Iontophoresis
"ionto" refers to ions - positive and negatively charged particles
"phoresis" refers to one organism or compound assisting the transport of another organism or compound"
So - iontophoresis describes a process of passive and active transport of ions across the skin.
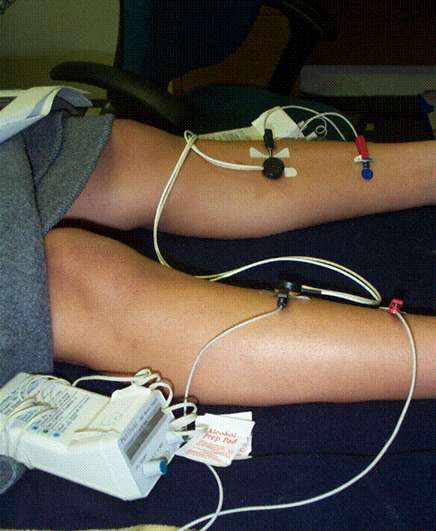
Iontophoresis adds energy, using direct current, to transport ionized medication across the skin and into underlying target tissue.
How Iontophoresis Works
It's Coulomb's Law! Small amounts of current help overcome skin impedance, and medication is delivered based on:
- The repulsive effects between the medication and the active electrode.
- Increased skin permeability as a result of the charge
- Movement of water and sodium (Na+) toward the cathode (negative pole)
Applying a charge to the skin changes the flow of ions through the skin, reducing it's resistance and enhancing the amount of and type of medication that can travel below the skin's surface to produce a therapeutic dosing effect.
A systematic review of iontophoresis in the treatment of lateral epicondylitis (tennis elbow) indicates low to moderate evidence in support: McKivigan, J. M., Yamashita, B., & Smith, D. (2017). A Systematic Review on the Efficacy of Iontophoresis as a Treatment for Lateral Epicondylitis. Research & Investigations in Sports Medicine, 1(3), Article-RISM.
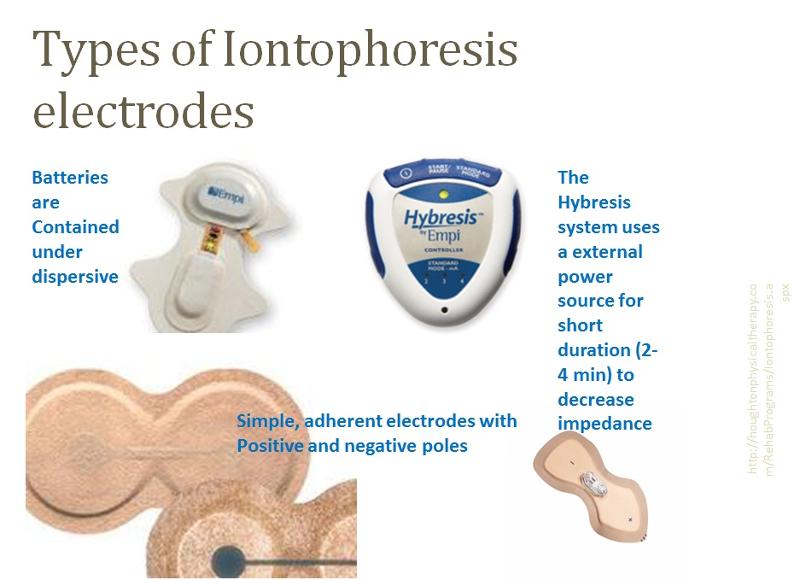
What Iontophoresors Look Like
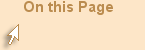
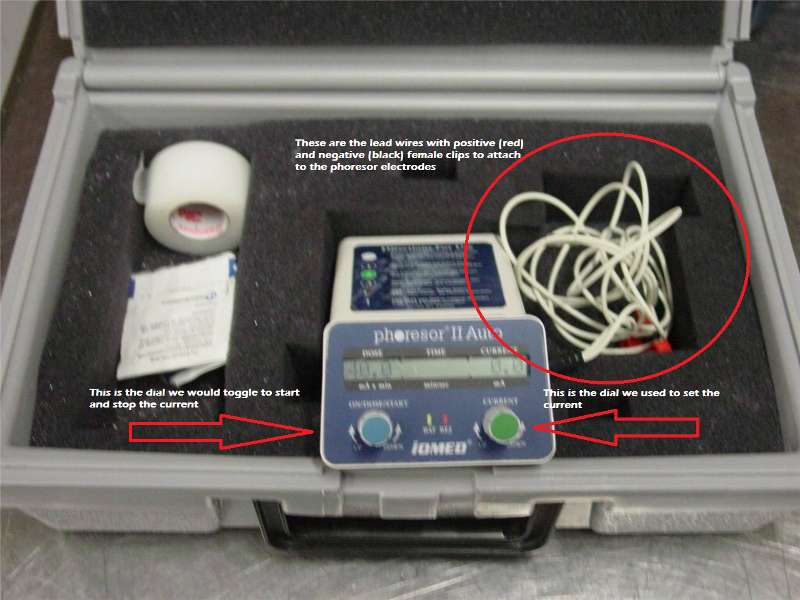
Back when I was in PT school, phoresors were electrical devices called phoresors (see image below), powered with a 9V battery, with clip-on leads to be placed on the electrode. Current was administered using two electrodes.
