Use the information below to fill in the blanks for the Unit 1 Preparations section
II
Cultural Influences on Nutrition and Cultural Competency.
Some of the commonly cited reasons for needing culturally
competent health care individuals includes the following:
- demographic diversity and projected population shifts
- increased utilization of traditional therapies
- disparities in health status of various racial/ethnic
groups
- under representation of health care providers from
diverse backgrounds
Merriam-Webster Dictionary defines culture as "... the integrated pattern of human
knowledge, belief, and behavior that depends upon man's capacity
for learning and transmitting knowledge to succeeding
generations." Therefore, culture is not something we are born
with, but rather it is learned and passed on from one generation
to the next. Culture encompasses more than simply race or
ethnicity because it is a shared system of values, beliefs,
attitudes, and learned behaviors. For example, dress, family
structure, language, and food habits often indicate one's culture.
Below are a few pictures that were taken while my husband lived in
Japan. The first picture shows the traditional attire that is worn
for kyudo, or Japanese archery. The second picture was taken at
the end of a tea ceremony, or chakai, and the women are all adored
in kimonos. The next picture is of me taking shodo or calligraphy
lessons in Japan, and the last picture is of dango, which are
Japanese dumpling made from rice flour and is often served with
green tea.




Every decade a census of the United States is conducted. According
to the U.S. Census 2000, 284 million people live in the United
States. The categories used in the most recent census included
white, black or African American, American Indian and Alaska
Native, Asian, Native Hawaiian and other Pacific Islander, and
"some other 'race.'" Note: Clearly, there are many subgroups
within each of these categories.
The expected changes in the nation's demographic makeup in race
and age categories have been cited numerous times as reason enough
for health professionals to pursue personal competence in cultural
knowledge. It is projected that by 2050 Latinos will triple to become the largest
minority group and the percentage of Asians will nearly double. By 2065 Non-Hispanic
whites will most likely be a minority
group.
The U.S. Census Bureau website, 2005-2007 American Community
Survey includes a breakdown of the demographic characteristics of
Lane County, Oregon:
POPULATION OF Lane County: From 2005-2007, Lane County had a total
population of 340,000 - 172,000 (51 percent) females and 167,000
(49 percent) males. The median age was 38.1 years. Twenty-one
percent of the population was under 18 years and 14 percent was 65
years and older.
Please go
to the following link (http://factfinder2.census.gov) and enter Lane
County, Oregon. Under "Quick Start" enter Lane County, Oregon and
then click on "Go". In the "Search for" box enter "demographics"
and a file titled "ACS DEMOGRAPHIC AND HOUSING
ESTIMATES" should be one of the first files listed. Click on
that file and answer the demographic questions and Lane County
below:
- What percentage of the population in Lane County, OR
considers themselves to be "white"? (Use the percentage under the subject "one
race".)
- How does the percentage of the population that is "white"
in Lane County, OR compare to the overall U.S. population? (The national average is
~74.5% "white".)
- What three racial groups (do not include the categories
"some other race" or "two or more races") comprise more than 1.1% of the
population in Lane County?
- Based on the racial breakdown of Lane County in
comparison to the overall U.S. population, do you think Lane
County is more or less racially diverse than most areas of the
US?
Using the maps below, what do you find to be most surprising or
interesting? (Map 1 on the left or top
shows the percent of the total population who are American
Indian and Alaska Native alone in 2007 and Map 2 on the right or bottom
shows the percentage of the total population who are Asian alone
in 2007.)
Map 1: Percentage of the
total U.S. population who are American Indian and Alaska Native (click
here
for map legend). (Note:
As of 3/29/2012 the link is no longer intact, but the darker the
area on the map, the more concentrated the population group that
resides in that area.)
Map 2: Percentage
of
the total U.S. population who are Asian alone (click
here
for map legend). (Note: As of 3/29/2012 the link is no longer intact, but
the darker the area on the map, the more concentrated the
population group that resides in that area.)
Many agree that the US population is currently more like a "salad bowl" rather than a
"melting pot." A salad may contain many ingredients, and blend
into a harmonious whole, but each ingredient retains its unique
taste and texture.
However, it is not enough to simply recognize and accept that our
culture continues to diversify. Cultural
competency, especially in healthcare, is the ability to
understand and respond effectively to the cultural and linguistic
needs of patients or clients. Implied is the acceptance and
tolerance of different backgrounds and their associated traits,
beliefs, etc., and absence of prejudice against unfamiliar
cultures. Learning to value diversity and being open-minded about
other cultures are key characteristics of cultural competency. A
culturally competent professional recognizes and understands the
differences in his or her culture and the culture of the patient
or client. Therefore, it is no wonder that cultural competency is
a current buzzword in health care.
