Introduction to material about 5-6 minutes.

A therapist assesses a child readiness for higher level tasks
The SAID principle
The SAID principle stands for Specific Adaptations to Implied Demands (Holcomb, Baechle, & Earle, 2016. This applies to any human being regardless of ability or age.
Speaking in basic principles, our bodies will adapt specifically to the demands we place on it. So if you stress the body with aerobic based exercise, implied demand, it will compensate with adapting the cardiovascular system. Likewise, strength training will adapt with increased muscular strength and so on. According to this principle, doing cardiovascular exercise will not necessarily increase strength and increasing strength will not necessarily increase cardiovascular measures. This is a basic understanding and there is, obviously, carryover between systems as well as a difference in response depending on the type of cardiovascular and strength training. In general, you want to select exercises that are specific to your goals. Your body will learn to respond to the stress you place on it.
A child's way of getting stronger is through play. Stop-start activities are often the foundational and normative activities for young children in early elementary school.
In pre-adolescence, children are engaged in more skill based activities such as T-ball, softball, baseball, and soccer.
Pre-pubescent children can gain strength during activities, but muscles do not hypertrophy. It is important to note that the strength of boys and girls in pre-adolescence is essentially the same (Lloyd & Faigenbaum, 2016)
In puberty or adolescence, strength gains occur through resistance activity such as gym based activities that involve resistance. This is attributed in part to improvements in size of muscle mass and improvements in subsequent muscle force (Lloyd and Faigenbaum, 2016). Another very important factor in this strength and power gain in the development of the nervous system. Myelination is more complete at this time and the nervous system further develops improvement is seen in balance, agility, strength and power.
I have included some general resistance training guidelines for youth through the highly evidence based National Strengthening and Conditioning Association (2016). It is very important to note that most evidence of the benefits of resistance training are from adolescent and late adolescent youth. This is supported by the facts that growth hormones, and insulin-like growth factors and testosterone significantly increase during adolescence and late adolescence (2016).
Information I have provided is not prescriptive. Always work closely with you PT when working with children, especially as new graduates, before deciding to implement resistance training.
*children are NOT mini adults and should not be left alone to perform any resistance training.
- Before including any resistance training, understand human development. Is resistance training appropriate for the youth based on their age, the health condition and appropriate based on the pt and PT goals?
- Equipment needs to be appropriate in size for the youth, otherwise don't use it.
- When appropriate stretching exercises should be part of a warm up and a cool down for injury prevention and exercise performance.
- Begin with light loads to allow appropriate adjustments to be made.
- Increase resistance gradually 5% and 10% increments as strength improves and technique improves.
- Well trained professionals who are qualified and educated in child development should be the ones to supervise child exercise programs. Children should upon discharge be appropriately supervised by a trained adult when performing exercises and to assist as needed.
Best practice as new practitioners is to work closely with the PT when deciding what interventions/exercise are appropriate for youth.

A pubescent is ready for WC basketball
General Age Appropriate Exercise/Activity Specific Guidelines for Children
This is a good resource from Stanford University School of Children's Health that lists age specific exercises. Please use this list as a resource for your future work as PTA's and as you prepare for the licensure exam.
Intervention Goals
Goals for the pediatric client are restoring function. For kids with neuromuscular conditions, this may mean improving head control to allow for progression in sitting activities. In the musculoskeletal population, this may mean conditioning for return to sport after joint injury or concussion. In each case, impairment-only goals do not meet the rigor required in a PT plan of care.

A therapist works with a child in a custom chair
Many times it becomes apparent that what at one time appeared to be a relevant functional goal is no longer so, due to progressive development, changes in condition, or changes to family priorities. When this occurs, the goal should be revised to make it more applicable by the physical therapist. The PTA can suggest modifying goals as appropriate and give these suggestions to the PT.
Brief Discussion on Cerebral Palsy (CP)
Guided Learning to Goodman chapter on CP is below
Because of the fact that CP is the 2nd most common neurological impairment in children, I wanted to share a brief overview of this health condition. The most common neurological impairment affecting children is intellectual disabilities (Goodman, 2017).
The incidence of CP has been surprisingly stable (Goodman, 2017) even with more children being born pre-term. This is despite the correlation between pre-term and low birth weight children and CP. Any prenatal, perinatal, or postnatal condition that results in cerebral anoxia, hemorrhage or damage to the brain can cause CP.
CP is non-progressive. The motor impairments change with growth and maturity and may become more apparent as the child grows (Goodman, 2017). A short list of some of the associated impairments of children and adults with CP follow (Goodman, 2017). Of note presentation is variable. More milder forms of CP may have few of the following characteristics.
