Impairment-Based Classification Considerations
Spine classification may guide recommendations for bracing. A wide variety of orthotic designs, ranging from lumbosacral corsets to rigid thermoplastic thoracolumbosacral orthoses (TLSOs), may be prescribed to appropriate position the spine for protection and pain relief. For example:
|
Condition |
Orthoses type |
Orthosis position |
|---|---|---|
|
Non-specific mechanical low back pain |
LSO |
typically positions lumbar spine in extension promotes lordosis |
|
Discogenic Extension-bias |
TLSO LSO Knight LSO
|
typically oriented toward lumbar spine in extension promotes lordosis
|
|
Stenosis Spondylolisthesis Flexion-bias Non-weightbearing bias |
LSO Williams LSO
|
typically oriented toward lumbar spine in flexion
|
|
Fracture Instability (traumatic and non-traumatic) |
Halo CTLSO Rigid external collar |
immobilizes specific levels and specific planes of movement. |
Note: Although the trade name type (e.g., Williams) is typically associated with a position, the role of the PTA is to understand that the position of bias is a position of ease, and to coordinate brace selection and use based on the desired outcome and within the plan of care.
Practical Applications
Active Learning Exercise
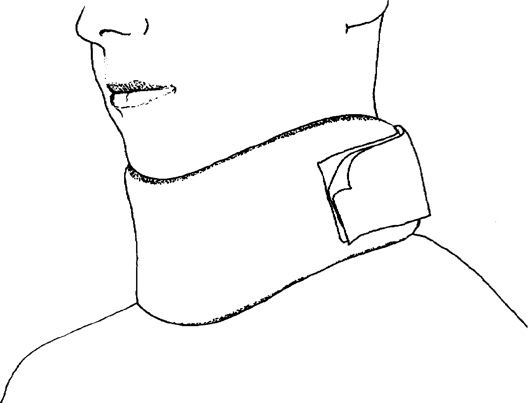
For your exam, you will be asked to identify how the structural components in selected orthotics reduce risk for reinjury and affect spine motion. Careful observation of orthoses components can often indicate which structures are receiving the greatest amount of stabilization. For example, by looking at this image, you should be able to classify it (rigid vs. soft, general level(s) of spine affected by bracing): 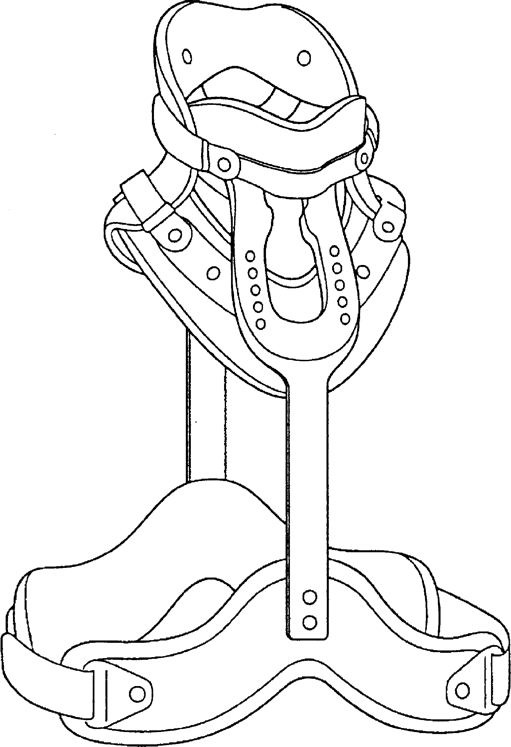
Take a look at this CTO and write down the points of contact for the rigid structures: 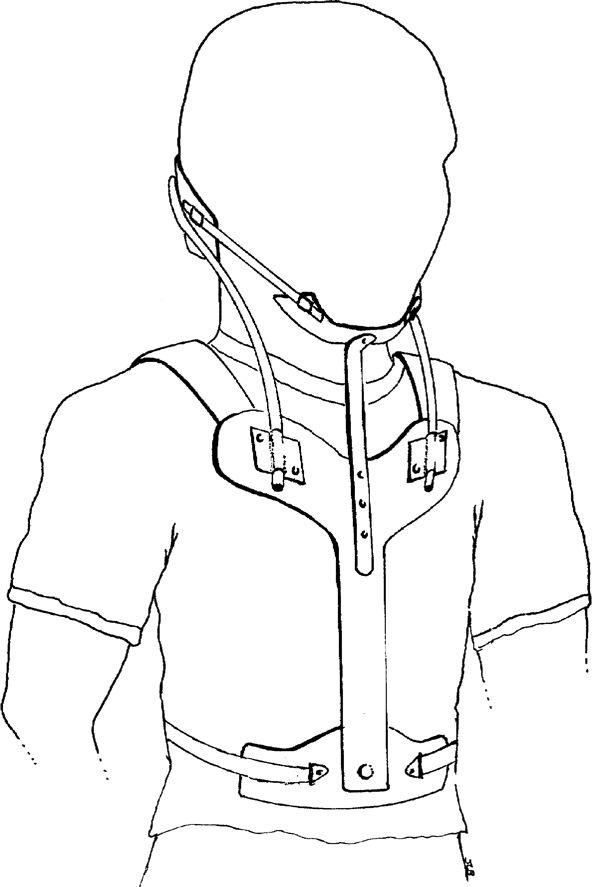 Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?
