Neuromuscular Pathology
Implications for Clinical Decision-Making
- Communication of dysfunction and observations depends on a mutually understood vocabulary between health care providers
- PTAs are more effective in planning and patient communication when terms used in a PT evaluation report are understood
- Understanding disease presentation and progression increases relevance of tests, measures, and interventions, area of concern in discharge planning, equipment management, communication, and home safety
Sources of Neuromuscular Pathology
- Impaired circulation (embolic ("clot") or hemorrhagic ("bleed")
- Disease of brain cells (degenerative)
- Disease at the neuromuscular junction
- Trauma (traumatic brain injury, spinal cord injury, peripheral nerve injury)
- Idiopathic (unknown origin)
Common Pathology Classes
|
Class |
Description |
Risk Factors |
Common Symptoms |
Examples |
|
Upper Motor Neuron Disease |
Lesions in descending motor tracts Includes the cerebral cortex, internal capsule, brainstem, and spinal cord |
Hemodynamic compromise Diabetes Cardiovascular disease Advanced age Closed head injury Arteriovenous malformation |
Weakness of many involved muscles Hypertonicity (increase in muscle tone) Hyperreflexia (exaggerated responses of spinal reflexes) Pathological reflexes Spasticity |
Cerebral Vascular Accident (CVA) ("stroke")
Cerebral Palsy Spinal Cord Injury Multiple Sclerosis |
|
Lower Motor Neuron Disease |
Lesions involving nerves and axons at or below the alpha motor neurons |
Under investigation Suggested linkages include genetic and environmental triggers |
Weakness of single or multiple involved muscles Hypotonicity (decrease in muscle tone) Fasciculations (small, local, involuntary contractions) Muscle atrophy Decreased or absent reflexes |
Amytrophic Lateral Sclerosis (ALS) Myasthenia Gravis Guillian-Barre Syndrome |
|
Disorders of the Basal Ganglia |
Lesion of specific deep nuclei (centers) in the brain Characterized by either 1) large involuntary movements (dyskinesias) or 2) abnormal static postures (akinesias) |
Under investigation. Hereditary factors; Long-term use of anti-psychotics |
Dyskinesias Resting tremor Athetosis (slow, involuntary, writhing, twisting movement) Chorea (involuntary, continuous, rapid, irregular and jerky movements) Akinesias Rigidity (resistance to passive movement of the limb) Dystonia (involuntary adoption of abnormal postures) Bradykinesia (decreased amplitude and velocity of movement; slowed movements)
|
Parkinson's Disease Huntington's Disease Hemiballismus |
|
Disorders of Cerebellum |
Lesion in the cerebellum |
Much like CVA risk factors Congenital malformation Genetic contributors |
Changes are ipsilateral (same side) Ataxia Dysmetria Dysdiadochokinesia Hypotonia Speech changes
|
Cerebellar stroke Ataxia disorders |
|
Peripheral nerve disorders |
Localized or diffuse trauma to the nerve structure |
Repetitive use Traction (stretching forces) from trauma Difficult birth Prolonged compression |
Weakness in select muscle groups Atrophy Persistent pain |
Carpal tunnel syndrome Tarsal tunnel syndrome |
Ischemic Versus Hemorrhagic Injury
|
Ischemic |
Hemorrhagic |
|
Most common (about 80% incidence) |
Less common |
|
Caused by emboli or arterial narrowing |
Caused by rupture of vessels
|
|
Damage follows vascular distribution
|
Damage can extend into multiple vascular territories
|
|
Symptoms of stroke develop and worsen over time
|
Symptoms are usually sudden
|
|
Warning symptoms (changes in vision, balance, cognition, speech) often precede ischemic stroke |
Warning symptoms (vomiting, severe headache, impaired consciousness) often precede hemorrhagic stroke |
|
Impairments are somewhat predictable |
Impairments will vary with the individual and size
|
R CVA impairments versus L CVA impairments
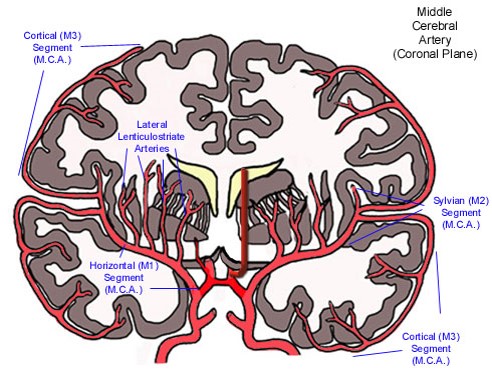
Most CVAs occur due to a blockage or bleeding in the middle cerebral artery. The vessel in red illustrates the distribution of the middle cerebral artery and its respective branches.
Common characteristics of cerebral CVA are:
|
Right CVA |
Left CVA |
|
L sided paresis (neurological weakness)
|
R sided paresis (neurological weakness)
|
|
Decreased attention span selective awareness of the environment or responsiveness to a stimulus or task without being distracted by other stimuli
|
Decreased initiation of tasks
|
|
Decreased awareness and judgment
|
Decreased R and L discrimination
|
|
Memory deficits
|
Dysphagia - impairment of strength and coordination of chewing and swallowing
|
|
L hemianopsia - loss of left half of the visual field
|
R hemianopsia - loss of right half of the visual field
|
|
L inattention
|
Increased frustration
|
|
Decreased abstract reasoning
|
Apraxia - inability to perform skilled purposeful movements
|
|
Emotional lability
|
Aphasia - inability to produce functional (expressive) or integrate (receptive) speech
|
|
Impulsivity
|
Compulsive behavior
|
|
Decreased spatial orientation
|
|
Arteriovenous Malformation (AVM)

 |
Click below the question to view the answer. |
|
This content requires JavaScript enabled.
|
|
- Disorganized collection of abnormally thin dilated blood vessels in the brain
- Directly shunts arterial blood into the venous system
- Result in increased pressure within the AVM and risk for hemorrhagic stroke
- Signs and symptoms include seizures, HA,dizziness, syncope, aphasia, motor and/or sensory deficits
Traumatic Brain Injury
- Primary cause of death and disability in children and young adults
- Greater incidence in males (3:1)
- Child abuse accounts for the majority of TBI cases in children
- Primary causes of TBI in general population
- MVA (motor vehicle accidents)
- Falls
- Violence
- Sports-related injuries
- Coup-Contracoup describes the mechanical forces on the brain as it strikes the inside of the skull as a result of high velocity impact
- Service-related TBI doubled between 2005 and 2011, largely from blast exposures and active and reserve-related duty (CDC, 2013)
- Glasgow Coma Scales and Rancho Los Amigos Scales and provide global assessment of cognitive functioning upon injury and during recovery respectively
Secondary Effects of Traumatic Brain Injury
- Swelling
- Bleeding
- Hypotension
- Respiratory complications
- Hypoxia
- Neuronal damage and death (diffuse axonal injury)
- Increased intracranial pressure


