Asthma and Pediatrics
Pathology - Key Points
Guided Learning to Material Below 6.5 minutes
Week 5 content includes content in obstructive lung diseases, such as asthma. This lecture expects you to be able to apply your knowledge of conditions and consider environmental and personal factors that influence activity and activity tolerance in children with asthma
Asthma attacks are generally recurring episodes, and by definition airway obstruction is reversible. Key points specific for pediatrics include:
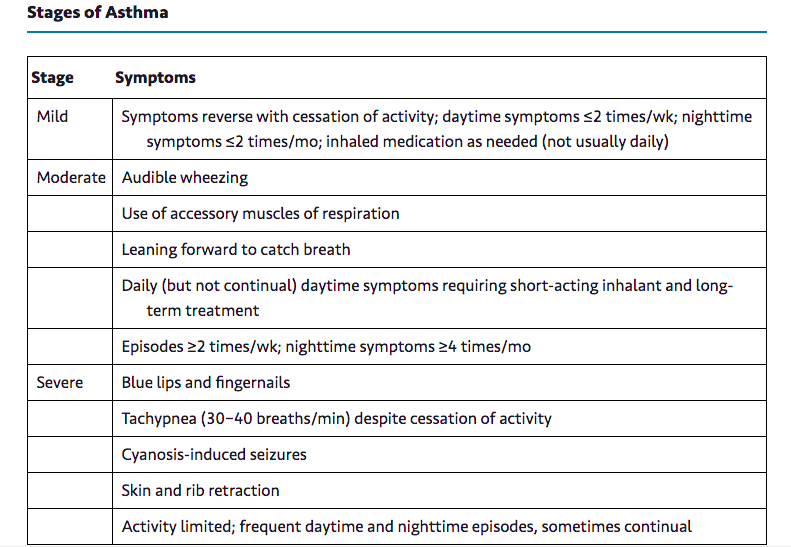
- Asthma episodes are classified as mild, moderate, and severe, because the degree to which a person reacts to a trigger varies.
- Often there are triggers that cause an asthma sufferer's airways to react by swelling, closing down,and producing excess mucus.
- Triggers include physical activity, allergens such as pollen or pet dander, irritants such as chemicals or smoke, and respiratory coughs or colds.
Zitelli BJ, & Davis HW, 2007.
- Asthma rates continue to increase all over the world and in the United States during the past decade. According to the Centers for Disease Control and Prevention (CDC, 2016), more than 6 million children under age 18 in the United States have asthma, making it one of the most common chronic health conditions of childhood.
- Racial and economic disparities are apparent in both the number of hospital and emergency room visits attributable to asthma and deaths from asthma (Goodman, 2017). Children of color in low-income neighborhoods have shown the highest increase in rates of asthma in recent years, perhaps related to both indoor and outdoor air pollution. Rates of asthma for children of color are double that of white children. Children in urban areas are more at risk for developing asthma.
- Children with lower birth rates - less than 5.5# and more than 3 weeks pre-mature are more susceptible to the effects of air pollution compared to children who are full term (Goodman, 2017). It is estimated that asthma goes unrecognized as an adverse factor affecting performance in 1/10 adolescent athletes.
- A study by Mount Sinai Medical Center in New York City showed that emergency room visits for asthma varied dramatically by zip code, with the number of visits much higher in poor areas having large minority populations. Spanish Harlem had 223 visits for every 10,000 residents, while some parts of more affluent lower Manhattan did not record any emergency room visits (CDC, 2012).
- The CDC (2016) reports that emergency room and hospitalization rates for asthma are higher for black children than for white children, particularly for those under age 5. Among non Hispanic black and white children aged 5 to 14, black children are five times more likely to die from asthma than white children.
- There is a relationship between obesity and asthma. The higher the BMI the greater the risk of developing asthma (Goodman, 2017). One study demonstrated reduced respiratory function in 32% of obese children versus 3% of children with a normal BMI.
Bronchial Asthma Clinical Signs (Goodman, 2017)
- Cough can be hacking, exhausting, irritative, involuntary, non productive.