- Alterations of muscle tone: a significant number of children with a high tone spastic presentation of CP, present with hypotonia the 1st year of life and emerge with spasticity, hypertonia later.
- Delay in movement onset
- Difficulty timing muscle force or generation of poor muscle force.
- Difficulty or inability to maintain anti-gravity postural control
- Decreased speed of movement
- Increased muscle cocontraction
- Persistance of primitive reflexes which can affect head, neck, trunk, extremities and affects ADL's such as feeding, dressing.
- Variable cognitive impairments for some. Others no cognitive impairments.
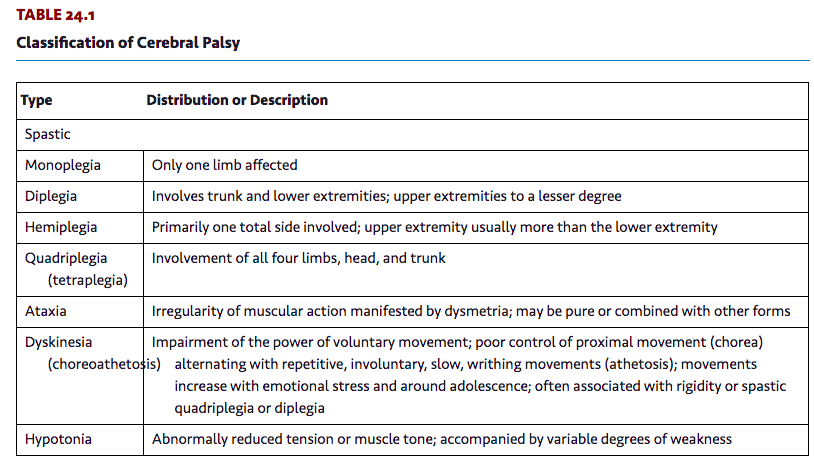
Below is from Goodman (2017) Table 24.1 that describes how presentations of CP are classified.
Intervention planning when working with children
The intervention plan is grounded in the ICF model, aiming for optimizing activity at home, school, and community. Interventions should be based on what is appropriate for both the child and the family. Interventions should always consider the related body structure and functions. If the injury is acute in nature (flare-up in arthritis, soft tissue shortening secondary to immobilization, torticolis, or an injury/surgery that requires gait training with an assistive device), then the PT plan of care will look very different from PT from a neuromuscular developmental disability (cerebral palsy, traumatic brain injury, Down syndrome, developmental delay).

A pediatric with trisomy syndrome as a health condition
For American children in the age range of birth to 3 years, pediatric physical therapy intervention may take place within early intervention. Services delivered in this way must be family-centered. Historically services were child-centered and mostly focused on the specific needs of the child. Family-centered service broadens the scope of the interventions and focuses therapy on the family and the child's position in the family. Therapists assume more of a coaching role, working with the child through the family.
Intervention should also be embedded in routines that already occur in the home or within the child's day. Thus lots of time and energy will be focused on teaching the family members how to handle, position, and interact with the child to get optimal performance from the child over the span of the day. Therapy goals are worked on throughout the entire day, not just at therapy-designated time. If a child needs to increase strength, then appropriate activities will be designed so that the child works on strength while participating in his or her regularly scheduled activities. Leg strength can be improved with squat-to-stand activities. If a container/toy is placed on a low table surface, and all of the pieces are on the floor, the child must repeatedly perform squat-to-stand activities to put all the pieces into the container. Likewise, if therapy is focusing on improved fine motor skills, pulling diaper wipes from a container will work on grasp-and-release movements. These are activities embedded in typically occurring routines. If the child needs to improve a gait pattern, the parent will be taught stretching activities that can occur at every diaper change, for instance. Ambulation can be built into going to check for mail at the box or cruising around the bedroom or kitchen. A child will be more inclined to cruise if furniture is placed close together to provide ready support.
Regardless of the child's impairment or pt or family goals, the therapist should use child sized equipment whether it is a medicine ball, elastic bands, dumbbells or barbells. The therapist needs to explain the why for the interventions and equipment used.