One electrode was filled with the medication. This is the active electrode, and one carbon adhesive electrode as the dispersive electrode.
The clinician set the amount of direct current, in milliamperes (mA) applied by the phoresor to the active electrode. The phoresor would calculate the treatment time to achieve a 40mA - min dose.
For example, if the patient comfortably receive 4mA of direct current, then the treatment would last 10 min (4mA x 10 min = 40mA - min). The challenge is that patients have varying sensitivities to current and varying nutritional and skin status, so when current is reduced for patient comfort, treatment times are longer (40mA - min dose at 2.0mA is now a 20 min treatment).
Most transdermal medication delivery by iontophoresis is simplified so that the source of current comes from the patch. These are called "wear-home" patches and the electrocircuitry is self-contained and can deliver medication over as long as a 24 hour period
A patch containing a positive and negative electrode adheres directly to the skin. One end of the electrode is filled with the selected medication, and the other is filled with standard saline (NaCl).
Patches contain a buffering agent that minimize the chances of a burn
Electrode configurations and shapes vary. This allows for good skin contact around surfaces. Patches are also designed to deliver different medication doses (e.g., there are 40mA-min, 60mA-min, and 80mA-min electrodes).
Medication and Treatment Times
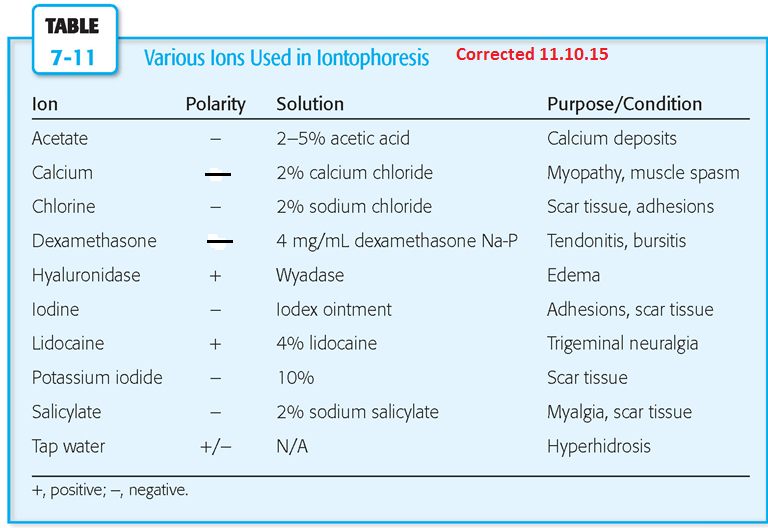
Key points - know the polarity of the drug or ion used and make sure there is good electrode contact with the skin to prevent skin injury
Drug selection is based on the intended effect in the tissue: anti-inflammatories, analgesics (pain medication), muscle relaxants, and sclerolytics (scar reducing) are all examples of common drug descriptions that may be delivered by iontophoresis
Medication dosages are based on drug properties. Typical dosages range from 40mA-min to 80 mA-min
Current density is the ratio of current (mA) to electrode surface area (cm2). Most electrodes are manufactured to be consistent with 0.5 mA/cm2 current density at the the cathode (negative pole)
Treatment time will depend on the electrode properties and method of introducing current (e.g., commercial unit vs. self-contained patch, vs. Hybresis)
General application procedures
•Identify treatment area
•Usually by palpation, depth of treatment is shallow
•Check skin for abrasions
•Clean with alcohol
•Fill appropriate electrode with medication (e.g., dexamethasone is (-), so would be filled on electrode identified as (-)
•Fill opposite electrode with normal saline
•Apply to skin, securing electrode by taking care to press only the edges of patch
•Depending on delivery method, introduce low current and calculate treatment time as needed based on targeted dose
Patient Safety with Iontophoresis
- Know the charge of the medication that has been selected for the patient
- Inspect the skin for any signs of compromise
- Screen the patient for prior medication or adhesive sensitivities
- Confirm the therapeutic dose for the medication (noted as mA - min)
- pH changes in the skin do occur with iontophoresis. The movement of Na+ and Cl- ions can change local protein density and can lead to electrical burns.
- Monitor patient skin and educate patient on possible minor skin irritations following treatment (itching, mild redness or dryness)
- PT Aides in Oregon may not dispense iontophoresis
Adverse Reactions with Iontophoresis
- First-degree burns
- Persisting, transient erythema at drug delivery electrode
- Sensations of burning, tingling, pulling or other dysethesias (abnormal sensations) at the electrode site
Role of the PTA
- Confirm the PT has included iontophoresis, and approved medication, in the plan of care
- Confirm the medication dose
- Check skin, inform patient of expectations, modify for comfort, discontinue if painful
- Document dosage, location, medication, consent
- Follow-up with patient next visit regarding treatment effects, check skin integrity