Electrotherapeutics
PTA 101 Introduction to Client Care
Instructional Use Statement
The following information is used for instructional purposes for students enrolled in the Physical Therapist Assistant Program at Lane Community College. It is not intended for commercial use or distribution for commercial purposes. It is not intended to serve as or take the place of medial advice or treatment.
Contact thorpeb@lanecc.edu for permission
Introduction
Electrical stimulation is used in rehabilitation settings for neuromuscular re-education, tissue repair, and pain management. In this lesson we will review indications, parameters, safety, and expected outcomes of using electrotherapeutics in the plan of care.
Lesson Objectives
By the end of this lesson, the successful student will be able to:
- Describe the principles and theory for electrotherapeutics.
- Describe the physiologic effects for electrotherapeutics.
- Describe clinical decision making in the use of electrotherapeutics for neuromuscular re-education, tissue repair, and pain management.
- Describe procedures for administering electrotherapeutics, including obtaining informed consent.
- Describe the expected goals and outcomes for electrotherapeutics as related to neuromuscular re-education, tissue repair, and pain management.
- Identify the role of the PTA during application of electrotherapeutics.
- Discuss how the patient's medical status may influence selection and outcome of treatments with physical agents.
Neuromuscular Re-Education
Neuromuscular electrical stimulation (NMES) is defined in Behrens as "the use of electrical stimulation for activation of muscle through stimulation of the intact peripheral nerve." Therefore, an appropriate patient candidate for NMES must have an intact, or at least partially intact, peripheral nerve for a positive response. The following outlines considerations for use of NMES.
Contraindications - Absolute
- Demand cardiac pacemaker due to possible electrical interference with signal
Contraindications - Relative
- Any type of cardiac pacemaker
- Pregnancy in the third trimester
- Broken or irritated skin at electrode site
Precautions
- Geriatric and cardiac patients need to be monitored for BP and HR
- Presence of superficial metal (i.e. external fixators, staples, and pins)
- Absent or impaired skin sensation
Considerations for use of NMES
- Two main concerns when planning a treatment with NMES
- quality of contraction of the activated muscle
- patient comfort related to compliance with plan
- Choice of Waveforms
- Symmetrical waveforms for large muscle stimulation such as the quadriceps
- Asymmetrical waveforms for smaller muscles such as those of the wrist flexors and extensors
- Intensity or Amplitude should be increased gradually for patient comfort and tolerance over a 15 minute period. The desired contraction may not be achieved on an obese patient due to adipose acting as an insulator, requiring the use of a high intensity, which may not be tolerated by the patient.
- Units with pulse duration between 200-400 milliseconds are more equipped for NMES use
- Strength-duration curve: low pulse duration takes a high amplitude to elicit a muscle response until >40 m sec
- Pulse rate = frequency, as pulse rate increases, so does rate of muscle firing resulting in a stronger contraction.
- To minimize fatigue, use lower pulse rate,
- Electronically generated muscle contractions recruit in reverse = larger superficial motor units FIRST in synchronous pattern
- Duty cycle = on time/(on time + off time); usually 1:3 or 1:5 ratio or 20-25%; off time is rest time for the muscle to recover before contracting again
- On time generally 2-10 seconds
- Ramp time is the gradual building to maximum current chosen; needs to be less than 1 second and less than the total on time
- Clinically, ramp down allows for patient confort and allows the patient to contract maximally and slowly lower the limb as the contraction
- Use length-tension relationship information: position limb with mild stretch on tissue for muscle contraction
- Visual feedback can enhance muscle control so position the patient to see the muscle movement during NMES treatment
Guidelines for Clinical Application
Strength and Endurance
- Originated with Russian Olympian training in 1976 reporting 10-30% increase in muscle strength using stimulation
- Can be used to supplement conventional exercise and units can be sent home with patient for use during HEP
- Choose electrode size and placement for a "balanced reaction" or full contraction without overflow or pulling into deviation
- Post neurological injury or surgery may leave a patient with difficulty initiating muscle contraction
|
Balanced Contraction
|
Unbalanced Contraction
|
|
|

|
See Behrens's text Box 10-3 on page 181 for patient home use instructions
Edema Reduction
- Leakage of blood cells and plasma proteins into interstitial space occurs after tissue trauma. Blood components are negatively charged and can be pushed from the area with negative polarity exposure.