As the child enters school age, the focus of therapy may switch from a family-centered to an education-centered approach. Therapies delivered within an educational environment must focus on improving school performance. Therapy services outside the educational system may continue to be more child/family centered. For example, a 6-year-old child with diplegic cerebral palsy attends school. The child lives on the second floor of a two-story walkup building. There are no elevators in this building. The child has difficulty ambulating up the many steep steps to his apartment. His school is in a single-story building without steps. If the family wanted this child to improve his safety on the steps at the apartment, providing practice opportunities would be outside the mandates of the school therapist, since there are no steps in the school building. Thus the goal is not educationally relevant. However, the astute therapist will think about the child's participation in school activities outside of the building, such as ascending and descending the school bus steps or the playground equipment. In this way therapy could focus on stair climbing, which is important to the child's ability to be independent and safe both at home and within his educational environment. Additionally, the family may choose to engage the services of a community-based therapist to work on non education-based goals.
After the therapist, family, and child, if appropriate, have developed goals, the therapist should decide what intervention technique(s) may be most efficient and effective at helping the child meet the goals. There are several types of interventions and differing philosophies. In this chapter several of the interventions will be discussed. By no means is this an all-inclusive list or a ranking of the "best" interventions.
Intervention types
Common interventions include the following:
- Neurodevelopmental treatment (Bobath)
- Proprioceptive neuromuscular facilitation (Kabat, Knott, Voss)
- Conductive education (Peto)
- Strengthening and stability
- Therapeutic taping
- Sensory integration (Ayers)
The basis for all treatments must embrace in some form the dynamic systems model of motor control and motor learning. This model explains that all components of a child's world must be considered and will be influenced by all systems working in concert or conflict with each other. Physical therapist Fay Horak (2009) from Oregon Health Sciences University wrote that humans accomplish tasks using interacting systems that work together in an integrated fashion with shifting dominance. There are several physiologic systems, as well as environmental and cultural systems, to consider before determining the optimal intervention. If any component of any of these systems is not on target and not working in concert with the other systems, dysfunction will occur. It is up to the treating therapist to collect all the clues and decipher which component is not up to par, then determine if intervention focus should correct the malfunctioning component or assist the child and family to adapt and learn new strategies in order to function as independently and optimally as possible.
Guided Learning Insert Below is About 7-8 min
Comparison of Common Interventions
|
INTERVENTION |
PHILOSOPHY |
APPROPRIATE USE |
|
Neurodevelopmental treatment (NDT) |
Uses motor control to effect postural control and interactions between many neurologic and physiologic systems. Enhances the individual's capacity to function.
|
Children with cerebral palsy and motor disorders |
|
Proprioceptive neuromuscular facilitation (PNF) |
Strengthens muscle groups within diagonal and rotational movement patterns, based on developmental sequence and the sequential mastery of motor milestones.
|
Children with muscle imbalances |
|
Conductive education (CE) |
Views child as a whole child, using learning concepts, motor control/motor learning, and the group model to improve function. Learning movements and functional skills requires practice, intention, group motivation, and breaking down skills into task series. Uses specialized equipment to enhance child's orthofunction (ability to be functional and independent).
|
Children with CP, spina bifida, and other motor disorders |
|
Strengthening balance, gait and stability |
Improved function through improved strength, bone density, joint structures, muscle function, and management of obesity.
|
Children and infants with weakness and muscle imbalances which include but is not limited to Down's Syndrome, Duchenne's Muscular Dystrophy, Cerebral Palsy, Spina Bifida and developmental delays due to pre-term deliveries in some cases. |
|
Therapeutic taping |
Uses rigid or flexible taping to support and influence muscle groups. |
Children with muscle weakness, joint instability, joint malalignment, and postural asymmetries
|
|
Sensory integration (SI) |
Provides controlled sensory input to help children with sensory processing. |
Children with sensory processing dysfunction; children exhibiting dysfunction in ability to take in and process sensory information, organize behaviors and movements, or formulate/plan/and execute motor plans.
|
In addition to the physiologic systems, each child is influenced by environmental and cultural systems. Environmental systems include the child's primary living habitat, school or day care facility, neighborhood, and resources to function in these environments. Cultural systems include the family's traditions and beliefs, the extended families' traditions and beliefs (which may differ somewhat from the immediate family's), and known or perceived expectations of the child from society at large.
In order for an intervention plan to be successful, all the described systems that have an effect on a child must be continually assessed and monitored. Although a child may have a primary pathology or functional limitation, various influences from other systems may negatively affect the child and impact the primary impairment.