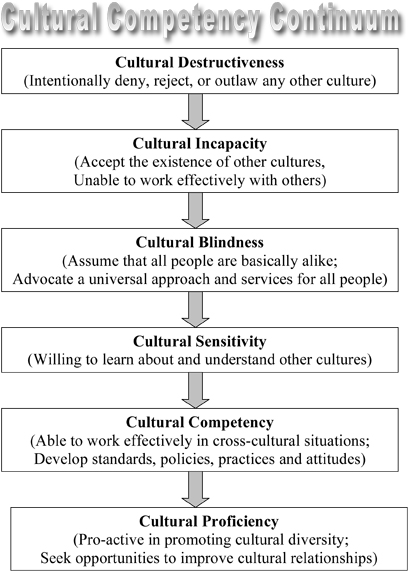
Cultural competency is a process
that occurs along a continuum. At one end of the continuum is
cultural destructiveness and at the other end is cultural
proficiency. The chart below was developed by the National Center
for Cultural Competence in 1999.
According to the University of Michigan Health System, the steps
involved in developing personal cultural competency are as
follows:
- Recognize your own personal cultural biases and
preconceived ideas/opinions;
- Desire to learn about and become involved with people
from diverse cultures;
- Seek out and increase your knowledge about other
cultures; and
- Learn and develop multicultural communication and
counseling skills.
Considering self-assessment is an essential element of cultural
competence, the following activity
will allow you to assess your cultural competence:
Cultural
Competence
Health Practitioner Assessment
- Click on the link above to participate in The Cultural
Competence Health Practitioner Assessment.
- Next click on "Begin the Cultural Competence Health
Practitioner Assessment (CCHPA)" at the bottom of the page to
start the assessment.
- Based your results for the clinical decision-making subscale, which one
recommendation does your profile indicate that you could
benefit from gaining knowledge that you think would be most
practical (e.g. explore the range of holistic traditional
practices used by communities served).
- Which one
of the resources for the cross-cultural communication subscale
sounds most interesting (e.g. Communicating Effectively
Through an Interpreter (1998) (Available from the Cross
Cultural Health Care Program, 270 South Hanford Street, Suite
100, Seattle, Washington 98134; Phone (206)-860-0329; Website
www.xculture.org).
Along this journey to attain cultural proficiency, it is
important to understand the difference between stereotyping and
generalizations. Stereotyping
is an assumption that ALL people in a particular group think and
behave alike. Stereotypes are often judgmental and do not allow
for individual differences--for this reason, a stereotype is an ending point. For example, a
stereotype could be that "All white southerners eat pork, have
buttered grits for breakfast, and drink sugared tea." In contrast,
generalizations refer to
the trends or behaviors within a group, but with the knowledge
that further information is needed to determine if the
generalization applies to this particular person. Therefore,
a generalization is a starting
point. An example of a generalization-based questions is asking a
Jewish client "Do you follow traditional Jewish dietary laws?"
This question provides a starting point to work from rather than
stereotyping that all Jewish clients follow traditional dietary
laws.
Keep in mind that just as individuals within a cultural group are
unique, so are their diets. For example, not all
Japanese-Americans like wasabi. Thus the emphasis should be on
seeing the patient or client as an individual, which is also known as
patient-centered care. Providing patient-centered care can prevent
bias, prejudice, and stereotyping on the part of healthcare
providers from contributing to differences or disparities in care.
After all, the connection with the patient or client is the most important component.
According to the National Center for Cultural Competence, cultural
competency in healthcare is paramount for fostering more favorable
clinical outcomes, results in positive and rewarding interpersonal
experiences, and promotes patient or client satisfaction. In order
for health care to be successful, services must be received and
accepted. The real benefit of cultural competency is improved
outcomes. Cultural competency is NOT an optional skill to learn,
but rather a necessity.
In order to deliver culturally competent care, health care
providers should understand: beliefs, values, traditions and
practices of a person's culture, family structure and the roles
within the family in making decisions, health-related needs of
individuals, families, and communities, cultural beliefs about
health and etiology of diseases, cultural beliefs about healing
and disease treatments, and attitudes about seeking help from
health care providers.
The dominant American cultural paradigm is largely derived from
Anglo-American heritage and places high value on individualism,
privacy, personal responsibility and control. The "culture" of
healthcare in the U.S. reflects Anglo-American values, many of
which include being time oriented, focused on disease management
and treatment, and dedicated to preserving life at any cost. These
values are often in direct opposition of the values of many
traditional cultures, which often believe that fate, God or other
supernatural factors determines a person's destiny and directly
influences their health and family almost always includes extended
family, who commonly participate in the decision-making,
especially regarding health care.