- Cough can be rattling and productive with frothy, clear, gelatinous sputum
- Paroxysmal breathing
- Audible wheeze
- Shortness of breath, may occur at rest.
- Respiration: prolonged expiration.
- Barrel chest in chronic asthma
- Elevated shoulders and use of accessory muscles of respiration.
- Airway inflammation, obstruction, or hypersensitivity to extrinsic and intrinsic stimuli
As a PTA you may observe a child using accessory muscles in the ribcage to breathe; in this instance, the child may appear winded. It is important to note that symptoms vary. During remission all pulmonary tests are normal (Goodman, 2017). However reported attacks may cause pulmonary remodeling chronic air trapping, proliferation of submucosal glands and hypertrophied smooth muscle. Overtime these changes may become irreversible and result in COPD.
Below is from Goodman, 2017 Table 11.8. It is a good reference for when you work with children/patient's with asthma.
Physical Therapy Assessment
After a review of the child's medical history, physical therapy evaluation should focus on identifying any areas of impairment, functional limitations, and activity and participation limitations. Examples of considerations in evaluation include:
| FUNCTIONAL ACTIVITY |
SECONDARY PROBLEMS |
|---|---|
|
Breathing |
Inadequate breath support and inefficient trunk muscle recruitment at rest or with activities, such that breathing or postural control are compromised. Asthmatic triggers such as rapid air flow caused by sudden increase in physical activity, dry air,extreme temperatures, or other triggers that trip an asthmatic reaction |
|
Coughing |
Ineffective mobilization and expectoration strategies |
|
Sleeping |
Breathing difficulties, signs of obstructive or central sleep disorders Nocturnal reflux (GERD) |
|
Eating |
Swallowing dysfunction Reflux (GERD) Dehydration Poor nutrition |
|
Talking |
Inadequate lung volume and/or inadequate motor control for eccentric and concentric expiratory patterns of speech Poor coordination between talking (refined breath support) and moving (postural control) |
|
Moving |
Inadequate balance between ventilation and postural demands Breath holding with more demanding postures: use of the diaphragm as a primary postural muscle for trunk stabilization Inadequate lung volume to support movement Inadequate and/or inefficient muscle recruitment patterns for trunk/respiratory muscles, causing endurance problems or poor motor performance Ineffective pairing of breathing with movement, especially with higher-level activities
|
|
From Campbell SK, Vander Linden DW, Palisano RJ: Physical therapy for children, ed 3, Saunders. Philadelphia Note: These activities require adequate lung volumes and coordination of breathing with movement for optimal performance.Ty pical secondary problems associated with asthma should be screened for to determine their possible contribution to the child's motor impairment or motor dysfunction. |
|
Preparing for safe treatment

Image above are examples of various devices that may be used by those with the health condition asthma
Physical therapy intervention of asthma comprises both short-term (medical needs and musculoskeletal restrictions) and long-term (reducing secondary impairments, usually through an established exercise regimen) goals
In caring for children with asthma it is imperative to have their diagnosis and asthma management plan on hand. Anyone involved with the child's care should be ;well-instructed in signs and symptoms of asthma as well as how and when to administer asthma medications or call for emergency help if needed. An individualized asthma management plan includes the child's asthma history, triggers and symptoms, ways to contact the parent/guardian and healthcare provider, physician and parent/guardian signatures, the child's target peak flow reading, and a list of current asthma medications. The plan will also include the child's treatment plan for medications, based on symptoms and peak flow readings.
Peak Flow Monitoring
Peak flow monitoring can be effectively used in children age 5 and older. There are many different peak flow meters available on the market. The simple device measures how well air is moving out of a person's air ways. To use the device, one takes a deep breath in, places the mouth on the peak flow meter, and exhales as fast and completely as possible. A reading will appear on the meter. Usually the steps are repeated a few times to ensure accuracy. Each person who uses peak flow monitoring has a personal best or target reading. Lower numbers may call for attention with medications and additional monitoring. Very low numbers demand emergency attention. Peak flow numbers or zones should be included in the asthma management plan. Though quite effective, peak flow monitoring is only one indicator of asthma stability or problems. Other symptoms such as coughing, wheezing, complaints of shortness of breath, and chest tightness should also be considered.