Note the 'U' Shaped rod which connects the occiput to the R and L sides of the sternum. If tension was released in the 'U' rod, what limited motion(s) would become available? Based on the points of contact, do you suspect an upper cervical or lower cervical instability? What areas will you check for skin breakdown? What would be your primary indicator of signs/symptoms of misfit?
Halo Jackets
A halo vest/jacket is the only orthosis which completely limits cervical motion in all three planes. It can be used conservatively or post-operatively to insure adequate healing time for cervical stabilization.
Wear time for a halo jacket is typically 12 weeks, depending on bone healing. Driving while wearing a halo is illegal.
The head is stabilized by pressure pins inserted 1/8" into the skull above the lateral 1/3rd of the eyebrow and just posterior to the ear. Halo jackets typically weigh 5-8 poiunds.
Pins may also loosen over time, shifting out of the skull or into dural tissue, so close monitoring for fit and excessive motion is important.
PT/PTAs are involved in inspecting pin sites for signs and symptoms of infection and reporting findings to appropriate medical personnel and teaching log roll technique for transfers out of bed. . 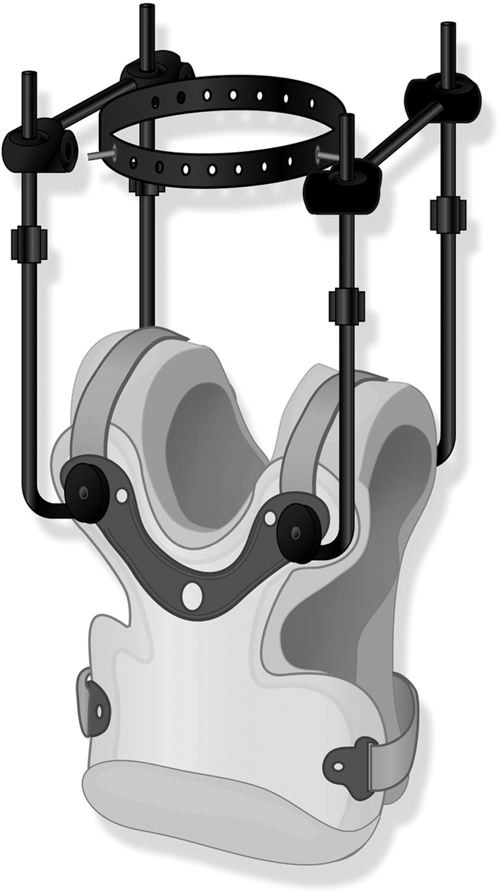
NEVER PULL ON THE HALO JACKET OR USE IT AS A POINT OF MANUAL CONTACT DURING FUNCTIONAL MOBILITY TRAINING. The anterior component of the jacket can be removed in supine for hygiene and for emergency medical procedures.
Scoliosis
Custom molded or 4 point rigid orthoses may be used to prevent progression of scoliosis. Research supports regular checking of fit and tension in the orthotic straps in order to prevent and/or reduce scoliosis progression (Wong, et al., 2000)
In a five year longitudinal study of 158 adults diagnosed with scoliosis, 80% saw increased spinal stability and improvements in curve measurements as a result of bracing (de Mauroy et al., 2016). In a systematic review of the literature, there is stronger evidence that bracing minimizes and slows scoliosis progression (Dunn et al., 2018).
Effective wear time ranges from 18-23 hours/day. In some cases where compliance is an issue, effects can be acheived through a night time wear schedule.
Your text provides examples of orthoses used in scoliosis management.
This six-minute video provides a patient perspective on using a brace for scoliosis management
de Mauroy, J. C., Lecante, C., Barral, F., & Pourret, S. (2016). Prospective study of 158 adult scoliosis treated by a bivalve polyethylene overlapping brace and reviewed at least 5 years after brace fitting. Scoliosis and spinal disorders, 11(2), 28.
Dunn, J., Henrikson, N. B., Morrison, C. C., Blasi, P. R., Nguyen, M., & Lin, J. S. (2018). Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US Preventive Services Task Force. JAMA, 319(2), 173-187.
Wong, M. S., Mak, A. F. T., Luk, K. D. K., Evans, J. H., & Brown, B. (2000). Effectiveness and biomechanics of spinal orthoses in the treatment of adolescent idiopathic scoliosis (AIS). Prosthetics and orthotics international, 24(2), 148-162.