Spinal Disorders
Radiculopathy
- Spinal nerve / nerve root conduction is impeded due to "encroachment into peripheral nerve tissue spaces resulting in nerve compression or ischemia";
- encroachment can be classified as direct or indirect, mechanical or chemical
- direct - mechanical : direct compression pressures from structures or motions is place on spinal nerve(s)
- indirect - mechanical: blood flow decreases (ischemia) to the spinal nerve from direct pressure (compression or stretch) or from scar tissue formation around nerve tissue
- direct - chemical: nuclear material from herniated intervertebral discs encroaches space
- indirect - chemical: ongoing cellular inflammatory responses with tissue edema
- Compression can be due to stenosis in the central canal or foramen by bony and/soft tissue changes, tumor, or disc bulge/herniation
- Associated Signs and Symptoms: Numbness (sensory n.), weakness (motor n.), muscle atrophy, impaired DTR, sensory changes in affected nerve root distribution
Sciatica
- sharp, radiating pain often associated with numbness and parasthesias
- weakness and loss of reflexes
- L4: patellar reflex, medial sensation
- L5: dorsiflexion, lateral sensation
- S1: Achilles reflex, plantar flexion, posterior sensation
- aggravated by coughing, sneezing, valsalva
- most-commonly caused by herniated disc
- Cauda Equina Syndrome: considered a surgical emergency
- sudden change in bowel/bladder function (urinary retention, loss of sphincter control) or
- sudden loss of sensation in the perineum ("saddle anesthesia")
- bilateral sciatica symptoms
- treatments is typically PT x 6 weeks with follow-up MRI/CT if there is no improvement in symptoms

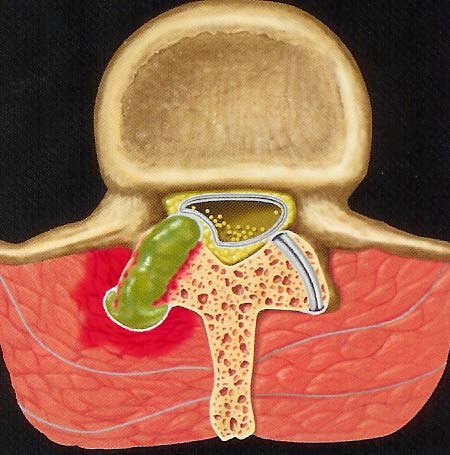
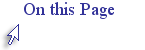
Intervertebral Disc Disease
- Disc structure allows for distribution of force during weight bearing through the spine
- Reinforce your understanding of spine kinesiology by
- reviewing the animation on the Vertebra and Discs
- you will be taken to a Web page on the Normal Spine and from there you need to click on the Vertebra and Discs link to view the animation
- Disc structure allows for complex spinal motions in multiple planes
- Degenerative changes increase with repetitive compression (e.g. heavy lifting in flexion) or trauma (e.g. fall); degenerative changes may be asymptomatic
- Annulus fibrosis can tear, resulting in decreased resistance to torque and increased risk of extrusion of disc contents; risk of herniation of nucleus pulposus increases with annular tears
- tears usually occur posteriorly where the annulus is weakest
- Discs may bulge without evidence of annular tearing or herniation
- Most common site of disc herniation is
- C5-6
- C6-7
- L4-5
- L5-S1
- foraminal disc herniations are the most symptomatic

Watch this video on lumbar disc herniation to reinforce concepts from your Cameron text
- Nucleus pulposus desiccates, decreasing its ability to absorb and distribute weight bearing and rotational forces; age-related change
- Increased calcification, fracture risk, and decreased density at vertebral end-plates
- The affected nerve root is between spinal levels (e.g. C5-6 involves C5 nerve root)
Spinal Stenosis
- Narrowing of the spinal canal or associated spinal foramen due to degeneration such as
- Stenosis progression can lead to specific motor and sensory deficit patterns:
- central cord syndrome: motor and sensory changes are primarily in the upper extremities
- Brown-Sequard syndrome: ipsilateral weakness, contralateral sensory deficits
Watch this video on spinal stenosis to reinforce concepts from your Cameron text
- Space within the canal/foramen changes with spinal motions:
- flexion --> central canal widens
- extension --> central canal narrows
- What therapeutic exercises will decrease compression to nerves affected by central canal stenosis?
- Signs and symptoms of spinal stenosis
- Cervical ->decreased strength and dexterity in hand, decreased grip function, pain, numbness in hands, potentially impaired balance/gait
- Lumbar -> pain (affected side or bilateral), numbness and LE weakness
- neurogenic claudication = pain in B LEs increasing with prolonged standing/extension and is relieved with lying down or sitting (flexion); increased pain with walking down inclines (due to increased lumbar extension)
- What postural adaptations can you expect from a patient with severe lumbar spinal stenosis?