Medications
Major drug classifications include bronchodilators, corticosteroids and combined beta-agonist/corticosteroids.
Asthma may be treated and controlled with a variety of pharmacological interventions. Many patients have at least two types of medications.
The first type is used as a preventive or maintenance medication. Preventive medications can be oral or inhaled and are used to help decrease the inflammation of the airways or decrease the response to triggers such as allergens. Combined beta-agonist/corticosteroids are preventative
The second is a rescue medication. Rescue medications are usually supplied in the form of an inhaler that contains a bronchodilator such as albuterol.
Albuterol quickly helps to open the airways,enabling an asthmatic to breathe easier. It is important to distinguish between the two types of medications. A preventive inhaler will be of no help during an acute asthma attack.
Children with asthma should also keep extra rescue inhalers at school and at any caregivers' homes.
Spacers
- A spacer is a large chamber that is fitted to an inhaler and is useful in dispensing a dose of medication more effectively.
- Spacers serve to increase the amount of medication that actually reaches the lungs, instead of being deposited in the mouth and throat.
- For children there is the added advantage of not having to coordinate the inhalation of medication, as they must with a multi-dose inhaler.
- The medication dose is released into the spacer and then can be inhaled at will by the child.
- In the event that the lung tidal volume is low and inhalation is difficult, he or she can breathe in and out several times with the chamber and still get an effective dose.
- Caution must be used to avoid spraying more than one puff at a time into the spacer.
- If the child's dose is two puffs, spray one and have the child inhale from the spacer, then repeat with the second puff after waiting 1 full minute.
It is vital for caregivers to be able to identify when a child is having difficulty breathing or having an acute episode. Activity should be stopped when these symptoms are noticed. If a child has an asthma management plan, instructions with regard to medications should be closely followed. If the child does not respond to medications or fails to improve,emergency help should be sought.
Signs and Symptoms of Emergency
If a child is hunched over, straining to breathe, has difficulty completing a sentence, looks ashen or has blue lips and fingernails, immediate emergency help (i.e., a 9-1-1 call) is warranted.
Exercise-induced asthma
Exercise-induced asthma is a special consideration. Children and caregivers can try to ;reduce triggers like allergens and irritants, but exercise should not be avoided to avert an asthma attack. Rather, with medications and possibly some modifications to physical activity, he symptoms can be controlled. Often a physician ;will recommend giving a dose of rescue medication prior to exercise to decrease the child's chances of having an acute asthma episode. This can be very effective. In addition, a child who has had a recent asthma episode is more likely to have additional episodes, and therefore the level of exertion should be modified.The physical therapies assistant can create an individualized exercise regimen that will improve muscle function while minimizing the risk of an asthma attack.
Exercising indoors or in a warm, humid environment rather than outdoors or in a cold, dry environment can reduce the frequency of asthma attacks. Recent research has determined that weather factors, pollen, and the different seasons have an effect on the severity of asthma symptoms.
- High temperature and barometric pressure were the most highly correlated weather factors with severity of asthma symptoms
- .Additionally, airborne irritants such as pollen and mold also correlated with asthma symptoms.
- .In most of the subjects, summer was the least difficult season for asthmatics, followed by spring; fall was the worst, followed by winter
- This research is important to the PT and PTA when designing exercise protocols for asthmatics or for the PT and PTA who work in schools.
- Be mindful when working with asthmatics that certain warm days with high barometric pressure, allergy-alert days when the airborne irritant count is high, and the fall season are specific times when healthcare providers must be keenly aware of the status of children with asthma.
General considerations for asthma including interventions such as exercise.
- Design an exercise protocol that includes no asthmatic triggers with education to patient and family member if a juvenile, on how to modify an exercise if a trigger occurs while exercising.
- Make sure exercises are to be carried out in a fun, but safe way being aware that promoting a walking program may not be safe for a child if the child lives in a neighborhood that is violent.
