Neuromuscular Re-Education
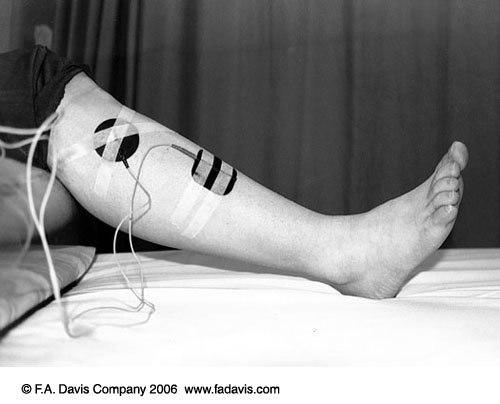
Neuromuscular electrical stimulation (NMES) is defined in Behrens as "the use of electrical stimulation for activation of muscle through stimulation of the intact peripheral nerve." Therefore, an appropriate patient candidate for NMES must have an intact, or at least partially intact, peripheral nerve for a positive response. The following outlines considerations for use of NMES.
Contraindications - Absolute
- Demand cardiac pacemaker due to possible electrical interference with signal
Contraindications - Relative
- Any type of cardiac pacemaker
- Pregnancy in the third trimester
- Broken or irritated skin at electrode site
Precautions
- Geriatric and cardiac patients need to be monitored for BP and HR
- Presence of superficial metal (i.e. external fixators, staples, and pins)
- Absent or impaired skin sensation
Considerations for use of NMES
- Two main concerns when planning a treatment with NMES
- quality of contraction of the activated muscle
- patient comfort related to compliance with plan
- Choice of Waveforms
- Symmetrical waveforms for large muscle stimulation such as the quadriceps
- Asymmetrical waveforms for smaller muscles such as those of the wrist flexors and extensors
- Intensity or Amplitude should be increased gradually for patient comfort and tolerance over a 15 minute period. The desired contraction may not be achieved on an obese patient due to adipose acting as an insulator, requiring the use of a high intensity, which may not be tolerated by the patient.
- Units with pulse duration between 200-400 milliseconds are more equipped for NMES use
- Strength-duration curve: low pulse duration takes a high amplitude to elicit a muscle response until >40 m sec
- Pulse rate = frequency, as pulse rate increases, so does rate of muscle firing resulting in a stronger contraction.
- To minimize fatigue, use lower pulse rate,
- Electronically generated muscle contractions recruit in reverse = larger superficial motor units FIRST in synchronous pattern
- Duty cycle = on time/(on time + off time); usually 1:3 or 1:5 ratio or 20-25%; off time is rest time for the muscle to recover before contracting again
- On time generally 2-10 seconds
- Ramp time is the gradual building to maximum current chosen; needs to be less than 1 second and less than the total on time
- Clinically, ramp down allows for patient confort and allows the patient to contract maximally and slowly lower the limb as the contraction
- Use length-tension relationship information: position limb with mild stretch on tissue for muscle contraction
- Visual feedback can enhance muscle control so position the patient to see the muscle movement during NMES treatment
Guidelines for Clinical Application
Strength and Endurance
- Originated with Russian Olympian training in 1976 reporting 10-30% increase in muscle strength using stimulation
- Can be used to supplement conventional exercise and units can be sent home with patient for use during HEP
- Choose electrode size and placement for a "balanced reaction" or full contraction without overflow or pulling into deviation
- Post neurological injury or surgery may leave a patient with difficulty initiating muscle contraction
|
Balanced Contraction |
Unbalanced Contraction |
|
|
|
See Behrens's text Box 10-3 on page 181 for patient home use instructions
Edema Reduction
- Leakage of blood cells and plasma proteins into interstitial space occurs after tissue trauma. Blood components are negatively charged and can be pushed from the area with negative polarity exposure.
- Elevate the extremity and use active range of motion for muscle pumping during treatment to enhance response to electrical stimulation
- Current should elicit brief but effective muscle contraction, frequency of 20-50pps
Orthotic Substitution
- Implanted functional electrical stimulation (FES) can be used on the lower extremity to control limb segments through a sequencing of muscle groups during a task such as ambulation.
Partial Denervation
- NMES can be used to retrain muscle after a peripheral nerve injury during the slow reinervation process.
- Return of function depends on degree of atrophy, mechanism and extent of injury, and time lapse since injury
Safety Considerations
- Equipment must be inspected regularly with documentation by professional
- Check patient medical history for any contraindication, precautions or changes since last treatment
- Skin checks BEFORE and AFTER modality - skin may be pink where the electrodes were placed due to increased blood flow but should subside in 30-60 minutes after treatment
- Cognitive issues - patient needs to be able to communicate sensation and follow direction. If cognitive impairment exists, electrical stimulation can still be administered if decided by the PT, however, extra care must be taken to monitor the patient.
Expected Outcomes
- Educate the patient and communicate about the goals of treatment for compliance, set realistic goals
Clinical Decision Making - Documentation
- Comprehensive examination
- Strength grades - isokinetic examinations
- Active ROM/Passive ROM measurements
- Edema and hypertrophy, girth measurements
- Gait description and movement patterns