When I was a dietetic intern, which means I had completed my
Bachelor's degree in nutrition but I was required to complete a
one-year internship and pass a national exam before I could use
the title of Registered Dietitian, I interned at a hospital where
about 70% of the patients were Vietnamese. I covered the cardiac
unit and the first nutrition education that I provided was with a
patient who primarily spoke Vietnamese and the nurse was our
translator as she was from Vietnam. The nurse was kind enough to
let me know that when giving dietary instructions it would be
perceived as disrespectful to give the instructions without the
family present. I agreed to return when the family was present,
which was a challenge as I felt I needed to "stay on schedule".
Like language, food
distinguishes one culture from another. A culture is strongly
identified with its foods, and it's food preferences will out last nearly any other
cultural practice. Afterall, what could be more culturally
defining and also unifying than diet? Persons of all cultures
today expect space to be made for their cultural norms, and
individuals who accept the United States as their new home,
although they may adopt U.S. portion sizes and fast-food culture,
typically maintain many of their own cultural food practices. In
order to positively impact the diet and health of a person or
family from another culture, one must understand their culture,
their communication style, values, and health beliefs. By
understanding these cultural aspects institutional food services
can work on including a variety of ethnic foods that are
reflective of their client base and nutrition counseling
interactions can incorporate familiar cultural foods.
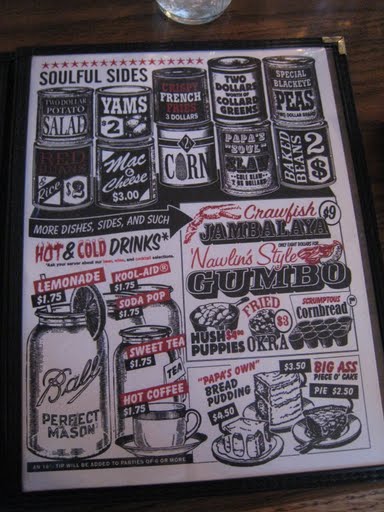
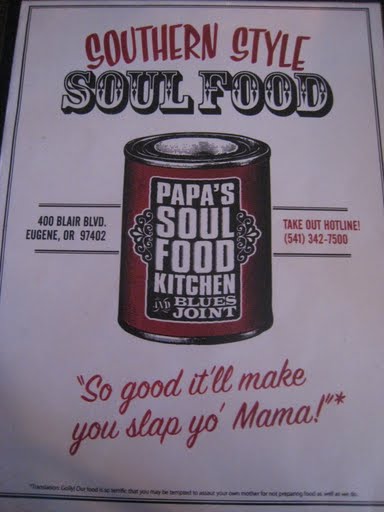
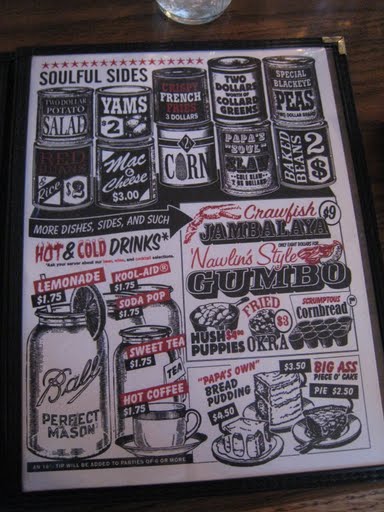
The images below were taken when I recently visited Papa's Soul
Food Kitchen BBQ in Eugene, OR. The menu included foods most
Americans would consider to be unique or strange, such as jerk
chicken, southern fried snapper, collard greens, black-eyed peas,
and sweet tea.
A good starting point for learning about cultural, ethnic and
religious food customs is to be able to access the nutritional
composition of many traditional foods.
A handy resource is the Oldways
website. The mission of Oldways is an
internationally-respected non-profit, changing the way people eat
through practical and positive programs grounded in science,
traditions, and delicious foods and drinks. It is best known for
developing consumer-friendly health-promotion tools, including the
well-known Mediterranean Diet
Pyramid.
The Asian Diet Pyramid, Mediterranean Diet Pyramid, Vegetarian
Pyramid, and the Native American Food Pyramid can be found at the
Food and Nutrition Information Center website (www.nal.usda.gov/fnic).
The packet will ask you a few questions that will require to check
out the Ethnic/Cultural Food Guide Pyramids.
- According to our textbook, Native North American Indian
Cuisine was not included in Tables 1.4, which starts on page 23,
because "the eating patterns of such a diverse group are not
easily categorized". However, the USDA has created a Native
American Food Pyramid. Why do you think it would be
challenging to create a Food Pyramid for Native North
Americans?
- Check out the Comparison
of
International Food Guide Pictorial Representations. What
was most interesting or surprising to you about these images?
(If
this link is problematic, feel free to check out ANY of the
ethnic or cultural pyramids provided.)
