Osteoarthritis (OA)
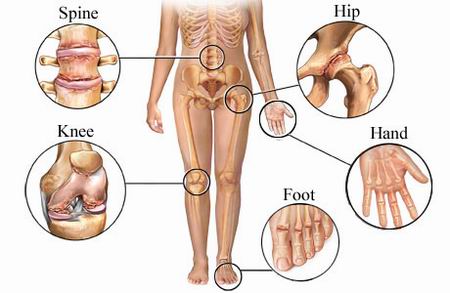
A chronic, degenerative disorder primarily affecting the articular cartilage of synovial joints, with eventual bony remodeling and overgrowth at the margins of the joint.
Background and Characteristics
- Refers to degeneration and inflammation of bone and cartilage in articulating (moving) areas
- Pain with weight bearing and joint motion can progress into partial to full loss of motion and pathological fusion (ankylosis)
- Osteophytes (bone spurring) may be identified on x-ray or diagnostic imaging. They can form in response to abnormal joint stresses
- http://www.medical-look.com/Joint_pain/Osteoarthritis.html
- Pathological bone remodeling can lead to ligamentous laxity and joint hypermobility/instability
- Can result in secondary nerve or postural dysfunction due to loss of joint height/space
- Symptoms are exacerbated with overuse, weather changes, or prolonged immobilization
- Associated with advancing age and family history (primary OA), lifestyle habits (sedentary, obesity, high-impact sports, repetitive loading/lifting), prior fracture or injury, and loss of bone density (secondary OA)
Signs and Symptoms
- pain - localized and referred
- impaired joint mobility (typically a capsular pattern)
- firm end-feel indicates chronic presentation
- guarded end-feel indicates acute presentation
- includes effusion and/or crepitus
- loss of accessory joint motion
- impaired muscle performance
- muscle length-tension relationships
- inadequate activation or guarding of postural stabilizers
- impaired balance
- joint degeneration limits feedback from proprioceptors
- functional limitations
- may need adaptive equipment to complete a functional activity or to protect joint(s) from further injury
Principles of Management of Osteoarthritis
- Patient instruction
- Pain management—early stages
- emphasis is on reducing joint stiffness, balancing activity and rest, and reinforcing the role of movement in joint health
- Pain management—late stages
- consider modalities for home use, pacing and prioritizing, modifying activities
- Assistive and supportive devices and activity
- bracing, aquatics, assistive devices for ADLs, home and environmental modifications
- Resistance exercise
- emphasis is on strengthening within non-painful ranges, isometrics to minimize disuse atrophy
- open chain activities with resistance across long lever arms can increase joint loads and exacerbate arthritis symptoms
- Stretching and joint mobilization
- assisted and patient instruction in safe and effective technique
- involved joints typically have a firm end-feel due to bony changes in the articulating areas
- Balance activities
- Aerobic conditioning
- patient education on exercise parameters, including low impact-low joint stress activities