Balance Overview
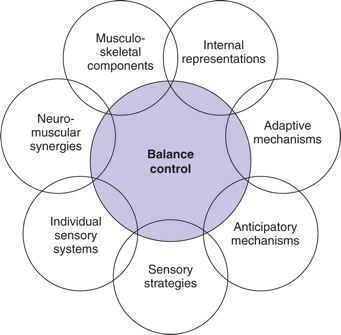
There are multiple models for looking at the role of systems in maintaining balance
Motor Control: Theory and Practical Applications,ed 2, Philadelphia, 2001, Lippincott Williams & Wilkins.
Balance is complex.
Balance control includes continuous coordination of sensory, motor, and cognitive systems. Selecting balance interventions, and measuring the effect of these interventions, is a fundamental skill for the PTA.
Balance impairments can result from pathologies and injuries that effect central nervous system processing. Altered sensation processing from the senses and periphery can influence motor planning, motor control, and motor responsiveness. Effective treatment of balance disorders is dependent on determining the cause of the impaired balance. Let's say this again, because this is IMPORTANT!
Effective treatment of balance disorders is dependent on determining the cause of the impaired balance
Contributors can be musculoskeletal, neuromuscular, sensory, or cognitive, or some combination. Unsteadiness, dizziness, and loss of balance is often attributed to disorganization or conflicting information from the sensorimotor system.
Stages of Information Processing
- Somatosensory - includes proprioception, kinesthesia, pain, temperature, vibration, sharp/dull, etc.
- Visual and Vestibular - includes references of head and eye position and spacial orientation, including speed of position change to maintain effective gaze
- Sensory Motor Integration - processes of integrating multiple inputs to resolve conflicts between systems
- Motor Output Generation - selecting automatic, well-learned, or generating new responses to produce a response resulting in efficient movement and balance control
Updated Evidence
Fay Horak and colleagues at OHSU have studied balance extensively, and developed an alternative schema for looking at balance control. They have identified six categories that influence balance. These include:
- biomechanical constraints (limitations from the physical body)
- stability limits - verticality (how far can you lean without taking a step?)
- anticipatory postural control (what needs to happen before you change positions?)
- postural responses (can you recover efficiently and effectively when there is a perturbation?)
- sensory orientation (what are your senses - (vision, vestibular, proprioceptive, perceptual) telling you?)
- stability in gait (can you walk safely, and more importantly, can you walk and do other things, too?)
Balance And Function
There are three primary categories of balance control during functional activities: static, dynamic, and automatic postural reactions (Dutton, 249)
Automatic Postural Reactions
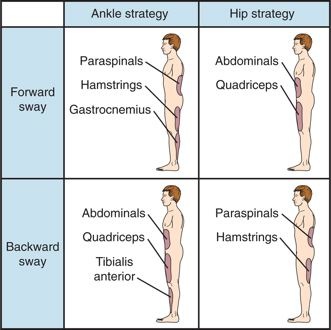
There are predictable balance strategies which are selected in response to a postural perturbations and/or loss of balance in order to prevent a fall.
- Hip strategy

- Characteristics:
- proximal to distal activation of muscles
- muscles activated on the side toward which COG is shifted or perturbed
- Typically elicited:
- during perturbations that are large in comparison with the supporting surface
- when the task requires a large or rapid shift in COG
- Appears only if vestibular reception is intact
- Ankle strategy

- Characteristics:
- distal to proximal activation of muscles
- muscles activated on side contralateral to direction that COG is shifted or perturbed ("elongation of the weight-bearing side"
- Typically elicited:
- during small shifts or perturbations of COG
- when the task requires maintenance of upright posture
- Appears only if somatosensory reception is intact
- Stepping Strategy
- Characteristics
- Limits of stability is reached or exceeded
- Muscles activate to allow a compensatory weight shift
- Typically elicited
- during large, gross perturbations
- Weight Shift Strategy
- Characteristics
- shifting from one leg or limb to the other
- Suspension Strategy
- Characteristics
- Lowers COG by quickly flexing knees
- Typically elicited
- During accelerations and momentum with perturbations (i.e. roller skating)
Primary Stabilizing Muscles for during Anterior/Posterior Postural Sway
Balance and Disability
Loss of balance and falls has a significant impact to older adults. An excellent resources for your future practice is the CDC progrram STEADI - Stopping Elderly Accidents, Deaths & Injuries
Statistics for related to falls in Oregon include:
- Falling is a major reason for hospitalization due to injury
- 50% of seniors hospitalized for falls are diagnosed with a hip fracture
- 8% of seniors hospitalized for falls are diagnosed with TBI
- Falls are the leading cause of TBI among Oregon seniors
- The rate of falls in seniors is one in three (33%). 20-30% of seniors who fall are injured as a result of the fall
Protect the Patient
Due to the high risk of injury when treating patients with impaired balance, best practices include setting up the treatment environment to challenge balance, but prevent injury from falls. This includes the use of a gait belt or harness, performing the exercises near a railing, and closely guarding the patient.