Starting next week, Week 2, you will work in groups to analyze
the nutritional status of an individual of a different racial,
ethnic, and/or religious group and life cycle stage. The cuisines
that will be discussed for each racial, ethnic, and/or religious
group will include the following:
- Vegetarian cuisine
- Food customs of religious cultures
- Native North American Indian cuisine
- Japanese cuisine
- Asian Indian cuisine
- Southeast Asian cuisine
- Chinese cuisine
- Soul food
- and potentially Caribbean cuisine
Based on what we've discussed about the importance of cultural
competence we all must continually seek out opportunities to
develop culturally competent skills. Some of the ways in which you
can do this are listed below:
- Explore the media. Read books, magazines, and newspaper
articles, and explore Web sites. Watch movies, videos and
television programs that pertain to other cultures and are
ideally targeted toward immigrant groups and non-native
speakers.
- Arrange cultural encounters. Attend fairs and religious
events. Go to restaurants and ethnic markets. Look for
opportunities to socialize with individuals from the target
culture.
- Take a walk down the grocery store's "ethnic foods" aisle
for a cursory lesson in diet diversity or visit local "ethnic
food" markets.
- Seek information on acceptable behaviors, courtesies,
customs, and expectations from a cultural expert that can help
you prepare for interactions and interpret actions.
- Walk or drive through communities to identify where
people gather, what types of stores and restaurants are
available, what is being advertised in windows, and how often
you hear the native language spoken.
- Visit community organizations to learn about a particular
cultural group, such as schools, block associations, senior
citizen's groups, and women's clubs.
- Many cultural groups have Web sites were you may find
chat rooms, advertisements, marriage brokers, lists of mail
order places for ethnic foods, and descriptive information
about food practices.
- Attend professional development and training classes or
group discussions.
- Take language lessons.
- Travel.
Below are a few images we took when we attended a
Japanese-American Lantern Festival in Eugene, Oregon.



One consequence of not attaining cultural competency can be seen
in the multitude of healthcare
disparities that exist in the United States. A healthcare
disparity occurs when a segment of the population bears a
disproportionate incidence of a health condition or illness. A
segment of the population can include gender, race, ethnicity,
education or income, disability, living in rural localities, or
sexual orientation.
In the U.S. there are four historically under-represented people
groups, African Americans, Native Americans/American Indians,
Latinos, and Asian Americans/Pacific Islanders. (Sound familiar to
the categories used in the most recent census?) In general, there
is a higher incidence of certain cancers, cardiovascular disease,
diabetes, obesity, and mortality in these population groups
compared to non-Hispanic whites.
The following list includes some of the most common causes of
healthcare disparities in the U.S.
- socioeconomic status (lower education and income levels)
- lack of insurance
- culture
- access to and utilization of quality health care services
- discrimination, racism, and/or stereotyping
- physical environment (e.g. housing conditions)
The following is an example of a healthcare disparity:
- English-proficient Hispanics were about 50% more likely
to report receiving advice on physical activity, as compared
with limited English-proficient Hispanics, after controlling
for health insurance coverage and number of visits to a
physician during the last year. Sex, age, region of residence,
level of education, annual family income, and smoking status
were not significantly associated with receiving physical
activity and/or dietary advice (Limited English Proficiency Is a Barrier to Receipt
of Advice about Physical Activity and Diet among Hispanics
with Chronic Diseases in the United States by
Lopez-Quintero C., Berry E.M., Neumark Y., JADA, October
2009, 109:10, Pages 1769-1774).
Unfortunately, in today's fast paced life the health care
system is not immune to time pressures. The Institute of Medicine,
in its report Unequal Treatment: Confronting Racial and
Ethnic Disparities in Health Care, cast a spotlight on
time pressure in the clinical setting to eliminate stereotyping
and other uncertainties that could have a negative effect on
quality of care. “In the process of care, health professionals
must come to judgments about patients’ conditions and make
decisions about treatment, often without complete and accurate
information. In most cases, they must do so under severe time
pressure and resource constraints... [leading to] those factors
identified by social psychologists as likely to produce negative
outcomes due to lack of information, to stereotypes, and to
biases.”
The Office of Minority Health of the US Department of Health and
Human Services (HHS), in conjunction with the Agency for
Healthcare Research and Quality, established National
Standards
on Culturally and Linguistically Appropriate Services
(CLAS), a collection of 14 mandates, guidelines, and
recommendations designed to eliminate racial and ethnic health
disparities. The idea behind the CLAS system is that better
communication leads to better adherence to medications and
lifestyle changes, which leads to improved health status, which
leads to less use of emergent care services and less frequent
hospitalizations.
Click on the CLAS link above to review the 14 mandates,
guidelines, and recommendations. Which one do you think will
be most helpful in eliminating racial and ethnic health
disparities and why?