Acute and Persistent Pain
Acute pain is the symptom associated with how the brain interprets direct tissue trauma and the subsequent inflammatory response which initiates the tissue healing processes. Over time, as endogenous opiates have an effect and as tissue sensitivity decreases, injured tissue heals within 2 weeks to 3 months and function is restored. Acute pain is usually easily to localize (e.g, the patient can point to it or name a specific body part/structure/area).
Persistent pain is defined as:
- pain lasting longer than 3 months
- etiology may be unknown or persistent (e.g., history of whiplash, degenerative condition)
- can result in abnormal movement patterns due to protective responses and nerve sensitization
Common causes of recurrent or persistent pain:
- overuse, repetitive strain, or trauma
- reinjury
- length-strength imbalance
- excessive tissue tension or tissue weakness
- insufficient recovery time
- training errors
- hypertrophic scarring
- poor blood supply
Psychosocial impact of persistent pain are significant and can lead to disability. Unrelenting pain sensations can result in chemical changes which impact appetite, mood, mobility, body system function, sleep, libido, and participation in work/social life. Patients who are unable to adequately manage persistently painful conditions may lose employment and strain family relationships. Individuals with persistent pain are at higher risk for depression and addiction disorders.
The role of the PT and the PTA in the treatment of persistent pain is to be an active participant in a multidisciplinary team that guides pain management. Cardiovascular endurance, pacing and prioritizing, body mechanics and posture, counseling and imagery/cognitive behavioral therapy (CBT), nutrition, stress management, and medication management comprise best practices for persistent pain management.
Pain Medication Overview:
- NSAID = Non-steroidal anti-inflammatory drugs. Non-narcotic. Ibuprofin is included in this class. Prolonged use may result in gastrointestinal irritation and decreased kidney function
- ASA= acetylsalicylic acid. Non-narcotic. ASPIRIN
- Acetaminophen = centrally-acting analgesic. Non-narcotic. Tylenol is the brand name.
- Opioids = centrally acting analgesic for severe pain. CNS depressant. Effects can be short or long-acting. Hydrocodone and morphine are included in this class
Pain Qualities
Subjective reports of pain include a description of the pain quality. Pain descriptions may provide some insight into level of acuity and the involved structures. It is important to know that people who persons persistent pain may report a multiple and fluctuating descriptions of somatic (felt in the body) pain, without any evidence of recent tissue trauma.
A PTA must be able to make comparisons in subjective reports of pain quality and decide if interventions should be modified or discontinued based on the patient response. Marked changes in pain presentation and quality may require consult with the supervising physical therapist.
Watch and listen to "Christina describes pain qualities"
|
Pain Quality |
Associated Involved Structure* |
|
cramping, dull, aching |
muscle |
|
sharp, shooting |
nerve root |
|
sharp, burning, lightning-like |
nerve |
|
burning, pressure-like, stinging, aching |
sympathetic nerve |
|
deep, nagging, dull |
bone |
|
sharp, severe, intolerable |
fracture |
|
throbbing, diffuse |
vasculature |
Spinal Levels and Referred Pain
- pain can be localized to one or more spinal levels, particularly when there is localized inflammation, compression, degeneration, or stretch trauma to nerves and/or surrounding tissue
-
pain can also perceived in one area while being generated from a distant structure
- spinal nerves are organized into plexi, which allows multiple spinal levels to share innervation with a target tissue.
- Active Learning Exercise - using your text as a resource, categorize spinal plexi into levels, and predict outcomes and pain presentation due to inflammation or compression on each plexus. What will the patient complain of? What potential impairments or functional losses might you expect?
|
Plexus |
Spinal Levels |
Example Signs and Symptoms |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
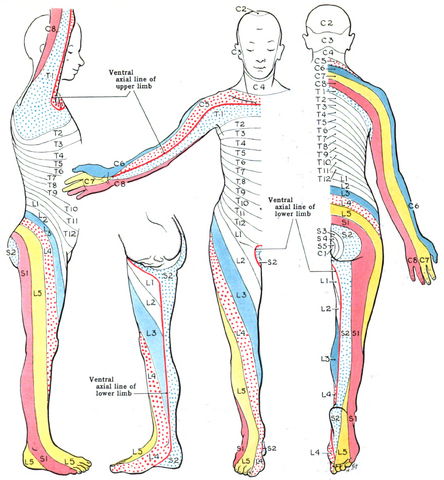
- pain originating from the spine or peripheral nerves may follow predictable patterns of sensory nerve distributions, called dermatomes; persistent pain conditions may also present in dermatome patterns due to nervous system sensitization
- radiating pain or paresthesia may indicate irritation of spinal level nerve roots - spinal nerve roots are generally at a higher risk for injury, as they lack protective perineurium and epineurium connective tissue coverings
- parasthesias can be caused by: ischemia (inadequate blood supply), obstruction, compression, infection, inflammation, and degenerative conditions
"Grant 1962 663" by Grant, John Charles Boileau - An atlas of anatomy, / by regions 1962. Licensed under Public domain via Wikimedia Commons - http://commons.wikimedia.org/wiki/File:Grant_1962_663.png#mediaviewer/File:Grant_1962_663.png
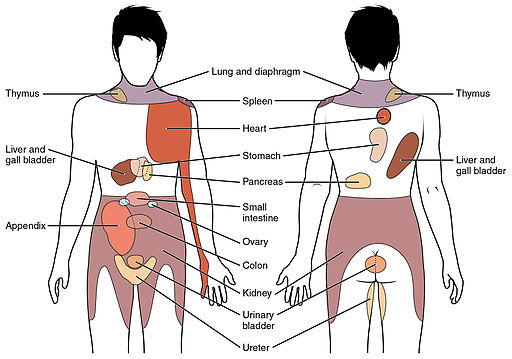
- body organs can refer pain to spinal levels from which their respective pain nerves originate from.
- for example, pain in the heart muscle (angina) can refer to the sternal area (T1-5 sensory nerve roots)
By OpenStax College [CC-BY-3.0 (http://creativecommons.org/licenses/by/3.0)], via Wikimedia Commons
 |
Solve the crossword puzzle. |
|
This content requires JavaScript enabled.
|
|