, rotator and torque absorber
K3: The patient has the ability or potential for ambulation with variable cadence - a typical community ambulator with the ability to traverse most environmental barriers and may have vocational, therapeutic, or exercise activity that demands prosthetic use beyond simple locomotion.
Eligible components: All of Level 1 and Level 2, dynamic response feet, hydraulic/pneumatic knees, dynamic or shock-absorbing pylons. All components allowed.
K4: The patient has the ability or potential for prosthetic ambulation that exceeds basic ambulation skills, exhibiting high impact, stress, or energy levels - typical of the prosthetic demands of the child, active adult, or athlete.
Eligible components: All of Level 1-3, all existing components
Video reflection and assignment preparation: Can you attribute a K level to the persons in the linked videos based on what you have observed functionally?
Physical therapy is often asked to provide summary reports and other impairment and function-based evidence to support a case for determining coverage for a final prosthesis.
Therapists and CPOs can use the Activities of Daily Living Evaluation to provide evidence and support for medical necessity of specific prosthetic components
For additional resources for optimizing reimbursement, visit https://shop.ottobock.us/media/pdf/LLPAuditSurvivalKit.pdf