Neurodevelopmental Treatment
Neurodevelopmental treatment (NDT) originally was theorized by Berta and Carl Bobath (Pagliarulo, 2016). Since its inception in the late 1940s, the approach underwent a major shift of focus in the 1990s. Originally the approach focused on patterns of movement. Dysfunction of the movement patterns was thought to be caused by a loss of control from damaged higher centers in the brain. These lesions unleashed abnormal reflex activity. In the 1990s a shift from an orthopedic model to a biomechanical and systems model occurred. Current NDT theory embraces knowledge of motor control and looks at the effects of postural control as a result of interactions between many neurologic and physiologic systems.The overall goal of management and treatment, according to NDT theory and tenets, is to enhance the individual's capacity to function. Intervention involves a hands-on approach when working with individuals with central nervous system insults that create difficulties in controlling movements, with NDT embracing several general treatment principles:
- A child with cerebral palsy must be treated as a whole child with a whole personality.
- A good evaluation or assessment of the child must be completed.
- From the time of initial assessment, treatment programs should be customized to meet the needs of the individual child.
- The child's responses to treatment should be reassessed often.
- Realistic and reachable treatment goals are essential.
- Key points of control are used in treatment. Key points of control are parts of the body, typically proximally, where the therapist can apply light pressure to influence movement through the rest of the body.
- Teamwork is essential and must include the family.
In summary, pediatric NDT is primarily used to treat children with cerebral palsy and other movement disorders. However, aspects of the theory are applicable to many different clinical scenarios.
Proprioceptive Neuromuscular Facilitation
Proprioceptive neuromuscular facilitation (PNF) was developed in the early 1950s by Dr. Herman Kabat and Maggie Knott (Pagliarulo, 2016). The goal of PNF was to strengthen muscles within functional movement patterns rather than straight-plane or anatomic-plane motions. These movement patterns are known as diagonals. Physical therapist Dorothy Voss added many clinically relevant techniques to the PNF patterns. The theoretical basis for PNF rests within the hierarchical model of development. Hence PNF theory is based on the developmental sequence and the sequential mastery of motor milestones. You have learned basic PNF patterns for the lower quarter in PTA 132L as well as PNF stretches.
This is one demonstration of a PNF technique. Be prepared to learn more about PNF in 204 Lab. I recommend for those interested to be mentored by a PNF therapist or better, take a class in PNF specific to physical therapy and PNF.
Diagonal patterns can efficiently and effectively address specific problems of musculoskeletal weakness, and PNF is based on the principle that human beings respond in accordance with the demand placed upon the neuromusculoskeletal system. Two diagonals of motion exist for each major part of the body, and each diagonal is made up of two patterns that are antagonistic to each other. Each pattern has a component of flexion or extension. Each diagonal involves movement toward and across the midline or movement across and away from the midline and includes rotation with a flexion or extension pattern. When assessing the patient, PNF treatment protocols will look first at the patient's functional abilities. The identified stronger areas (agonist) will be used within the treatment session to assist the weaker areas (antagonist). Treatment movement patterns must be specific and directed toward a goal. Additionally, activity that will best develop coordination, strength, and endurance is necessary. Stronger body parts assist in strengthening weaker body parts though cooperation of muscle groups to achieve optimal function. For this reason PNF places great emphasis on using maximal resistance tolerated throughout the entire range of motion; by resisting stronger muscles, weaker muscles will receive overflow/reinforcement to help them become stronger and more coordinated. To initiate a movement, PNF technique may call for a stretch of the synergist. This provides the increased proprioceptive stimulation necessary to create a chain of muscle activity from a completely lengthened state to a completely shortened state, where the shortened muscle is the agonist.
In summary the PNF techniques work optimally in individuals with muscle imbalances secondary to spasticity, flaccidity, weakness, or pain. As a patient improves, coordination and balance activities can be added. Treatments tend to be intensive, using the patient's existing capabilities and skills without increasing pain or fatigue. The overall emphasis is on improving the person's function.
Conductive Education

Motor skills are needed for the task or activity of riding a bike
Conductive education was theorized by Andres Peto in 1948 in Budapest, Hungary. It is an integrated system that allows a child with motor dysfunction to learn to move within functional skills. Peto believed that children with motor disorders could learn to move by utilizing their brain's plasticity. He believed that learning movement required practice as well as rhythmic intention, so he based his technique on the educational principles of group learning and motivation .
Conductive education is based on four primary principles: a conductor, the group setting, rhythmic intention, and a specific task series for each functional skill. A conductor or a therapist trained in conductive education leads a session. The children attend in a group setting, with a typical ratio of 3 children to 1 adult. Skills are broken down into a series of tasks by the conductor. Children receive individual assistance as needed in order to complete the task at hand. The group of children practices each task until mastered, and then individual tasks are built into mastering skills. Rhythmic intention is the cadence set to time a movement or series of movements. Rhythmic intention allows children to replay the cadence and perform newly learned movements on their own. The cadence helps the child initiate a movement, sequence a movement, and complete the movement. Conductive education focuses on the functional skills a child needs to be optimally independent. This notion is also known as orthofunction. Motor learning and motor control principles come into play, and intensive amounts of practice time are part of conductive education programs.
