Anatomy and Physiology
The anatomy of the respiratory system will be a review of content from your A&P coursework and Pagliarulo from fall term.
Reading and Web Exploration
- Cameron & Monroe, pp. 398-406
- "What do the lungs do"
Respiration and Ventilation
Breathing is an automatic action coordinated by the nervous system, the musculoskeletal system, and the anatomical structures that comprise the airways. Impairments that arise when their are dysfunctions within one or more of these systems can result in decreased endurance, decreased strength, postural abnormalities, and impaired airway clearance. When respiration or ventilation is impaired, a patient will work to generate compensatory strategies to maintain breathing function.
Why is an understanding of anatomy critical to optimizing ventilation and respiration? As we move forward in the lecture, we will be connecting anatomy and physiology to the basis for the interventions. For example, positioning for postural drainage requires that a PTA can integrate knowledge of lung lobes and respective airways and gravity to passively improve airway clearance, and therefore decrease muscular efforts and improve gas exchange. Although breathing is largely under autonomic control, PTs and PTAs take advantage of volitional breathing patterns and pathways to help patients and clients optimize respiration and ventilation.
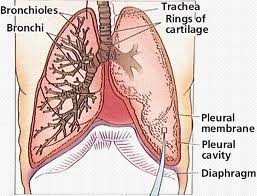
As you refresh your knowledge of anatomy and breathing mechanics, start thinking about how each structure, such as the rib cage, intercostals, and respiratory zones play an essential role in breathing:
- skeletal components
- muscular components
- Primary breathing mm - diaphragm
- Accessory mm
- Internal intercostals - forced expiration
- lungs and airways
Respiration: "Respiration is the process of exchange of gases between the atmosphere and the tissues"
Ventilation: "Ventilation refers to the movement of a volume of air from the atmosphere in and out of the airways and is highly dependent on the ability of the respiratory muscles to generate force to bring air into the lungs"
Note the number of medical diagnoses (Cameron & Monroe, Box 26-1) that are associated with breathing impairments. In addition to COPD, neuromuscular disorders, infections, and musculoskeletal conditions, such as scoliosis, can present with breathing impairments as a primary contributor to disability. Can you see why a strong foundation of anatomy, physiology, and pathophysiology can improve patient outcomes in airway clearance, posture, and endurance?
Neural Control of Breathing
The take home message for PTs/PTAs is that abnormal level of O2 and CO2 trigger a change in respiration rate, effort, efficiency, perfusion, and overall function.
- Voluntary and involuntary neural control
- Chemoreceptors - these work to balance concentrations of oxygen (O2) and carbon dioxide (CO2) for optimal gas exchange
- Hypercapnia: High C02, high acidity, low pH: .
- As C02 increases, respiratory rate (RR) increases to remove C02
- Hypoxia: Low 02 detected by the receptors in larger proximal blood vessels triggers increase RR
- Mechanoreceptors
- stretch responses in skeletal muscle and related tissue can trigger increased ventilation
- ANS
- Vagus nerve (Cranial nerve X), associated cranial nerves associated with ventilation muscles are influenced by sympathetic and parasympathetic pathways
- Motor cortex allows use to voluntarily control of our own breathing. Everyday examples include:
- Blowing out birthday candles
- Blowing up and balloon
- Holding breath in and out of water