- Elevate the extremity and use active range of motion for muscle pumping during treatment to enhance response to electrical stimulation
- Current should elicit brief but effective muscle contraction, frequency of 20-50pps
Orthotic Substitution
- Implanted functional electrical stimulation (FES) can be used on the lower extremity to control limb segments through a sequencing of muscle groups during a task such as ambulation.
Partial Denervation
- NMES can be used to retrain muscle after a peripheral nerve injury during the slow reinervation process.
- Return of function depends on degree of atrophy, mechanism and extent of injury, and time lapse since injury
Safety Considerations
- Equipment must be inspected regularly with documentation by professional
- Check patient medical history for any contraindication, precautions or changes since last treatment
- Skin checks BEFORE and AFTER modality - skin may be pink where the electrodes were placed due to increased blood flow but should subside in 30-60 minutes after treatment
- Cognitive issues - patient needs to be able to communicate sensation and follow direction. If cognitive impairment exists, electrical stimulation can still be administered if decided by the PT, however, extra care must be taken to monitor the patient.
Expected Outcomes
- Educate the patient and communicate about the goals of treatment for compliance, set realistic goals
Clinical Decision Making - Documentation
- Comprehensive examination
- Strength grades - isokinetic examinations
- Active ROM/Passive ROM measurements
- Edema and hypertrophy, girth measurements
- Gait description and movement patterns
Electrical Stimulation for Tissue Repair
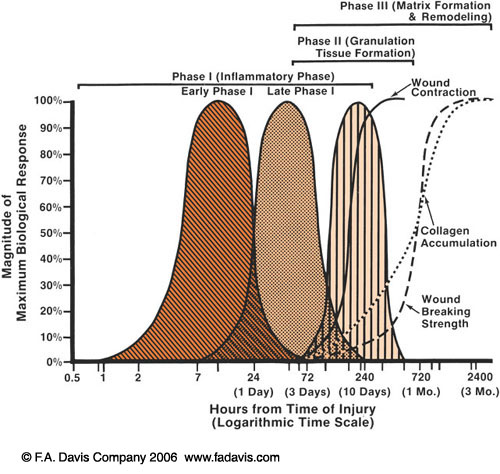
Let's recap the phases of wound healing quickly. Remember that there is a predictable sequence to tissue healing but the phases also overlap.
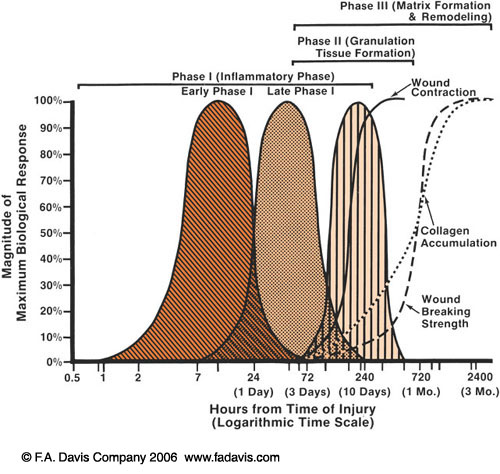
Phase 1: Inflammatory Phase
- Up to 3-7 days post insult
- Immediate vasodilation to protect the area followed by localized vasodilation to bring in the "clean up crew" macrophages via chemical signal or "chemotaxis"
Phase 2: Proliferation (granulation) Phase
- 3 days - 1 month post insult
- Multiple events occurring:new blood cells forming, extracellular matrix to fill space and form granulation tissue as scar tissue foundation, FIBROBLASTS are busy building new tissue, then wound contracts to pull edges back together
Phase 3: Remodeling Phase
- Can start within a few days and last up to 2 years following wound closure
- Significant increase in collagen, converting and reorganizing into strong, more elastic scar
How can electrical stimulation affect wound healing?
"Current of Injury" occurs when there is interruption of the normal skin barrier with negative outer layer (stratum cornue m) and positive inner dermis layers, creating a voltage gradient at the edge of the wound. This positive polarity flows out from the wound and returns via the sodium potassium pump.
