Spine Conditions
The following provides an overview of signs and symptoms primarily associated with cervical and lumbar conditions
12 minute video
Radiculopathy
- Spinal nerve / nerve root conduction is impeded due to "encroachment into peripheral nerve tissue spaces resulting in nerve compression or ischemia";
- encroachment can be classified as direct or indirect, mechanical or chemical
- direct - mechanical : direct compression pressures from structures or motions is place on spinal nerve(s)
- indirect - mechanical: blood flow decreases (ischemia) to the spinal nerve from direct pressure (compression or stretch) or from scar tissue formation around nerve tissue
- direct - chemical: nuclear material from herniated intervertebral discs encroaches space
- indirect - chemical: ongoing cellular inflammatory responses with tissue edema
- Compression can be due to stenosis in the central canal or foramen by bony and/soft tissue changes, tumor, or disc bulge/herniation
- Associated signs and symptoms: Numbness (sensory n.), weakness (motor n.), muscle atrophy, impaired deep tendon reflexes, sensory changes in affected nerve root distribution
Sciatica
Sciatica is a radicular condition associated with pain in the low back and lower quarter,specifically pain that extends down the posterior lower leg, including the foot. It is typically unilateral, but can present bilaterally. It is most commonly caused by intervertebral disc herniation, and is also associated with degeneration, infection, stenosis, and pelvic instability. Patient who have increase pressure on the sciatic nerve due to pregnancy, posterior hip/buttock trauma, or inflammation of the piriformis muscle may also report sciatica symptoms
- sharp, dull, burning or radiating pain often associated with numbness and parasthesias
- may include weakness and loss of reflexes
- L4: patellar reflex, medial sensation
- L5: dorsiflexion, lateral sensation
- S1: Achilles reflex, plantar flexion, posterior sensation
- aggravated by coughing, sneezing, valsalva
- movement is generally guarded and stiff, especially in the trunk and affected hip
- Cauda Equina Syndrome: considered a surgical emergency
- sudden change in bowel/bladder function (urinary retention, loss of sphincter control) or
- sudden loss of sensation in the perineum ("saddle anesthesia")
- bilateral sciatica symptoms
- treatment is typically conservative with PT x 6-12 weeks with follow-up MRI/CT if there is no improvement; epidural steroid injections can be helpful for symptom reduction.
Intervertebral Disc Conditions
Although disc herniation can result in pressure on the nervous system tissue, either from direct contact or from chemical irritants from inflammation, a majority of these cases resolve over time with conservative treatment. The evidence for long-term relief with surgery is mixed, with exceptions for situations that markedly reduce strength and sensation.
- Disc structure allows for distribution of force during weight bearing through the spine during static posture and during spine motions in multiple planes
- Foraminal disc herniations are the most symptomatic
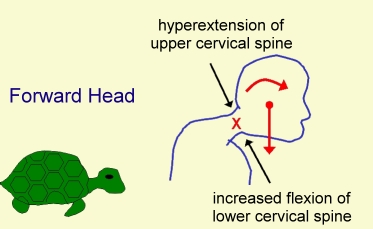
- Degenerative changes increase in the cervical spine with postural imbalances, primarily forward head
- Degenerative changes increase in the lumbar spine with repetitive compression (e.g. heavy lifting in flexion) or trauma (e.g. fall); degenerative changes may be asymptomatic
- Nucleus pulposus desiccates over time, decreasing its ability to absorb and distribute weight bearing and rotational forces; age-related change; disc rehydration occurs during sleep and recumbent positions Increased calcification, fracture risk, and decreased density at vertebral end-plates The affected nerve root is between spinal levels (e.g. C5-6 involves C5 nerve root)
- Annulus fibrosis can tear, resulting in decreased resistance to torque and increased risk of extrusion of disc contents; risk of herniation of nucleus pulposus increases with annular tears
- Annular tears usually occur posteriorly where the annulus is weakest; herniation may be central, posterior, or posterior-lateral (e.g. foramen).
- Discs may bulge without evidence of annular tearing or herniation
- Most common site of disc herniation is
- C5-6
- C6-7
- L4-5
- L5-S1
- in the cervical spine, the greatest amount of flexion motion occurs at C5-6
- in the lumbar spine, the lower segments are more vulnerable because the posterior longitudinal ligament ends at L3.
Spinal Stenosis
Stenosis refers to a narrowing in the central canal or associated spinal foramen due to degeneration of bony structures and ligaments. Space within the canal/foramen changes with spinal motions:
- flexion --> central canal widens
- extension --> central canal narrows
Cervical signs and symptoms->decreased strength and dexterity in hand, decreased grip function, pain, numbness in hands, potentially impaired balance/gait
Lumbar signs and symptoms -> pain (affected side or bilateral), numbness and LE weakness
Neurogenic claudication describes pain that results from ischemic compression on the nerve root, producing signs and symptoms in the legs with prolonged standing/extension and is relieved with lying down or sitting (flexion). There is increased pain with walking down inclines due to increased lumbar extension
![]()
 Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. / CC BY 3.0
Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. / CC BY 3.0
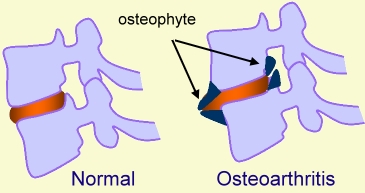
Osteoarthosis
- usually appear at the uncovertebral and/or facet joints
- osteophytes are one of the space-occupying lesions which may lead to radiculopathy
- spondylosis is used to describe osteoarthosis in the spine at the margins of the vertebral bodies
Facet Joint Pathology
Facet joint pathology is a type of osteoarthrosis in the spine. It is a degeneration at the facets that results in bone spurring or related changes to bone tissue. Symptoms include:
- painful restricted motion
- in the cervical spine, pain is typically provoked with combined motions of extension, side bending and rotation
- achiness which may radiate into the shoulder (cervical) or lower leg (lumbar)
- complaints of the lumbar area clicking, locking or "going out"
![]()
 Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. / CC BY
Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. / CC BY
Spondylolysis and Spondylolisthesis
Spondylolysis
Fracture of the pars interarticularis (segment of bone between the superior and inferior articulating facets)
In the image below, notice how the spinous process has separated from the lamina. Result is instability at the affected segment and abnormal weight-bearing forces in adjacent spinal segments. You should notice how the vertebra translates forward in the sagittal plane with respect to adjacent vertebra. This can occur with repetitive forces and due to some forceful impact in extension, such as hopping and landing on one foot with force
Spondylolisthesis
Mostly a condition of the lumbar spine which is associated with chronic, repetitive trauma. Instability of longitudinal ligaments from repetitive force or excessive motion causes the segment to move anteriorly or posteriorly. Anterolisthesis is most common and may require surgical fusion to prevent further instability or loss of nerve function.