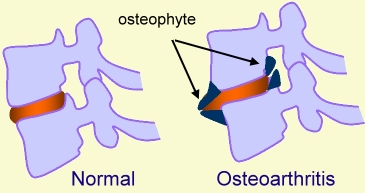
Osteoarthosis
- usually appear at the uncovertebral and/or facet joints
- osteophytes are one of the space-occupying lesions which may lead to radiculopathy
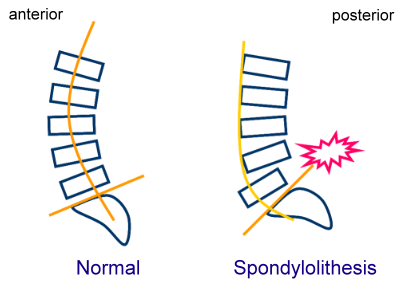
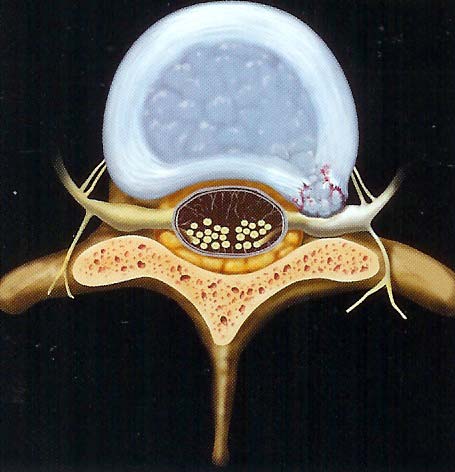
Spondylolysis and Spondylolisthesis
Spondylolysis
Fracture of the pars interarticularis (segment of bone between the superior and inferior articulating facets)
Can occur with some forceful impact in extension (hopping/landing on one foot)
Result is instability at the affected segment and abnormal weight-bearing forces in adjacent spinal segments
Vertebra translates forward in the sagittal plane with respect to adjacent vertebra
Spondylolisthesis
Mostly a condition of the lumbar spine which is associated with chronic, repetitive trauma
Mostly involves and anterolisthesis of the affected segment
May require surgical intervention/posterior fusion to prevent further instability or loss of nerve function
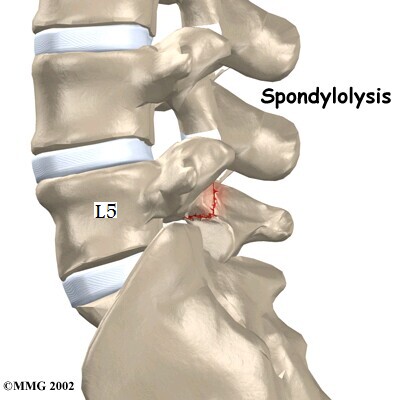
Ankylosing Spondylitis
An inflammatory condition of unknown etiology which initiates as inflammation in the sacral region. It results in progressive loss of spinal motion due to progressive inflammation and vertebral fusion.
Whiplash-Associated Disorders (WAD)
Refers to bony and/or soft tissue injury in the cervical spine and upper quarter due to acceleration-deceleration forces
Injury is to ligaments and muscles; stretch forces to neuromuscular structures may account for increase sensitization
Symptoms of WAD include:
- pain
- headache
- decreased spinal mobility
- stiffness
- low back pain
- shoulder pain
- visual disturbances
- dizziness
Classification of WAD
- Grade I: No physical signs of musculoskeletal dysfunction; subjective reports of pain, stiffness, and tenderness
- Grade II: Some physical signs of cervical movement dysfunction; subjective symptoms reported
- Grade III: Physical and neurological signs of cervical dysfunction; subjective symptoms reported
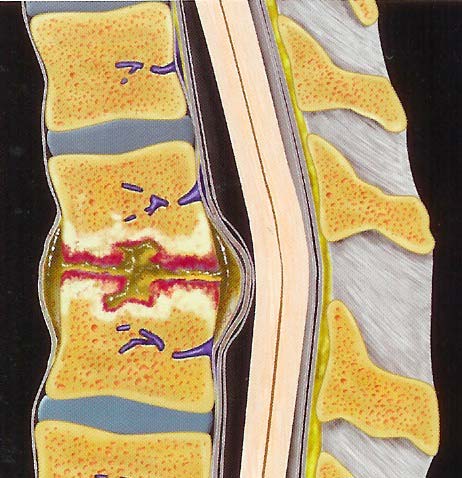
Discitis / Osteomyelitis
- Infection of the vertebral bodies and intervening discs
- Typically not observable in a x-ray during the early stages
Malalignment
- forward head (turtle neck)
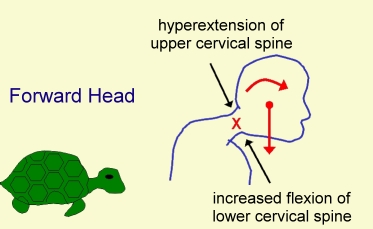
- hyperflexion of lower cervical spine
- hyperextension of upper cervical spine
Self-Assessment
Prepare for the test by checking your understanding of spinal disorders
return to top | previous page | next page