- Electrical stimulation may mimic the normal body electric current to facilitate the wound healing process, though not determined
- Wound polarity is initially positive for the first 3-4 days then switches to negative, a sign of healing
"Galvanotaxis" - electrodes act to carry charges cells within the wound since cells are attracted to either a positive or negative pole based on their own opposite positive or negative charge
Indications: wounds from the following categories:
- Pressure (ducubitus) ulcers
- Venous insufficiency
- Arterial insufficiency
- Diabetes Mellitus
Contraindications
- Demand cardiac pacemakers
- Over the carotid sinus
- Site of skin lesions: basal cell carcinoma, squamous cell carcinoma, melanoma
- Osteomyelitis directly under the wound
- Presence of metal from antimicrobial medication or implants
- Lumbar region over pregnant woman
Precautions
- Wounds located at the cranium or upper cervical area
- Patient history of epilepsy, CVA, or reversible ischemic neurological deficiency
Application Techniques
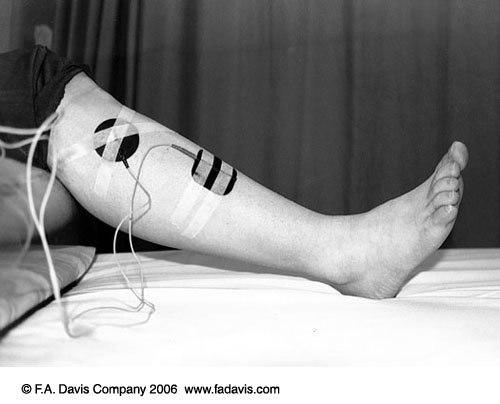
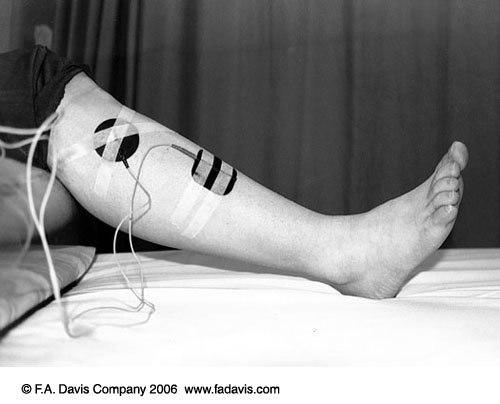
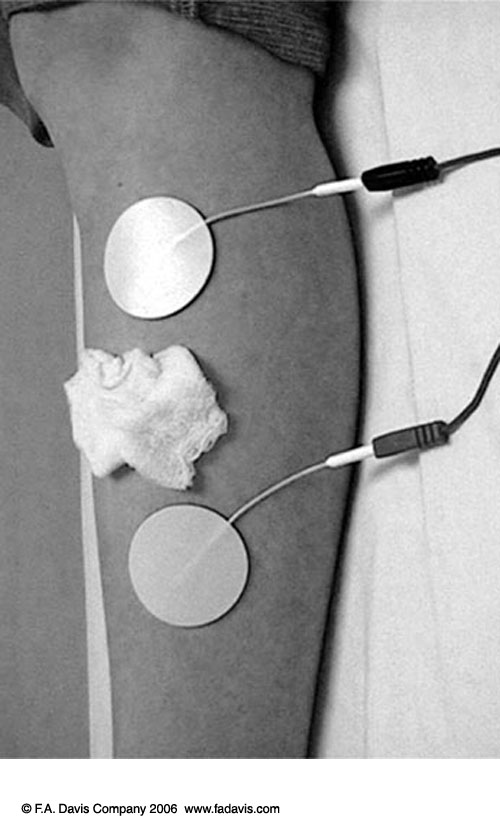
- Direct Technique - Active electrode placed directly over wound with dispersive 15-20cm distal to wound
- high voltage monophasic pulsed current
- saline soaked gauze in wound bed for debridement
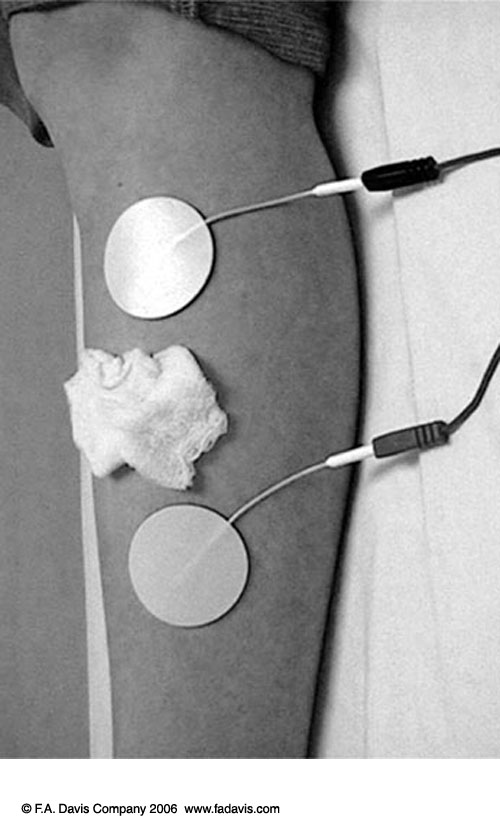
2. Periwound Technique - 2 electrodes are placed on intact skin adjacent to wound
- generall proximal and distal, but can be lateral as well.
