Treatment - Clinical Application
Approximately 6 minutes
When selecting electrical stimulation, a therapist must select a device and an application that will support achieving the desired effect. Common goals that may be achieved with including electrical stimulation into the treatment include:
- improving muscle performance and strength
- decreasing or alleviating pain
- improving blood flow
- decreasing or controlling edema
- facilitating tissue healing
Application Decision-Making
The physical therapist will screen each patient for contraindications. Precautions are conditions to consider when selecting and applying electrical stimulation
Contraindications
- Pregnancy - except during labor for pain control
- Pacemaker or other cardiac implants for interference
- Cancer - risk metastasis
- Location of thrombophlebitis or phlebothrombosis for risk of embolism
- Active Tuberculosis
- Over carotid sinus
- Area of active hemorrhage
- Cognitive Impairments - unable to follow directions or provide feedback
Precautions
- Obesity - insulator
- Absent or diminished sensation
- Skin conditions - eczema, psoriasis, acne, dermatitis, infection, allergies to gel or tape
- Diabetes - fragile thin skin
- Peripheral neuropathies or areas of denervation
- Metal - internal or external
- Range of Motion or exercise limitations
- Spinal Cord Injury - dysreflexia
There are times when a Physical Therapist may decide to use a modality that is normally contraindicated after discussion with the patient's physician. For example, a patient with a history of cancer in the distant past or application of the modality at an extremity away from the cancer site may not pose more risk than benefit.
Estim Parameters
Electrical stimulation parameters are intentionally selected to produce the desired effect. Electrical stimulation parameters are frequency, duty cycle, ramp time, and duration. For direct current and monophasic pulsed current, the active electrode is set for a positive or negative tissue charge.
Frequency - number of electrical pulses delivered to the body in one second
- Also called pulses per second (pps), Hertz (Hz) with AC
- Higher frequencies cause higher levels of muscle fatigue due to less time between bursts/pulses
- Impedance decreases when frequency increases
- Frequencies of 1-120pps meets most therapeutic goals
- Stimulation at 50pps tends to be more comfortable than 35pps
- Classified as low, medium, and high in clinical units:
|
low |
medium |
high |
|
<= 1 kHz "microcurrent" |
1-100kHz IFC, Russian, LIDC |
>100kHz TENS, HVPS |
Duty Cycle - percentage of on time to total time between pulses
- Current flows during 'on time' and ceases during 'off time'
- Percentage of on time divided by the sum of the on and off time
- Example, on time is 5 seconds, off time is 20 seconds = 1:4 ratio or 5 sec/(5+20sec) = 20%
- Clinically speaking, muscle contractions elicited through electrical stimulation are more fatiguing, so longer off time allows for recovery/rest and fends off fatigue.
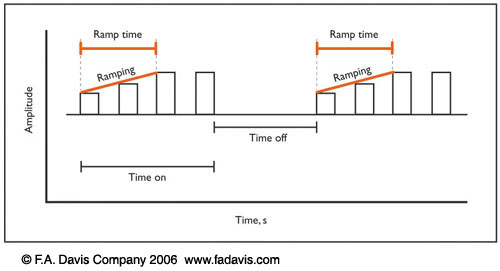
Ramp Time - the time it takes to increase wave amplitude to its peak amplitude
- Fixed on some commercial machines, ranging from 1 - 8 seconds
- 2 second ramp up is often adequate for comfort
- Slow rise times can allow a tissue to accommodate to a stimulus
- Ramp down or off can increase patient comfort and provides opportunity to actively hold a contraction after the stimuli has ended.
Duration - the total time providing electrical stimulation. Treatment times can range from 10 to 45+ minutes
This table provides a summary of conditions that may be treated effectively with electrical stimulation.
Key point: You will find variations in the literature about parameters with respect to pulse frequency, pulse duration, and duration. For this reason, you will not be teste on pulse frequency or pulse duration or duration. In clinical practice, you will consult the literature and use observation, patient feedback, and measures to inform your effectiveness.
|
Indication |
Type |
Waveform |
Pulse Frequency (pps) |
Pulse Duration (µS) |
Intensity |
Duration |
|
Muscle strengthening |
NMES |
AC, Russian
|
50-80 |
200-800 |
to 60&-70& max voluntary contraction |
10-20 strong contractions |
|
Contraction for function |
FES |
AC, Russian |
20-60 |
200-800
|
to the desired effect |
task specific |
|
Pain Modulation |
High frequency TENS |
pulsed AC or DC |
>50; generally 80-110 |
50-100 |
to perception of stimulus; no motor response |
20-30+ minutes |
|
|
Low frequency TENS |
pulsed AC or DC |
<10 |
> 150 |
to point of visible muscle twitch |
20-45 minutes |
|
|
Hyperstimulation |
DC or pulsed DC |
(High) 100 (Low) 1-5 |
250. up to 1 second |
to highest tolerated painful stimulus |
30-60 seconds each area |
|
Edema Management (acute) |
Sensory stim |
pulsed DC |
100-125 |
2-100 |
to comfortable sensory threshold; just below motor response |
20-45+ minutes |
|
Edema Management (subacute/chronic) |
NMES |
AC, Russian |
20-80 |
100-600 |
to tetanic muscle contraction |
3 seconds on: 3 seconds off x 10-20 minutes |
toc | return to top | previous page | next page