- Goodman (2017) has come excellent exercise guidelines for children with asthma below. Please study these guidelines as you are likely to work with children with asthma, and adults with asthma.
Exercise Guidelines for Children with Asthma

- Implement low-cost measures for indoor allergen avoidance
- Restore, maintain, and promote optimal physical functioning
Goodman, 2017) summarizes the implications regarding asthma and PTA on age 386. Pay special attention to the fact that there are many barriers to exercise as cited earlier in this section on asthma. Certainly weather, and a misguided belief that exercise is not good for this condition. I recall a peer of mine who refused to exercise because of this fear and that exercise would trigger his asthma so he never attempted exercise. There is strong evidence to support physical training for this population particularly cardiovascular training although this study was likely specific to adults (Goodman, 2017). On a related note, there is limited evidence to support breathing exercises and inspiratory muscle training for this population: again, the study was likely on adult subjects.
Obesity can contribute to the associative inflammatory process associated with asthma and exercise and education about the benefit of exercise should be part of any treatment plan (Goodman, 2017).
Swimming is beneficial for those with exercise induced asthma, even long distance swimming (Goodman, 2017). Because the air is fully saturated with moisture near water, exercise is well tolerated. Because expiration breathing underwater by swimmers is essentially pursed lip, this prolonged underwater expiratory breathing increases end-expiratory pressure within the respiratory system.
Application Brainstorm: A Summary of this Lesson Builder
- How can a child practice standing and weight shifting while in the family's kitchen/food preparation area?
- What are the benefit of including typically developing peers within a treatment session?
- What effects do therapeutic garments have on facilitating strengthening and stability in the pediatric population?
- Can you name two triggers that may affect an asthmatic child's ability to breathe.
- What racial and economic groups demonstrate the highest rate of childhood asthma?
- What are the components of an asthma management plan?
- What is the purpose of the peak flow meter?
- Is it better to have a high reading or a low reading on the peak flow meter?
- What is the difference between preventive medication and rescue medication?
- What are two accommodations that children with asthma may make in order to participate in an exercise routine/activity?
- What are three common signs or symptoms of an asthma attack?
- What is the appropriate action to take if a child begins to have an asthma attack while exercising?
- What weather-related factors and season seem to correlate with the severity of asthma symptoms?
- How do exercise methods to improve muscle performance vary between early childhood and adolescents?
- What is an example of applying the SAID principle to a therapeutic exercise intervention in the pediatric population?
References
Campbell SK, Vander Linden DW, Palisano RJ: 2006. Physical therapy for children, 3rd Ed. Saunders, Philadelphia
Centers for Disease and Control, 2012. Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States, 2001–2010. Available at: http://www.cdc.gov/nchs/data/series/sr_03/sr03_035.pdf#x2013;2010 [PDF - 910 KB]
Centers for Disease and Control. 2016. Asthma and Children. Available at:
https://www.cdc.gov/vitalsigns/childhood-asthma/
Goodman. C. 2017. Introduction to Pathology for the PTA. Elsevier. MO
Holcomb, W. R., Baechle, T. R., & Earle, R. W. (2016). Essentials of strength training and conditioning. 4th Edition. Champaign, IL: Human Kinetics.
Lloyd. R and Feigenbaum. A. (2016) Age and Sex Related Differences and Their Implications for Resistance Exercise. Essentials of strength training and conditioning. 4th Edition. Champaign, IL: Human Kinetics.
O'Shea, R. K. (2009). Pediatrics for the Physical Therapist Assistant.1st Ed. Saunders Elsevier, IL.
Pagliarulo. M. 2016. Introduction to Physical Therapy 5th Edition. Elsevier. MO.
Stanford Childrens Health. 2021. Aerobic Exercise for Kids. Available at:
https://www.stanfordchildrens.org/en/topic/default?id=aerobic-exercises-for-kids-1-4800Zitelli BJ, Davis HW: 2007. Atlas of Pediatric Physical Diagnosis, Ed # 5, Philadelphia, Mosby.