Conductive education programs use specifically designed equipment that assists the child to perform a movement. Slatted plinths and benches allow the child to grasp between the slats for stability. Additionally, horizontal or vertical posts can be attached to table tops to provide anchors for children to use to stabilize themselves against gravity. Ladder-back standers and ladder-back chairs also provide graspable uprights to use while practicing ambulation. Conductive education programs in the United States are typically 3 to 4 hours per session, with sessions occurring 3 to 5 times per week. Given that generous amount of treatment time, there is wonderful opportunity to practice and use feedback and feed forward mechanisms to master a task and eventually master the skill.
In the United States the trend is to develop transdisciplinary or interdisciplinary teams to provide conductive education programs, using conductors and therapists working together. Some programs also use a hybrid system that allows the child to simultaneously attend their educational program (school) and a conductive education program.
Conductors, who until recently could only receive training in Europe or Hungary, can now earn a teaching certificate with an emphasis on conductive education pedagogy in the United States, and therapists in the United States can receive additional training in the pedagogy of conductive education and be certified as well.
In summary, conductive education is an intensive motor training program that uses motor learning and motor control principles, along with educational learning principles, to teach children with movement disorders to move to their highest potential. This leads to the child being as functional as possible. Conductive education is not appropriate for all children. However, many of the principles and tenets of conductive education can be used successfully with children who may not be eligible for an entire conductive education program.
Strengthening and Stability

Balls can be used to promote strengthening
and sensory input when used with children
Current theories in rehabilitation support the fundamental notion that children with motor impairments must work on strengthening and stability. There is strong evidence in the literature about the importance of strengthening for children with spasticity . Appropriate weight bearing through the long bones helps to maintain bone density and joint structure.
Exercise and strengthening are mandatory for a child with movement disorders to prevent overuse of the strong muscles, atrophy and wasting of weaker muscles, and obesity for children who cannot move as efficiently as their typically developing peers .
Different tools are used to help a child become stronger and more efficient. Appropriate use of a appropriate sized physioballs can be a tool to proximate core muscle strengthening in prone, sidelying, quadruped or supine. Various techniques may be used in addition to any of the other therapeutic techniques when working with a child and/or the child's family.
Therapeutic taping
Therapeutic taping is used to provide support or input to a muscle group. Flexible taping is also known as Kinesio taping, while rigid taping is known as Leukotaping or strapping.
Kinesio taping helps to support weakened muscles or prevent muscle overuse. Kinesio tape is flexible and has elastic properties. To strengthen a weakened muscle, the tape is applied from origin to insertion. To prevent cramping or over contraction of a muscle, tape should be applied from insertion to origin.
Leukotaping (named after Leuko sports tape) is rigid strapping used to support a joint in normal alignment. Muscle facilitation for appropriate firing can be achieved by laying the tape parallel to the muscle fibers. Similarly muscles can be inhibited by laying the tape perpendicular to the muscle fibers. Over time it has been demonstrated that bony remodeling can occur with appropriate and consistent rigid taping.
TheraTogs (2016) is an orthotic product designed to capture the benefits achieved with taping without directly adhering to the skin. The client wears a vest and shorts made of a neoprene-type material. With additional arm and leg cuffs, flexible or rigid straps can be added to the suit to facilitate or inhibit movements. TheraTogs are easy to don and doff, should be worn directly next to the skin, and easily fit under typical street clothes and diapers. The TheraTogs provide consistent input, essentially where a therapist would provide manual input for the child, in the absence of handling the child.
Sensory Integration
Sensory integration therapy assists the child by using controlled sensory input to help children with sensory processing difficulties.It is a theory of brain-behavior relationships.The theory has three major components: normal sensory function, sensory integration dysfunction, and a programmatic guide for using sensory integration techniques. Ayers felt that learning is dependent on the person's ability to take in and process sensory information from the environment and self-movements, then organize behavior and movements in response to these inputs. If an individual has difficulty integrating and processing, the result will be deficits in planning and executing movements and in motor learning. To remedy this dysfunction in motor learning, intervention within a meaningful context must occur to improve the ability of the central nervous system to process and integrate sensory inputs.
In summary, sensory integration treatment encapsulates three areas: the theory, the evaluation, and the treatment. Each is vital in treating the child. A clinician can receive additional training in sensory integration theory and treatments.