- less risk of skin/wound disruption
*See Application Checklist and Patient Instructions in Behren's text
Pain Management with Electrical Stimulation
According to Behren's, Pain management involves controlling the perception and/or sensation of pain.
- actively involves patient to control discomfort
- analgesic effect on central and peripheral nervous system
- block pain by stimulating
Transcutaneus Electrical Nerve Stimulation (TENS)
Application of electrical stimulation across the skin; portable units capable of stimulating nerve receptors and block ascending nerve pathways to gait pain reception
Analgesia vs Anesthesia
Analgesia is the absence of pain or noxious stimulation; the absence of sensibility to pain; or the relief of pain without a loss of consciousness
Anesthesia is a loss of sensation, usually by damage to a nerve or receptor, that is numbness; or the loss of ability to feel pain caused by the administration of drugs or medical interventions.
- Sensory analgesia can produce a "tingling" with activation of A-beta nerve fibers causing a "gating" mechanism at the level of the spinal cord preventing pain from traveling higher, relief usually only occurs while stimulus is being applied.
- Endogenous opiate release may occur with stimulation of A-delta and C-fibers with electrodes over motor points to reach level, mimicking narcotic drugs and decreasing perception of pain; if electrical stimulation can produce the same effect, it can be supplemented for narcotics
- Alcohol also produced analgesia through depression of the central nervous system and should be avoided while electrica stimulation is applied
- Excercise beyond tolerance can produce sharp A-beta pain; electrical stimulation during exercise may be utilized to combat this
Contraindications
- Demand type cardiac pacemakers
- Over carotid sinus
- Directly over the eye
- Epilepsy
- Malignancy
- Loss or decrease in sensation
Precautions
- Monitor patients with known cardia disease or arrhythmia
- Directly over an open wound
- Lumbar region of pregnany person, except during lab pains possibly
- Diagnoses malignancies as terminal, palliative pain relief with informed consent
- External use only, keep out of reach of children
Clinical Decision Making for Electrical Stimulation
Some items to take into consideration:
- Patient's previous experiences with modality
- Presence of contraindications or precautions
- Type, location, characteristics of pain
- Portability of unit
- Electrical stimulation can be used during a painful procedure
- Electrode options, placement options
- Motor points where peripheral nerves enter the muscle, to elicit motor response, electrodes should be placed over these
- Trigger points within a muscle are sensitive to pressure and electrical stimulation
- Sensory analgesia requires more diffuse electrode placement around an area
- Parameter guidelines are listed in the Behrens text Boxes 12-3 through 12-6 for practice in lab
Expectations
- Acute pain in inflammatory phase = decrease pain intensity, break pain cycle, facilitate healing process
- Subacute phase with pain at end range of motion = control pain created by PT interventions at end range of motion during or post treatment
- Maturation phase = treat pain created by interventions
- Chronic pain = will not cure pain = goal of increased function
- decrease intensity of chronic pain at rest
- decrease pain created by therapeutic techniques
- treat acute "flare ups"
Documentation
- Treatment parameters need to be reproducible by others, Objective needs to include:
- type of electrical stimulation used
- mode of delivery
- pulse duration (PD)
- Frequency (F)
- Rise and fall time if used
- Treatment area
- Electrode placement sites
- Duration of treatment
- Goal/response to treatment
End of Lesson
Use the discussion questions to check your understanding of the material. Case Studies and Why Do I Need to Know... boxes offer extra practice explaining the material and making clinical decisions regarding which modality choices are available and appropriate for a patient. Use the CAN YOU HELP ME forum to share ideas or questions with classmates.