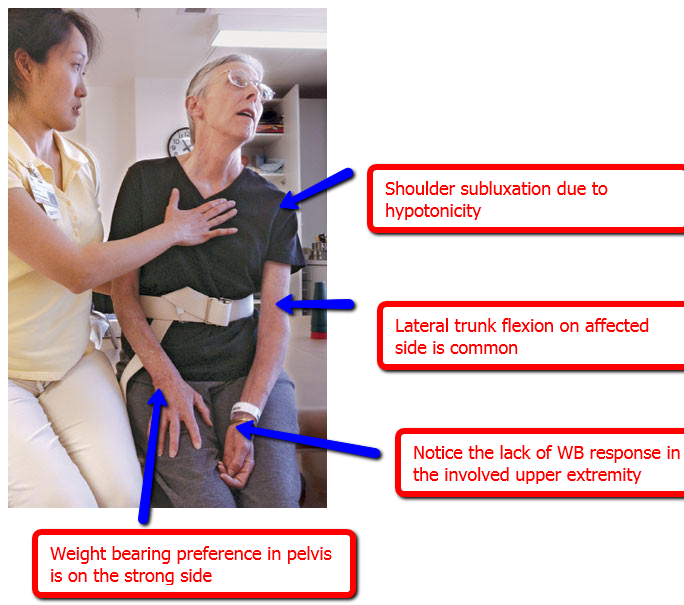
Clinical Decision-Making Practice
How could this therapist use Fell's framework and manual facilitation interventions to progress this patient's
- Attention to the L side during functional sitting task?
- Functional use of the L side (limbs and trunk)?
- Postural alignment in static sitting?
http://assets.bizjournals.com/story_image/112502-0-0-2.jpg
Positioning and Shoulder Pain Management
A significant percentage of patients develop some form of shoulder pain following stroke.
Downward scapular rotation and rotator cuff weakness due to loss of motor control on the affected side leads to subluxation of the glenohumeral joint. Pain can result from prolonged stretch, shoulder impingement from malalignment, adhesive capsulitis from loss of active or regular range of motion.
Over time, repeated microtrauma can result in severe pain throughout the limb: Complex Regional Pain Syndrome.
Signs and symptoms of CRPS include: red and swollen hand, cool hand/limb or change in temperature, shiny skin and increased sweating, thenar and hypothenar atrophy
Interventions to minimize shoulder pain
Support a flaccid arm at all times: pillows in bed, wheelchair lap tray, UE sling/hemi sling
Maintain glenohumeral external rotation
Maintain scapular mobility on the thorax
manual scapular ROM
PNF techniques in multiple directions with scapular facilitation
Avoid
passive or active shoulder movements beyond 90 degrees unless the scapula is gliding toward upward rotation and sufficient external rotation is available.
pulleys: they may cause impingement
Educate family members and nursing staff in use of positioning and protective strategies; proper transfer techniques to prevent pulling or lifting on affected limb
Positioning
|
Supine and sitting |
scapula protraction & slight abduction with neutral GH rotation; humerus is supported |
toc | return to top | previous page | next page